Abstract
Objectives
The National Hospital of Saint Maurice (HNSM) for Physical Medicine and Rehabilitation aims at strengthening its position as a pivot rehabilitation and physical therapy center. The opening in 2011 of a new unit for the evaluation and treatment of motor disabilities meets this objective. This project includes several parts: clinical, financial, architectural, organizational, applied clinical research as well as dealing with medical equipments and information system. This study focuses on the risk assessment of this future technical unit.
Methods
This study was conducted by a group of professionals working for the hospital. It started with the design of a functional model to better comprehend the system to be analyzed. Risk assessment consists in confronting this functional model to a list of dangers in order to determine the vulnerable areas of the system. Then the team designed some scenarios to identify the causes, securities barriers and consequences in order to rank the risks.
Results
The analysis targeted various dangers, e.g. political, strategic, financial, economical, marketing, clinical and operational. The team identified more than 70 risky scenarios. For 75% of them the criticality level was deemed initially tolerable and under control or unacceptable. The implementation of an action plan for reducing the level of risks before opening this technical unit brought the system down to an acceptable level at 66%.
Conclusion
A year prior to opening this technical unit for the evaluation and treatment of motor disabilities, conducting this preliminary risk assessment, with its exhaustive and rigorous methodology, enabled the concerned professionals to work together around an action plan for reducing the risks.
Résumé
Objectifs
L’hôpital national de Saint-Maurice, établissement de soins de suite et de réadaptation, souhaite conforter son positionnement d’établissement de rééducation spécialisé et de recours. L’ouverture en 2011 d’un plateau technique d’analyse et de traitement des troubles du mouvement répond à cette ambition. Ce projet comporte des volets clinique, financier, architectural, organisationnel, liés aux équipements médicaux, au système d’information et à la recherche clinique appliquée. L’étude consiste en l’analyse des risques a priori de ce futur plateau technique.
Méthodes
L’étude est réalisée par un groupe de professionnels de l’établissement. Elle débute par la réalisation d’une modélisation fonctionnelle afin de décrire le système analysé. L’analyse des risques repose sur la confrontation de ce système avec une liste de dangers, permettant d’établir les vulnérabilités du système. Elle se poursuit par l’élaboration de scénarios afin d’identifier causes, barrières de sécurité, conséquences et de hiérarchiser les risques.
Résultats
L’analyse ciblée sur les dangers politique, stratégique, financier, économique, commercial, clinique et opérationnel permet d’identifier plus de 70 scénarios dont 75 % sont estimés de criticités initiales tolérables sous contrôle ou inacceptables. La mise en œuvre d’un plan d’actions de réduction de risque avant l’ouverture du plateau technique fait passer le système vers un niveau acceptable en l’état à 66 %.
Conclusion
L’analyse préliminaire des risques, méthode exhaustive et rigoureuse, permet, un an avant l’ouverture du plateau technique, de faire un point d’avancement du projet et de fédérer les professionnels concernés autour d’un plan d’actions de réduction des risques.
1
English version
1.1
Introduction
1.1.1
General context of the study
In April 2008, two acts were voted to determine the authorizations and technical conditions required for Physical Medicine and Rehabilitation (PM&R) Centers. They introduced the notion that establishments need an authorization to provide specialized care while having an expert and support role for other healthcare structures. For each type of specialized care there are specific requirements including ones for opening technical units within PM&R hospitals or clinics. All these establishments are required to abide by the new acts and regulations and the French Healthcare Organizational Framework ( Schéma Régional d’Organisation Sanitaire – SROS) by April 2011.
A new national financing system will be implemented in 2011-2012 for PM&R care; each clinical activity will be attributed a certain amount of money. Some additional elements will also be taken into account: specific missions and new contracts, expensive medicines but also “technical units or labs” with additional financing. Since 2009, a new temporary model has been tried out: the Activity Value Indicator (Indicateur de Valorisation de l’Activité) .
Several neurological, orthopedic, rheumatology or congenital pathologies are involved in gait, posture or motor disorders .
There are also various etiologies for these disorders: congenital or acquired (e.g. trauma, degenerative). Motor impairments affect 13.4% of the French population, i.e. more than 8 million inhabitants. The greater Paris region has 12 million inhabitants and 20% of them are children. The prevalence of cerebral palsy in children is estimated at 1.12 for 1000 children. The affected persons, children or adults alike, can benefit from gait and movement assesment and/or their therapeutic care.
Movement and gait analyses yield some objective elements that can be confronted to clinical data to refine the diagnostic approach of the various disorders of the gait cycle or other motor impairments and thus facilitate the therapeutic decisions. Thanks to databases of patients’ medical charts, we can now evaluate and compare the efficacy of the various treatments (surgery, orthoses, medications, rehabilitation programs).
Furthermore, for the past 10 years, just like in the United States, healthcare professionals and hospitals have been instructed to conduct global and coordinated risk management approaches, in order to prevent and reduce the onset of medical errors and guarantee the safety of their therapeutic care .
1.1.2
Specific context surrounding the study
Since 1998, the Saint-Maurice National Hospital (HNSM) with its center for PM&R care has developed a clinical and technical expertise in gait and movement analysis (video, video-EMG, treadmills, and posture analysis tools) as well as treating spasticity (Botulinum toxin injections under ultrasound monitoring and/or electrostimulation, multidisciplinary consultations on spasticity).
The HNSM wishes to strengthen its position as an expert PM&R center for the therapeutic care of children with cerebral palsy and adults with other pathologies, mainly neurological or geriatric ones.
In 2011 a program on the evaluation and treatment of motor disabilities, defined at a National and European level , will be implemented and located in a new specific technical unit within the HNSM. This program will help develop new medical activities by acquiring medical equipments and new competencies while strengthening its existing multidisciplinary team. With innovative evaluation tools the medical teams will spread their educational and clinical research activities.
In a context of uncertainty regarding the future financing of National healthcare, this project answering the needs of public healthcare, represents a strategic and economical challenge for our hospital. The future technical unit for the evaluation and treatment of motor disabilities must guarantee the safety of users and highest quality of care, in order to satisfy the patients, their family, the users and healthcare staff while ensuring the long-term viability of the structure.
The study consists in assessing the potential risks of the future technical unit by conducting a preliminary risk assessment analysis according to a method used largely in the industrial world. We can now observe in Healthcare, the development and use of tools and methods that have been widely applied to aeronautic, aerospace and nuclear industries .
1.2
Material
Movement analysis (MA) of the upper limbs, trunk or lower limbs includes analysis of movement observation (AMO) and quantified analysis of movement (QAM).
AMO combines an analytic and static clinical examination with a visual analysis of gestures or gait, ideally with video data.
QAM includes:
- •
video analysis with EMG: Video data in the frontal and lateral planes synchronized with a dynamic surface EMG recording;
- •
kinematics (mechanics that describe the various joint angles);
- •
kinetics if the patient can walk without technical aids on the force plates; kinetics supply information on joint moments and forces exerted.
All these elements help us understand the biomechanics of motor disabilities.
Recorded kinematics data require an optoelectronic system (numeric cameras with infrared high definition, retro-reflective markers). This allows for 3D-movement measurements and analysis by reconstructing a human model representing portions of limbs in the three dimensions. The results obtained in one patient are compared to a norm.
Spatiotemporal gait parameters can be quantified through treadmill data recordings, GAITRite ® (Biometrics), which includes pressure sensors to compare gait with or without orthoses and/or technical aids.
Static and dynamic plantar pressure measurements can be recorded when walking on the Zebris ® (Biometrics) platform with various pressure sensors. The measures can only be taken when the person is barefoot, without any technical assistance. The measure of the angle of postural oscillations derived from plantar pressure measurements gives an image of the patient’s balance control. Spatiotemporal parameters during gait are also collected.
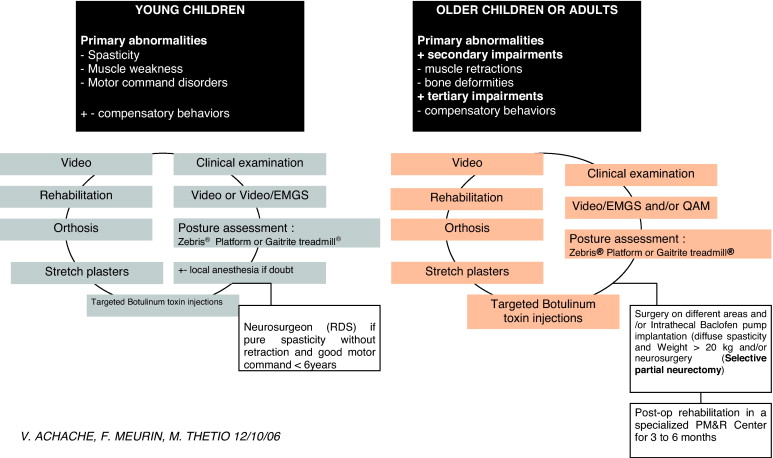
The therapeutic program associates to various degrees: medical treatments, including intramuscular injections of Type A Botulinum toxin (Botox ® manufactured by Allergan Labs and Dysport ® by Beaufour-Ipsen) , physiotherapy, occupational therapy, muscle stretching plasters, orthoses, self-rehabilitation. It can also involve orthopedic surgery and/or neurosurgery ( Fig. 1 ).
1.3
Method
The method used, Preliminary Risk Assessment (PRA), is taught at the Ecole Centrale in Paris, as part of the Master of Business Management in Risk management and safety in healthcare structures and networks (A. Desroches, ).
The study is driven by a multidisciplinary group of professionals from the hospital representing the various players involved in the system studied. The team is made up of:
- •
the specialized physician and the physiotherapist, who is also a Doctor in Neurosciences, in charge of conducting movement assessment;
- •
the department manager and director;
- •
the hospital general manager;
- •
the healthcare general manager;
- •
the medical assistant;
- •
the physicians who are potential users of the future technical lab;
- •
the biomedical engineer;
- •
the pharmacist;
- •
the electronic medical records and healthcare information physician;
- •
the chief financial officer.
The project team met several times either in networking sessions or individual meetings and came up with a complete description of the projects and subsequent practices as well as various documents needed for the risk manager to build the risk assessment framework. The team also designed the functional analysis to be used with a mapping of dangerous situations and subsequent scenarios. Then they carefully read, made changes and validated it. Direct observations, onsite visits and relevant documents completed these sources.
The experience was based on a review of the literature and advice from professionals who contributed to the design and implementation of similar units.
The following paragraphs present the main steps for this Preliminary Risk Assessment (PRA).
1.3.1
A functional model to describe the system to be analyzed
The program for the evaluation and treatment of motor disabilities include:
- •
therapeutic care organization (scheduling the therapeutic care, logistics, welcoming the patients);
- •
evaluation and treatment of motor disabilities (medical evaluation, posture evaluation, 3-D gait analysis, interpreting the results, therapeutic proposals, Botulinum toxin injections);
- •
evaluating the therapeutic care (financing, risk assessment, clinical research).
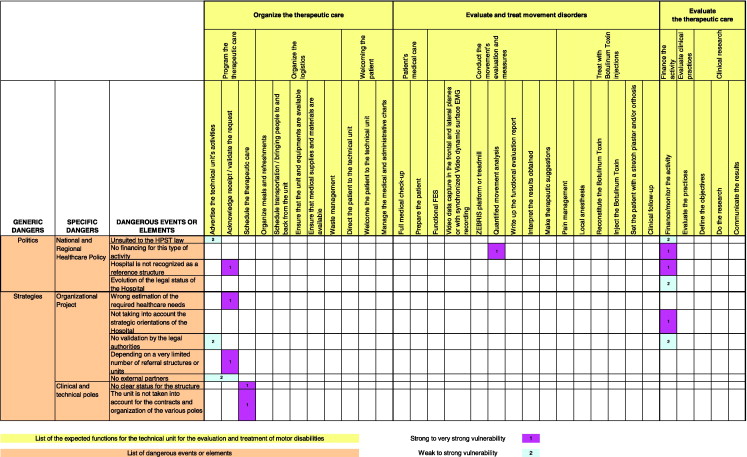
The list of these various functions is presented in Fig. 2 .
1.3.2
Making a list of all potential dangers that the “technical unit for evaluating and treating motor disabilities” could be confronted to
Starting with fifteen generic dangerous situations, the team’s experience and knowledge allowed for drawing up an inventory of specific dangers categorized into dangerous events or elements. The risk assessment analysis focused first on these generic dangers: political, strategic, financial, economical, marketing, clinical, operational. Later on the team worked on other dangers: legal, technical, technological, safety of persons and goods, information system, human factor, social factors, environmental factors.
1.3.3
Identifying dangerous situations according to the vulnerability of the elements
The double entry table used for this analysis includes on the X-axis all the functions expected for the future technical unit (e.g. financing the activity) and on the Y-axis, the list of all dangerous elements (e.g. no planned financing for this type of activity in the National and Regional healthcare politics). For each crossing of the axes, the professionals define if the vulnerability to the system is: strong to very strong (grade 1), weak to moderate (grade 2) or null.
Thus we get a mapping of the dangerous situations shown in Fig. 2 .
1.3.4
Making up scenarios (PRA scenario)
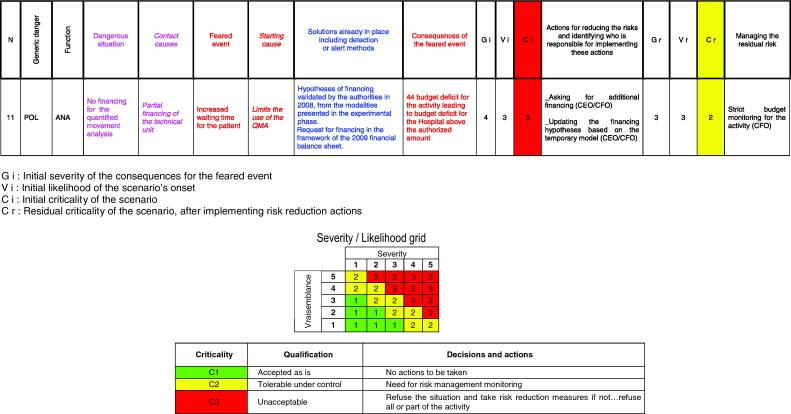
When a strong to very strong vulnerability is identified, the professionals define the nature of the dangerous situation (e.g. lack of financing for the QAM activity) and elaborate a scenario around it. The scenario presents the causes and consequences of the feared event but also the solutions already in place such as detection methods or alert signals ( Fig. 3 ).
1.3.5
Evaluating the impact of the scenarios to rank the risks and establish an order of priorities
Using scales that measure the severity of the consequences and likelihood of the event validated by RA professionals assesses each scenario.
The severity of the feared consequences is graded on five-point scale:
- •
Grade 1, minor: no impact on the performances and safety of the activity;
- •
Grade 2, significant: deterioration of the system’s performances without any impact on the safety (delayed therapeutic care with no consequences, written complaint from a patient with no compensation, employees loosing motivation, financial loss but still within the pre-determined amount, deterioration of the HNSM’ image);
- •
Grade 3, severe: severe deterioration or failure of the system’s performances without any impact on safety (aggravation of a patient’s health status or delayed therapeutic care with reversible complications, patient’s complaint with compensation, tension within the workforce, financial loss above the pre-determined amount, deterioration of the HNSM’s image);
- •
Grade 4, critical: deterioration of the system’s safety or integrity (aggravation of the patient’s health or delayed therapeutic care with irreversible consequences; patient’s complaint followed by legal sentence and moderate compensation amount: active opposition from the workforce, the activity comes under budget implying financial losses for the hospital above the authorized amount, closing down the unit);
- •
Grade 5, disaster: severe deterioration or security failure or complete system failure (death of a patient, complaint followed by a legal sentence and heavy compensation amount, resignation from all employees, structural weakness, closing the HNSM).
The scenario’s likelihood is also based on a five-point scale:
- •
Grade 1, impossible to not likely: once or less than once over a 5-year period;
- •
Grade 2, very unlikely: between once a year to more than once every 5 years;
- •
Grade 3, unlikely: between once a month and more than once a year;
- •
Grade 4, likely: between once a week to more than once a month;
- •
Grade 5, very likely to certain: more than once a week.
These two figures can help determine the scenario’s criticality based on a grid ( Fig. 3 ). Three criticality levels: acceptable, tolerable under control or unacceptable. The criticality matrix indicates that for the professionals in this particular context, the onset of a Grade 3 event (severe, i.e. having an impact on the system’s performances) with Grade 4 likelihood (likely, i.e. between once a week and more than once a month) is unacceptable.
1.3.6
Defining and strengthening the resulting actions
Development of a risk reduction plan.
1.3.7
Follow-up and control the risk reduction actions implemented
To maintain, over time, a level of risk in accordance with the objectives set.
1.4
Results
1.4.1
Functional analysis
The functional model allows for defining the system’s constraints and performances.
The project, with its architectural aspect and acquisition of biomedical and information system equipments, amounts to a 1.8 million euros investment and 300 k€ in additional expenses per year. Conducting and interpreting these movement analyses require some clinical competencies in PM&R medicine, biomechanics and neurophysiology.
Regarding financing the activity, the team built a financing value model in phase with the PM&R activity and in accordance with the Activity Value Indicator (AVI) that will be implemented soon. The new activity’s income will be set according to the number of AVI points for each week/patient (Standardized Weekly Summary) times the number of hospital days/patient during these weeks. The AVI points obtained for each week/patient are deducted from an algorithm formula taking into account the specific parameters correlated to the patient’s care (applicable to postural analyses for example). Due to the lack of guarantees for the financing mode of these technical units and based on the AVI model, the 3-D movement analysis activity will not yield any additional income.
These constraints forced the team to set strict objectives for this activity to guarantee a stable financial situation for the HNSM. At the beginning of the project, the center made the hypothesis of a 60% activity increase, bringing up the number of patients from nine to 15 patients per day in average, including the Botulinum toxin injections. Regarding human resource the project needs one full time engineer, one full time physiotherapist, one full time medical secretary and one part time physician.
1.4.2
Initial criticality analysis
PRA targeted on political, strategic, financial, economic, marketing, clinical and operational dangers identified 77 scenarios: 26% were C1 (accepted as is), 64% were C2 (tolerable under control) and 10% were C3 (unacceptable).
This initial criticality analysis is based on the technical unit opening with the elements in place in 2009.
The scenarios correlated to technical, technological and information system aspects, human and environmental factors as well as safety and social contexts will be studied six months before the unit’s construction.
A risk reduction action plan is implemented; it combines preventive actions to decrease the likelihood of the scenarios and protective actions to decrease the severity of the consequences.
It focuses on the following aspects:
- •
Financial:
- ∘
update financing hypotheses based on the temporary AVI model,
- ∘
ask for additional financing,
- ∘
optimized the PMSI data collecting,
- ∘
implement a health economics monitoring for this new technical unit;
- ∘
- •
Organizational:
- ∘
get the directing board to validate the objectives and management plan,
- ∘
implement an institutional and structured approach for the structures and/or units referring patients to our HNSM’s new technical unit,
- ∘
increase our healthcare capacity,
- ∘
define the future management of jobs, human resources and competencies for this unit,
- ∘
organize the medical appointments’ schedule,
- ∘
define the logistics regarding getting patients to the new unit and back to their starting point,
- ∘
harmonize our institutional documents before opening this new unit;
- ∘
- •
Clinical:
- ∘
evaluate professional practices,
- ∘
point out and report adverse events;
- ∘
- •
Structures and equipments:
- ∘
final opening of the new technical unit,
- ∘
organize equipment maintenance.
- ∘
1.4.3
Analysis of residual criticality
Implementing a risk reduction action plan before opening of the new technical unit did bring down the system to an acceptable C1 level at 66% and a tolerable under control C2 level at 34%.
For 26 identified scenarios matching the residual C2 dangerous situations, it was decided to implement a control action plan to limit the residual risks:
- •
C1_Budget monitoring;
- •
C2_PMSI data control;
- •
C3_Finances control;
- •
C4_Evaluating the satisfaction of referral centers/structures and patients;
- •
C5_Insurances for liability and damages.
The charts representing the scenarios’ proportion according to their criticality and by generic danger is useful for having a direct vision of the entire system before and after implementing the risk reduction action plan ( Fig. 4 ).










