Saddle Prosthesis
Kristy L. Weber
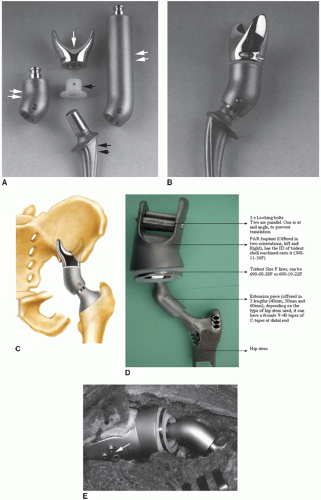
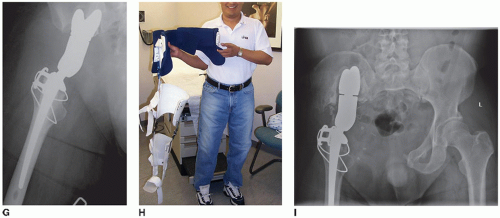
Saddle prosthesis reconstruction of a large acetabular/pelvic defect is a rare procedure with limited indications and substantial morbidity. This construct was originally designed for reconstruction in patients with large acetabular bony defects after total hip replacement with or without infection (Fig. 5.1). The most common current scenario is a patient with a primary or metastatic bone tumor located in the periacetabular region. Occasionally, it is still used in cases of massive bone loss after trauma or hip dysplasia or as a salvage procedure after failed hip reconstructive surgery. Resection types for pelvic tumors have been classified according to anatomic location (1). There are alternative reconstructive options after a Type 2 periacetabular resection that include a custom pelvic endoprosthesis, allograft-prosthetic composite hip reconstruction, iliofemoral arthrodesis or pseudarthrosis, ischiofemoral arthrodesis or pseudarthrosis, and flail hip. The benefits of a saddle prosthesis include stable limb reconstruction for early weight bearing, equal leg lengths, acceptable function, and relative ease of prosthesis placement compared to arthrodeses or allograft-prosthetic composites.
INDICATIONS
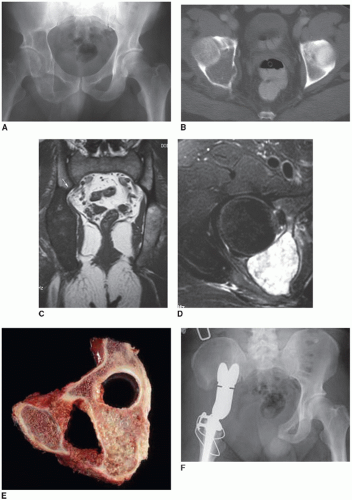
Periacetabular (Type 2 or Type 2/3) resection of a primary or metastatic bone tumor (Fig. 5.2) Salvage procedure after multiple hip revision surgeries with periacetabular bone loss
Periacetabular bone loss secondary to trauma
Periacetabular bone loss due to severe hip dysplasia
CONTRAINDICATIONS
Active pelvic infection within the operative field
Lack of substantial remaining ilium. The saddle prosthesis requires a stable, thick area of medial ilium for attachment to the pelvis; otherwise, there is a risk of iliac wing fracture through the thinner (lateral, superior) bone.
Lack of functional abductor muscles puts the patient at higher risk of dislocation.
Severe osteoporosis predisposes the ilium to fracture during weight bearing.
Patients receiving intensive chemotherapy may be at higher risk of infection.
Compromise of the lumbosacral plexus or femoral neurovascular bundle by tumor in addition to involvement of the acetabulum/hip joint is generally an indication for an external hemipelvectomy (hindquarter amputation).
No viable rectus abdominus musculature to fill the dead space if the iliopsoas or gluteal muscles are resected. This is a relative contraindication as free tissue transfer or local tissue rearrangement can also be used.
Extensive medical comorbidities that preclude a prolonged surgical procedure or predict a lifespan <3 months
PREOPERATIVE PREPARATION
Patient Expectations
Pelvic resections are challenging procedures with potential complications. Patients should be adequately counseled on the risks for their particular situation. There are several different periacetabular reconstructive options, and the risks and benefits of each should be described so that the physician and patient can make the best decision to balance function with potential complications. After a saddle prosthesis reconstruction, patients are usually able to fully bear weight after the soft tissues have healed, and their leg lengths should be equal. However, they may have a permanent limp and require assistive devices to ambulate if the hip flexors or abductors are compromised from the tumor extension. The known risks of this reconstruction (dislocation, infection, fracture, neurologic compromise, etc.) should also be clearly outlined.
Workup
A detailed history and physical examination are performed preoperatively with attention to pain, tumor stage, expected lifespan, neurologic status, gait, lower extremity strength, presence of signs of infection, inguinal adenopathy, and location of prior incisions/biopsy tracts. Plain radiographs and cross-sectional imaging of the pelvis are necessary. An MRI scan is helpful in situations where an adequate tumor margin needs to be achieved, as this will show the marrow and soft tissue extent of the disease. In a case of traumatic bone loss or a failed hip arthroplasty, a CT scan can better outline the bony structures in the pelvis. Adequate medial iliac bone is required to allow a stable fit of the saddle portion of the prosthesis and avoid a postoperative iliac wing fracture. Staging studies to assess the presence of possible metastasis are performed to better assess the anticipated lifespan or likelihood of cure. Preoperative laboratory tests include a complete blood count, protime/prothrombin time, electrolytes, and a type and cross for blood products. For a highly vascular metastasis (renal, thyroid), preoperative embolization should be considered to decrease blood loss. A formal preoperative bowel prep is used to minimize the chances of infection if the bowel is perforated during surgery.
Surgical Team
For the resection, ensure the availability of appropriate surgical services. Depending on the extent of tumor, other services may include urology, gynecologic oncology, vascular surgery, general surgery, and plastic surgery. If a primary bone tumor such as chondrosarcoma, Ewing sarcoma, or osteosarcoma invades the bladder or vaginal wall, it is necessary to partially resect these structures en bloc with the tumor to achieve an adequate margin. Often there is a plane between tumor and bowel, which is carefully dissected by the orthopedic or general surgeon. The benefit of the plastic surgery team cannot be underestimated, as a saddle prosthesis reconstruction creates a large devascularized dead space with frequent loss of part or all of the iliopsoas muscle.
This becomes a potential area for accumulation of a hematoma and subsequent infection. An ipsilateral or contralateral rectus abdominus flap is often rotated into the wound at the end of the case if the inferior epigastric vessels are maintained.
Equipment
There are several companies that currently make a saddle type of prosthesis (Link, Hamburg, Germany [1979] and Stryker, Mahwah, New Jersey). As of early 2011, the Stryker PAR process remains in the 510(k) approval process at the FDA. Review the specific technique considerations. Template the femoral side and determine the likely gap after resection in order to select the correct length of the curved body (base) component. The femoral component is placed with methylmethacrylate. Heavy sutures will help secure the saddle component to the ilium. For surgeons who use computer navigation for pelvic resections, the specific equipment should be ordered. A ureteral stent is placed in the operating room by the urology team to protect one or both ureters during the resection. A formal abduction brace is often used postoperatively to prevent early dislocation and is ordered in advance so that it can be placed on the patient at the end of the case.
Anesthesia Considerations
Often a pelvic resection and reconstruction can require many hours in the operating room depending on the extent of the tumor. The anesthesia team should be aware of this in advance to plan for additional venous access, arterial lines, and blood products.
TECHNIQUE
Positioning
The patient is placed in a sloppy lateral position on a beanbag or other support after vascular access catheters, endotracheal tube, urinary catheter, and ureteral stent(s) are inserted. If there is a possibility of a rotational muscle flap, it is best to prepare and drape out the entire abdomen, leg, and the back to midline. Intravenous antibiotics are given and re-dosed throughout the procedure. If the dissection occurs around the bowel, additional antibiotic coverage may be warranted.
Resection
The resection technique depends on the specific location of the periacetabular tumor. An ilioinguinal or iliofemoral approach is used depending on the involvement of the anterior pelvis. For some resections, an additional “T” incision is made to raise the gluteus maximus as a posterior flap. In this case the anterior/inferior flap should be retracted with the origins of the sartorius and tensor fascia lata to maintain blood supply to this corner of the skin. Expose the retroperitoneal space with release of the abdominal muscles from the ilium. The inguinal ligament is transected carefully to preserve the underlying external iliac vessels. The spermatic cord is retracted medially. If the inferior epigastric vessels are maintained to the ipsilateral rectus abdominus, it can be used for a later rotational flap. If the superior pubic ramus requires exposure, the rectus abdominus muscle is released superiorly and the space of Retzius between the symphysis pubis and bladder is exposed. The femoral neurovascular bundle is elevated from the superior pubic ramus and freed distally to the profunda femoris artery to allow for adequate mobilization. If the anterior pelvis is part of the resection, the obturator vessels and nerve are ligated. If a medial portion of the superior and inferior pubic rami can be maintained, obturator neurovascular structures can potentially be saved. The adductor muscles are released from the symphysis, and eventually the hamstring muscles are released posteriorly from the ischium. If transection through the symphysis pubis is required, protect the urethra, which is just posterior to this area. The urinary catheter is usually palpable within the urethra. A Gigli saw is helpful for this cut. The external iliac vessels are dissected as proximal as necessary in the pelvis to allow the appropriate cut through the ilium. The hypogastric vessels are identified and preserved if possible or ligated if necessary. Often, depending on the soft tissue extension of the tumor, the iliopsoas obstructs an adequate view for dissection within the pelvis and needs to be partially or fully resected while maintaining the femoral nerve. The patient will have improved function if some or all of the iliopsoas is maintained. Maintenance may also preclude the need for a rotational muscle flap. At this time it is usually possible to assess whether there is involvement of the bowel, bladder, prostate, or vagina and intraoperative consultations are called if necessary. As the dissection continues proximally it is important to protect the ureter. The L5 nerve root lies over the sacral ala, and the lumbosacral plexus travels through the greater sciatic notch and both should be protected. Some tumors require an iliac cut to be made through the lateral sacrum and then superior to a point where a transverse cut across the entire ilium is safely made.
If a posterior flap is raised, the gluteus maximus is maintained along the posterior ilium and may or may not need to be partially or totally released from the iliotibial band or femur. The sciatic nerve is identified and followed proximally to the sciatic notch. The gluteus medius is either released from the iliac crest and retracted
distally or it is released via a trochanteric osteotomy and elevated proximal to the level of the iliac osteotomy. The sciatic nerve and surrounding vessels are protected in the greater sciatic notch, and the ischial spine is identified as the most inferior border of the sciatic notch. The sacrospinous ligament is released from the ischial spine after the pudendal vessels are ligated. The pudendal nerve can occasionally be maintained. Usually, the sacrotuberous ligament is released from the ischial tuberosity. The external rotators (piriformis and gemelli) are released from the femur and tagged. The iliac osteotomy is made once the soft tissues are cleared and protected within and outside the pelvis. The femoral neck cut is then made so that the hip joint can be maintained intact with the resection in case there is tumor extension into the acetabulum. After all the cuts are made, the remaining hamstrings and pelvic floor are released to remove the specimen. For cases after traumatic bone loss or as a salvage after failed hip reconstruction, much of this technique is not necessary. A more limited resection is done after débridement of the fracture fragments or removal of a prior acetabular reconstruction. In these situations, more bone and soft tissues can be maintained such that there is usually no need for a rotational flap. After a tumor resection, the operative team changes gowns, gloves, and instruments and adds or changes the upper drapes to maintain a clean field. The pelvic cavity is irrigated with warm saline using a pulse lavage system, and hemostasis is obtained. Bone wax is placed on bleeding bone edges and care is taken to prevent stretch on the pelvic neurovascular structures.
distally or it is released via a trochanteric osteotomy and elevated proximal to the level of the iliac osteotomy. The sciatic nerve and surrounding vessels are protected in the greater sciatic notch, and the ischial spine is identified as the most inferior border of the sciatic notch. The sacrospinous ligament is released from the ischial spine after the pudendal vessels are ligated. The pudendal nerve can occasionally be maintained. Usually, the sacrotuberous ligament is released from the ischial tuberosity. The external rotators (piriformis and gemelli) are released from the femur and tagged. The iliac osteotomy is made once the soft tissues are cleared and protected within and outside the pelvis. The femoral neck cut is then made so that the hip joint can be maintained intact with the resection in case there is tumor extension into the acetabulum. After all the cuts are made, the remaining hamstrings and pelvic floor are released to remove the specimen. For cases after traumatic bone loss or as a salvage after failed hip reconstruction, much of this technique is not necessary. A more limited resection is done after débridement of the fracture fragments or removal of a prior acetabular reconstruction. In these situations, more bone and soft tissues can be maintained such that there is usually no need for a rotational flap. After a tumor resection, the operative team changes gowns, gloves, and instruments and adds or changes the upper drapes to maintain a clean field. The pelvic cavity is irrigated with warm saline using a pulse lavage system, and hemostasis is obtained. Bone wax is placed on bleeding bone edges and care is taken to prevent stretch on the pelvic neurovascular structures.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree