Revision with Adequate Bone
Bernard F. Morrey
Mark Morrey
Joaquin Sanchez-Sotelo
INTRODUCTION
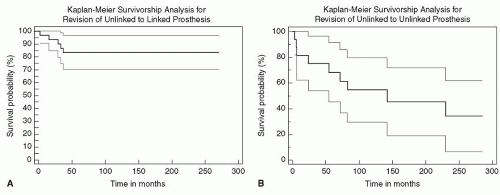
It is uncommon that augmentation of some sort is not required when revising a failed elbow replacement. The clinical setting in which this is seen consists of those instances in which the revision is with a very well-fixed implant with small, short stems. This is usually the case when revising an unlinked device (Fig. 38-1). This occurs with infection and with instability of unlinked implants, as well as with fractured stems. The overall requirement for a possible recurrent reinsertion is to remove the well-fixed implant while preserving the ability to obtain good fixation in the residual host bone.
INDICATIONS/CONTRAINDICATIONS
Contraindications
Inadequate host bone to obtain reliable fixation
Low-grade sepsis
Nonfunctional hand
Absent active elbow flexion
Fracture of host bone
In general, there are three steps that must be considered for successful reimplantation:
The effective strategy to remove the well-fixed device
The ability to remove residual cement without significantly violating the host bone allowing reliable reinsertion
Reinsertion technique
In all instances, preoperative planning is important for all three phases of the revision.
PREOPERATIVE PLANNING
Preoperative planning may be categorized according to a couple of considerations.
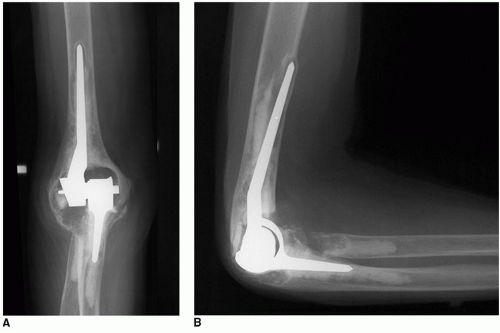
Implant system. It is critically important to assure that there is an adequate size in both length and diameter of stems to accommodate the pathology encountered at the revision (Fig. 38-3).
Osseous augmentation. Consideration of the possibility of osseous augmentation should always be given. Even in instances in which it is anticipated that this will not be necessary, breaches in the cortex and bone grafting behind the flange often require that some bone be available for these limited applications.
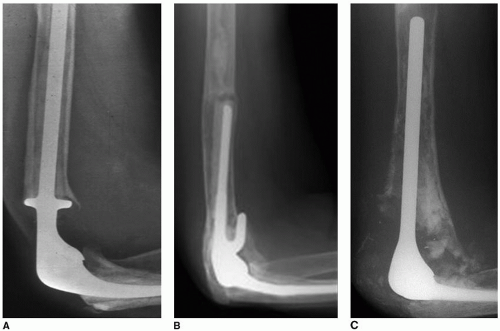
Implant stem position. Observe the AP and lateral projections. If the tip of the stem is centered, preparation is relatively easy. If the tip of the stem is touching the cortex, cement removal without breaching the cortex is very difficult (Fig. 38-4).
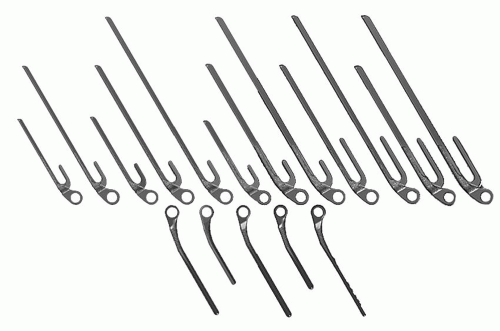 FIGURE 38-3 A full array of implant lengths and diameters is important when considering any revision procedure. |
The Triceps
A common residual problem after revision particularly for sepsis is that of triceps insufficiency (5). For humeral revisions, the triceps may be able to be preserved in the revision setting.
It is disappointing after a difficult revision that is otherwise successful to find that the patient has lost triceps function. Thus, as the final step prior to closure, the triceps must be meticulously addressed and repaired or occasionally reconstructed. Care should be taken to observe the presence and nature of the olecranon, and all efforts should be made to assure this lever arm is present to further guarantee the likelihood of active extension of the elbow joint. Lacking this, not only will the patient have a significant functional impediment but patients without triceps function also tend to have more significant flexion contractures.
The Ulnar Nerve
Great care must be taken before surgery to assure a clear understanding of any ulnar nerve symptoms as well as previous history of managing ulnar nerve and determining its current location. If patients do not have ulnar nerve symptoms at the time of their revision, the nerve is always identified but it is left alone. If the ulnar nerve is symptomatic and if it is felt that the symptoms can be alleviated with intervention and decompression at the time of the revision, then this should be carried out. Be prepared to use magnification and anticipate an additional 15 to 30 minutes to the procedure.
As with the triceps, preserve. If the nerve has been relocated, place it securely in a favorable environment.
Component Removal
The real key to successful reimplantation is that it starts with successful component removal. As in the hip, we have learned that this is best done by controlled osteotomy. Today, careful osteotomies of the humerus and of the ulna do afford the opportunity to reliably remove cement without compromising in a significant way the osseous integrity of the host bone.
Cement Extraction
This becomes a major issue and can in fact alter the surgical procedure from that of a reliable reimplantation to one in which graft augmentation is required. This latter occurs when there has been a breach in the cortex or if a fracture occurs during the cement or component extraction. Strategies for cement removal include osteotomy and drilling and reaming. Ultrasound is effective but dangerous and has been largely abandoned by this surgeon.
Reinsertion of the Revision Component
This is a critical step. One of the most subtle issues is that of surgeon fatigue that occurs with difficult extraction and cement removal. There are instances in which sometimes these steps almost seem to represent the major goal of the procedure and less vigilance may be provided for cementation and reinsertion of the implant. This must be guarded against. Hence, the final stages of the revision consist of meticulous preparation of bone plugging of the canal assuring there is adequate size of the implant to serve as the revision device and to bypass any osseous deficiency.
Cement Delivery System
It has been shown that the quality of the cementation is critically important (6). This is possibly more so in a reimplantation revision setting. The introduction of cement should be done through a delivery system with the cement inserted in a retrograde fashion. The canal should be plugged in order to enhance as much as possible the bone-cement interface. This point is probably more important in a revision than in a primary procedure.
SURGICAL TECHNIQUE
Humeral Revision
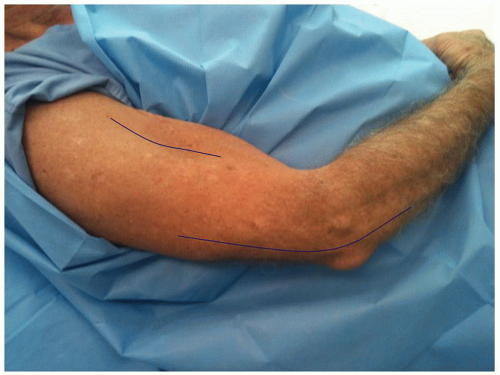
Exposure The patient is placed in the supine position with the arm across the chest. However, if the revision is felt to require a more proximal exposure, the preparation includes the shoulder as if a shoulder replacement is to be done. The supplemental anterolateral incision is sometimes used to obtain access and exposure of the proximal humerus (Fig. 38-5).
The triceps is maintained if at all possible. This may be the case with humeral revision. It is virtually impossible with an ulnar revision.
The medial and the lateral condyles are usually stripped of soft tissue to obtain complete exposure of the distal humerus.
Implant Removal
If the attachment cannot be preserved, the triceps is split proximally exposing the posterior surface of the humerus.
The length of the implant is determined, and a posterior truncated trapezoidal-shaped window is removed from the posterior humeral cortex.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree