CHAPTER 35 Rotator interval—considerations and techniques for instability
 The rotator interval is a complex anatomic area between the supraspinatus and subscapularis and contains the superior glenohumeral ligament, the coracohumeral ligament, the long head of the biceps, and the capsule.
The rotator interval is a complex anatomic area between the supraspinatus and subscapularis and contains the superior glenohumeral ligament, the coracohumeral ligament, the long head of the biceps, and the capsule. A competent rotator interval contributes to inferior stability of the shoulder but is probably not the main stabilizer.
A competent rotator interval contributes to inferior stability of the shoulder but is probably not the main stabilizer. An open rotator interval closure should not be considered to perform the same biomechanically as an arthroscopic rotator interval closure because of the difference in direction of repair and layers of tissue.
An open rotator interval closure should not be considered to perform the same biomechanically as an arthroscopic rotator interval closure because of the difference in direction of repair and layers of tissue. Although controversial, arthroscopic rotator interval closure does not appear to have any effect on posterior stability of the shoulder.
Although controversial, arthroscopic rotator interval closure does not appear to have any effect on posterior stability of the shoulder. The coracohumeral ligament tightens with external rotation and is not predictably shortened with arthroscopic rotator interval closure.
The coracohumeral ligament tightens with external rotation and is not predictably shortened with arthroscopic rotator interval closure. There is a predictable loss of external rotation with arthroscopic rotator interval closure, which may be desirable in some cases.
There is a predictable loss of external rotation with arthroscopic rotator interval closure, which may be desirable in some cases.Introduction
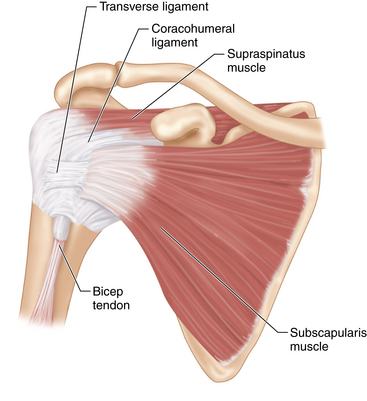
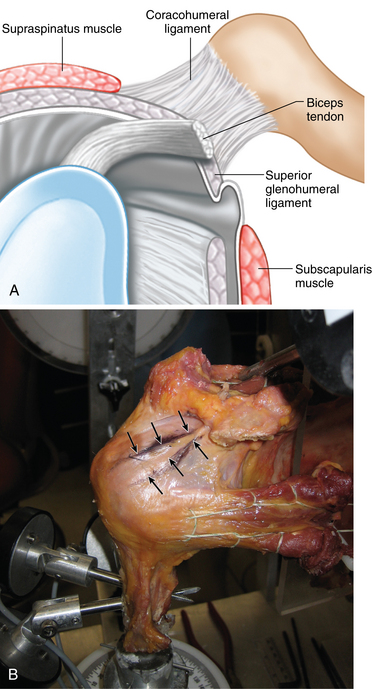
The rotator interval (RI) is a triangular space of the anterosuperior shoulder between the supraspinatus (SS) and subscapularis (SSc) tendons, containing both the coracohumeral ligament (CHL) and superior glenohumeral ligament (SGHL), as shown in Figs. 35-1 and 35-2. Its complex anatomy and complicated mechanical function keep the role of the RI in overall shoulder stability under debate. Several reports have suggested that RI structures contribute to stability by maintaining negative intra-articular pressure1 and/or resisting inferior glenohumeral translation.2–5 Other reports show that surgical imbrication of the RI augments surgical correction of multidirectional and posterior instability.2,3,5–10 Furthermore, injuries to the RI have been associated with increased glenohumeral translation,11 while fibrosis of the RI is associated with adhesive capsulitis and osteoarthritis, pathologies that commonly result in decreased shoulder range of motion and translation.
Thus, while surgical closure of the RI has been advocated in specific cases of shoulder instability, the biomechanical and clinical evidence for routine treatment is inconclusive, making the overall role of RI closure in shoulder instability controversial. One of the more pressing issues associated with RI repair is a potential loss of external rotation, as demonstrated by several cadaveric laboratory studies.5,9,10,12 In the past, RI closure was commonly performed via open surgical techniques; however, recent all-arthroscopic techniques for RI closure have been described.13,14 The purposes of this chapter are to review the indications and contraindications of surgical RI closure for treatment of glenohumeral instability and to describe operative treatment techniques with regard to glenohumeral instability.
Indications
Rotator interval repair after a shoulder instability procedure remains controversial, especially because of potential losses of external rotation postoperatively and lack of convincing biomechanical evidence. In addition, while clinical and biomechanical studies show improvement in anterior stability when arthroscopic RI closure is performed, the outcomes are not as clear regarding posterior and/or inferior stability. Currently, there are no long-term clinical studies regarding the outcomes of RI closure, and because the biomechanical data regarding the benefits of arthroscopic RI closure are controversial, the decision to perform RI closure can be difficult, and it is unknown if performing the surgery is actually beneficial for the patient. Thus, careful preoperative planning and patient selection is crucial for a successful outcome.
Preoperative history, examination, and radiographic findings
History
A thorough history is necessary to determine the best treatment options for a patient with suspected RI pathology. An isolated RI lesion is probably quite rare, and RI pathology is usually seen with concomitant instability conditions of the shoulder, including anterior, posterior, and multidirectional. Thus, in a patient with shoulder instability, it is imperative to evaluate the RI for possible deficiency. As suggested by Ho et al,15 injuries to the RI usually occur as part of a spectrum of glenohumeral pathology as opposed to a separate, isolated lesion. Surrounding structures including the labrum, coracohumeral ligament, biceps tendon, and rotator cuff are often injured along with an RI lesion; thus, presenting symptoms may be consistent with the same symptoms reported with injuries to any of these structures. The diagnosis of any additional pathology in addition to lesions to the RI is thus crucial for preoperative planning and appropriate surgical management.
Physical examination
Isolated pathology of the RI is difficult to assess on physical exam because examination findings may be vague and representative of other shoulder lesions, including anterior, posterior, and/or multidirectional instability. It is thus imperative to perform a complete examination of the shoulder, paying particular attention to signs for instability and glenohumeral pathology, including rotator cuff tears, impingement, and biceps pathology. Critical assessment of the shoulder will enable the surgeon to make appropriate decisions regarding potential operative care and will help determine if the patient actually has RI pathology or if the symptoms are due to some other cause.
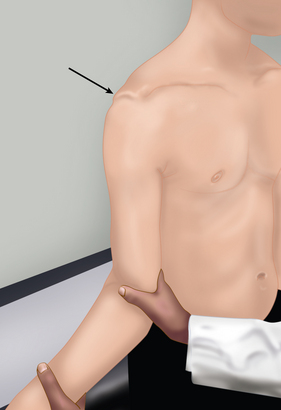
During examination, if downward traction of the arm causes inferior subluxation of the humeral head that does not resolve with external rotation of the shoulder, also known as the sulcus sign, a lesion of the RI should be suspected.11 When the RI is intact, external rotation with the arm at the side will allow for resolution of the sulcus sign as the CHL becomes taught (Fig. 35-3).11 In patients who have hyperlaxity, careful attention of the sulcus evaluation should be performed to assess for an incompetent RI. In addition, as demonstrated by Gagey et al16 if the arm is able to be abducted beyond 105 degrees when the scapula is stabilized as the shoulder is maximally passively abducted, the patient is said to have hyperlaxity of the inferior glenohumeral ligament (IGHL); however, it is not known if this is due to an inferior capsule that is enlarged or incompetent RI (Fig. 35-4).
Radiographic findings
Various imaging modalities can be helpful in the diagnosis of RI pathology, including radiographic studies, computed tomography (CT) studies, and magnetic resonance image (MRI) and arthrogram studies. Radiographic studies, including the anteroposterior, scapular-Y, and axillary views should be performed preoperatively to assess the shoulder joint as a whole, particularly if there are concerns regarding glenohumeral joint space narrowing. Associated bony deformities, such as a Hill-Sachs lesion or glenoid bone loss, can be assessed with a Stryker notch radiograph and a West Point view radiograph, respectively. CT scanning is also extremely helpful in identifying any associated bone loss, in particular when used with software that allows for 3-dimensional visualization of surface lesions. MRI studies are typically used to evaluate soft-tissue structures surrounding the glenohumeral joint, including the labrum and capsular complex, and have been used to identify both the anatomy and pathology associated with the RI.17,18 Magnetic resonance arthrogram (MRA) is the most sensitive of all imaging studies. Typical signs of RI injury include radiopaque dye in the subacromial and/or subdeltoid bursa through the RI,19 as well as radiopaque dye under the coracoid on the oblique sagittal images.20,21 Improper MRA technique can result in dye being injected into the soft tissues as opposed to intra-articularly, producing a false-positive result.22,23
Description of technique
Relevant anatomy
The RI is a triangular-shaped space of the anterior shoulder, bordered superiorly by the anterior margin of the SS tendon, inferiorly by the superior margin of the SSc tendon, medially by the base of the coracoid process, and laterally by the sulcus for the long head of the biceps (LHB) tendon and the transverse humeral ligament.2,11 Complicating the anatomy is the amount of structures contained within the relatively small space of the RI, including the CHL, the superior and middle glenohumeral ligaments (SGHL and MGHL), the LHB tendon, and a thin layer of capsule.1–3 The CHL is a fibrous structure that originates at the base of the coracoid and splits laterally into two bands. One band of the CHL inserts on the anterior edge of the SS tendon and greater tuberosity, while the other inserts on the SSc, the transverse humeral ligament, and the lesser tuberosity. The SGHL is relatively smaller than the CHL, originating from the glenoid labrum adjacent to the supraglenoid tubercle, crossing the floor of the RI deep to the CHL, and inserting on the fovea capitis on the lesser tuberosity.2,18 The LHB tendon is located between the CHL and the SGHL.
The overall function of these various structures within the RI, and thus the overall role of the RI in preserving glenohumeral stability, is unclear. The SGHL has been shown to prevent inferior translation of the abducted shoulder, while the CHL has been demonstrated to be an important stabilizer against inferior glenohumeral translation in the adducted arm. The RI capsule, while only 0.06 to 0.1 mm thick,24 is nevertheless vital in maintaining the negative intra-articular pressure and concavity-compression of the glenohumeral joint, and lesions may compromise overall shoulder stability (Table 35-1).
Table 35-1 Summary of RI Anatomy and Function
| Structure | Function |
|---|---|
| SGHL | Prevent inferior and posterior translation |
| CHL | Prevent inferior translation in adducted and abducted arm |
| Capsule | Maintain negative intra-articular pressure and concavity-compression of GH joint |
| LHB tendon | Unknown, possibly a role in shoulder stability or possibly only a vestigial function involved in pain generation if injured; potential humeral head depressor and anterior stabilizer |
CHL, Coracohumeral ligament; GH, glenohumeral; LHB, long head of the biceps; SGHL, superior glenohumeral ligament.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree