Chapter 122 Robotics in Total Knee Arthroplasty
Degenerative joint disease of the knee is treated with total knee arthroplasty (TKA) after conservative therapy options have been exhausted. However, despite conscientious planning and carefully performed procedures, surgeons are often unsatisfied with implant alignment. Various studies have described significant axial or rotational malalignment, and mediolateral and ventrodorsal tilt.2,3,15,26 Seemingly small displacements of 2.5 mm potentially alter the range of motion by as much as 20 degrees.8 None of the contemporary improvements in implant design and instrumentation have alleviated these problems.
To improve precision in surgery, robotic systems were developed. Robots are able to position and move tools accurately, thereby reducing human error. These systems rely on preoperative imaging, registration, and planning. The first clinical use was reported in 1985 in the field of neurosurgery.16 In 1992, orthopedic surgeons started using robot systems for total hip arthroplasty.4 The active surgical robot CASPAR (computer-assisted surgical planning and robotics) was initially adapted for total hip arthroplasty and for anterior cruciate ligament repair.20 Later it was developed for total knee arthroplasty. The first robot-assisted knee replacement with this system was performed in March 2000 at the Kassel Orthopedic Hospital (Kassel, Germany). A total of 108 consecutive procedures were performed at this institution and followed up for at least 5 years in a prospective study.25
Surgical Technique
Placement of Fiducial Markers
To facilitate orientation, the robot requires placement of femoral and tibial pins that serve as fiducial markers for each bone (Fig. 122-1). The robot uses these pins for spatial orientation and performs geometric calculations based on their location.
Computed Tomography Scanning and Preoperative Planning
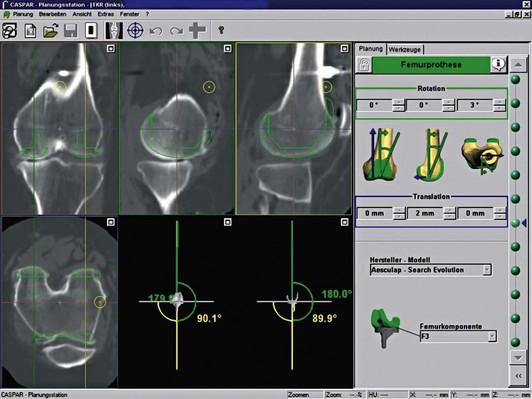
The system allows the user to select and position a specific implant in different sizes. With computer-assisted planning, the strong interdependence of all parameters, including the mechanical axes, becomes evident. Implant fit can be accurately assessed by scrolling through the scan. Unintentional notching can easily be avoided. All angles and possible geometric translations are displayed on the video screen during the planning procedure (Fig. 122-2). The system informs the user about the expected change in extension and flexion gaps and the resulting ligament tension. After positioning the implants, the milling areas are specified in order to protect the surrounding soft tissue. As a last step, the system prints out an overview of the final plan. All data are stored on a PC card and transferred to the robot control unit before surgery.
Robot-Assisted Surgery
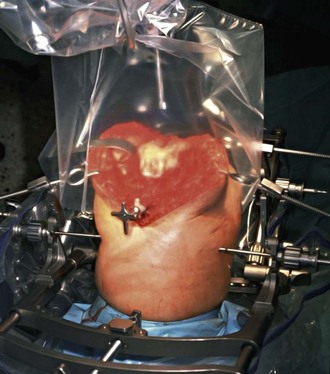
A conventional median incision with parapatellar approach to the knee joint is used. The knee joint is secured by a transfemoral and transtibial self-cutting screw to a specially designed frame. This rigid frame is also used for fixation of self-holding soft tissue retractors. To control for unwanted micromovements of the leg during robotic surgery, rigid bodies with light-emitting diodes (LEDs) are firmly attached to the frame. The LED signal is constantly monitored by an infrared camera system, which will automatically shut off the robot in the event of excessive motion (Fig. 122-3). After registration of the fiducial markers, robotic milling is started by the surgeon. The cutting tool is equipped with internal water cooling and irrigation. A splash guard helps keep the operative field and LEDs dry and clean (Fig. 122-4). Milling heads are changed during the procedure, depending on the type of cut to be made. Varying with the size of the implant and bone density, the entire milling procedure takes approximately 18 minutes. If required, it is possible to revert to conventional manual technique at any point during surgery.
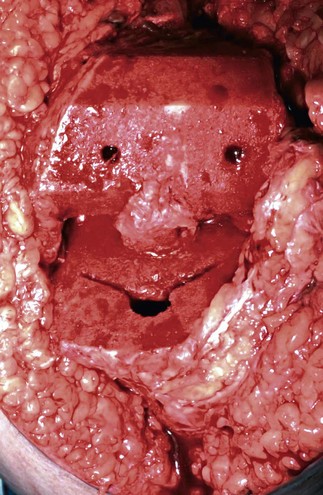
The resulting bone surfaces are accurately shaped and smooth (Fig. 122-5). After the fixation frame and pins are removed, soft tissues are balanced and the components of the implant are inserted. In this study, we started with the cemented LC Search Evolution knee system (Aesculap, Tuttlingen, Germany) in the robotic group because this was the first knee implant system geometry that was loaded into the planning software.
Patients and Methods
A total of 108 knees were operated using the CASPAR robot system. The following cruciate-retaining implant designs were used: 70 Search Evolution (Aesculap), 31 PFC Sigma (DePuy Orthopaedics, Warsaw, Ind), and 7 Genesis (Smith & Nephew, Andover, Mass). Of these, 55 were implanted with both components being cemented (Figs. 122-6 and 122-7), 46 implants were hybrids (tibia cemented, femur cementless), and 7 were completely cementless (Fig. 122-8). The average age of the patients (74 women, 34 men) was 66 years (range, 37 to 87 years). Patients were clinically evaluated before and after surgery according to their Knee Society score.12 All patients were followed up at intervals of 3, 6, 12, 24, and 60 months after surgery. No patients were lost to follow-up.

Figure 122-6 Anteroposterior (A) and lateral (B) x-rays of a patient with medial gonarthrosis before robotic TKA.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree