Fig. 42.1
Nonanatomical position of the femoral tunnel and the new correct position (white circle)
42.4 Clinical and Instrumental Diagnosis
While clinical examination of recurrent anterior knee joint instability is identical to that for primary ACL rupture, a foremost concern is understanding what were the causes, besides injury, so that surgical treatment can be planned appropriately. Recurrence may be due to having missed peripheral ligament damage during primary reconstruction or because of axial malalignment with graft elongation over time. The incidence of such failures varies from 2.8 to 31 % [27, 36, 43]. The most commonly missed peripheral lesions are posteromedial and posterolateral injuries in particular [44]. If associated with previous total or partial medial meniscectomy, posterolateral injury can lead to varus angulation and progressive elongation of the new ACL, resulting in ligament deficiency. In such cases, revision should be combined with valgus-producing tibial osteotomy to avert repeat recurrence [45]. Another option that may be considered is meniscal graft placement when the varus deformity is related to the lack of the internal meniscus. Such approaches, however, will not satisfy the needs of professional athletes who want rapid return to sports activity.
Plain and weight-bearing radiographs are important for identifying metal implants that may interfere with the placement of a new tunnel, to evaluate tunnel position (Fig. 42.2) and any axial malalignment. Computed tomography is useful for quantifying bone tunnel enlargement, which may be over- or underestimated on plain radiographs [46, 47]. Examination will include magnetic resonance imaging (MRI) to evaluate the state of the tunnel, other ligaments, menisci, chondral tissue, and all joint compartments.


Fig. 42.2
X-ray standard to evaluate tunnel position (incorrect)
In addition to physical examination and imaging studies, preoperative work-up will include thorough history taking to collect information on the onset of symptoms, the time since primary surgery, the extent of new injury, the type of rehabilitation received, and the type of sport the patient engages in. Collectively, this information provides essential clues to understanding whether the recurrence is due to biological failure, injury, or surgical error. Also useful is having the patient’s medical records at hand to review the type of graft implanted, the type of implantation technique, the preoperative condition of the menisci and cartilage, and the type of fixation material used.
42.5 Graft Selection
Graft selection in revision ACL reconstruction depends on many factors, including the tendon used in the primary repair procedure, tunnel position and widening, peripheral laxity, and the surgeon’s experience. Both autografts and allografts may be used. The most commonly used autografts are the patellar tendon, the gracilis and semitendinosus tendons, and the quadriceps tendon. The advantage of using the patellar tendon is that it can be harvested together with a large tibial wedge to fill tunnel enlargement. Though reuse of the patellar tendon from the primary surgery was once proposed [48], various authors have advised against employing this technique because of the tendon’s diminished mechanical properties and the higher risk of complications such as patellar fracture and tendon rupture [49]. The quadriceps tendon has the same mechanical properties as the patellar tendon but is associated with a higher risk of patellar fracture when the patellar tendon has been used. The pes anserinus tendons offer the advantage that harvesting creates fewer problems at the harvest graft site; however, because they are relatively small, they cannot be used when a preexisting anatomic tunnel will be used and when the patellar tendon and a tunnel (diameter, 10–11 mm) were employed in the primary surgery. Again, because they are small, pes anserinus tendons cannot be used in tunnel enlargement; however, they do permit easier creation of a new tunnel when the old tunnel is malpositioned, and there is less space to create a new tunnel in a correct anatomical position. The literature reports no differences in results with the use of patellar or hamstring tendons, as for primary reconstructions.
Allografts have the distinct advantages that there is no harvest graft site morbidity and that they allow for multiple ligament reconstructions and, especially important, large bone gaps from tunnel enlargement can be filled. Though there do not appear to be any significant differences between the use of allografts and autografts [50], failure rates with soft tissue allografts were higher in young athletes [51]. Because biological incorporation of allografts is slower [52] and the failure rate is higher in elite athletes, we advise against their use as a first choice in graft selection. In the United States, allografts are used in just over 50 % of revision ACL reconstructions and patellar grafts in 50 % [38]. Generally, we prefer using ipsi- or contralateral autografts, reserving allografts for repeat revision, associated ligament damage, and when large bone wedges are needed for tunnel enlargement.
42.6 Treatment Strategy
Revision ACL reconstruction can be performed as a two-stage or more often using a single-stage technique, the preferred of the two, because of the longer time needed for bone defect filling (3–5 months after bone grafting of the tunnel on average) and the higher risk of meniscal tears and chondral degeneration, with rapid progression of arthrosis [27, 53, 54]. The two-stage technique should be reserved for cases in which there is evidence on preoperative computed tomography or during surgery of excessive widening of ≥16–17 mm in diameter of one or both tunnels [55].
The less anatomic the tunnel position, the easier it will be to create an anatomically correct tunnel. New tunnels will have a vital spongious bone wall that will promote incorporation of the new graft (Fig. 42.3). We believe that, in order to create a new femoral tunnel, the surgeon will need to be familiar with the anteromedial and the outside-in techniques. Both portal techniques allow the tibial and femoral tunnels to be drilled independently for achieving an anatomically more correct tunnel position [56]. Particularly for the femoral bone, if a preexisting tunnel has been placed with the transtibial approach, a completely new tunnel can be created along its entire length. If the old femoral tunnel is malpositioned but close enough to the anatomical position, the outside-in technique is preferable since it is more likely to allow for the creation of a new tunnel with a correct exit point, which may be the same as the aperture of the old tunnel but having a completely different direction. The technique we apply entails reaming over the guide wire in both outside-in and anteromedial portal reconstructions at about 6 mm in diameter less than the final diameter. The tunnel is then widened by free-hand reaming to the diameter of the previously prepared graft. Using increasingly larger diameter reamers permits approximation of the correct tunnel position until the definitive tunnel diameter has been created and allows for correcting tunnel placement, as determined by knee joint flexion-extension (anteromedial technique) and free-hand reamer direction without the guide wire [40]. Use of the medial port in both techniques permits complete visualization of the entire medial wall of the lateral condyle and precise positioning of the tunnel.
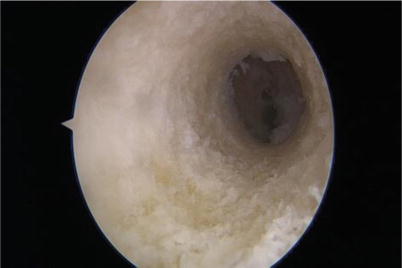
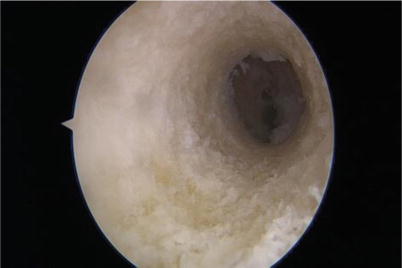
Fig. 42.3
New tunnels will have a vital spongious bone wall
Assuming that anatomic placement of the femoral tunnel during primary reconstruction surgery will become increasingly precise, we will likely encounter anatomically placed tunnels in the future. In such cases, we will need to approach the old tunnel via the anteromedial or outside-in technique but drilling to a larger diameter to remove bone and obtain a tunnel wall with vital tissue that will promote integration of the new graft. For this reason, it will be better to use a patellar graft with a bone wedge that can be shaped to the new tunnel or to use an allograft.
One of the major problems is the tibial tunnel. Creating a completely new tibial tunnel is practically impossible because of overlap, at least at the exit point. A similar challenging situation is a preexisting tunnel aperture that is too posterior. Therefore, even if we have created a new, more anteriorly and anatomically correct tunnel, the exit points will overlap and position the new graft posteriorly, raising the risk of renewed failure. To overcome this problem, we can fill the posterior end of the tunnel with a bone dowel and perform a two-stage revision or revision with a double-bundle technique and tibial tunnel widening [55].
Synthesis materials should be removed if they induce hypersensitivity reactions or interfere with the new tunnel. If located near the new tunnel, they should be left in place to avert wall rupture and tunnel enlargement.
In recurrence of knee joint instability with moderate to severe ligament laxity (pivot shift test score 3+), external extra-articular plasty should be performed, for which we prefer the Coker-Arnold procedure, or anterolateral ligament reconstruction considered.
An additional concern is deterioration of the secondary stabilizers in recurrences due to nontraumatic graft elongation. Posteromedial meniscocapsular separation (Fig. 42.4) must be repaired because the posterior horn of the medial meniscus and the tibial meniscal ligament serve as secondary stabilizers of anterior tibial translation when the ACL is absent. In chronic laxity, as in nonfunctional grafts, there is progressive detensioning, leading to rupture of the meniscocapsular insertion or of the posteromedial meniscotibial ligament [31]. Such injuries should always be repaired to prevent excessive strain on the graft, together with retensioning of the posteromedial corner, which can be easily performed using femoral or tibial suture anchors, depending on the type of lesion.


Fig. 42.4
Posteromedial meniscocapsular separation
42.7 Rehabilitation and Return to Sports
Over 40 % of patients do not return to their pre-injury athletic activity level after repeat ACL reconstruction [13, 15, 36, 41]. Chondral and meniscal damage affects the capacity for recovery, and improvement after repeat ACL reconstruction is less favorable than after primary surgery. Except for a few case series, there are no studies involving only professional athletes [13]. In revisions with placement of a new tunnel, the rehabilitation protocol is the same as for primary reconstruction since we can rely on the primary fixation. If there are problems with tunnel enlargement, slow rehabilitation at least for the first month postsurgery is advisable to reduce the risk of further enlargement and biological failure. In peripheral reconstructions, the rehabilitation protocol should be adapted to the type of arthroplasty performed. We use the same rehabilitation protocol after external extra-articular plasty as after ACL reconstruction. Early rehabilitation after primary ACL surgery is important, whereas the use of braces affords no extra advantage. A slow rehabilitation program after revision ACL reconstruction is recommended; in many cases, bracing can aid in facilitating graft integration. The timing of return to sports should be discussed with the patient since it varies and depends on muscle recovery, psychological factors, neuromuscular control, and knee joint stability.
References
1.
Giannotti SM, Marshall SW, Hume PA, Bunt L (2009) Incidence of anterior cruciate ligament injury and other knee ligament injuries: a national population-based study. J Sci Med Sport 12(6):622–627CrossRef
2.
3.
4.
Mullaji AB, Marawar SV, Luthra M (2008) Tibial articular cartilage wear in varus osteoarthritic knees: correlation with anterior cruciate ligament integrity and severity of deformity. J Arthroplasty 23(1):128–135CrossRefPubMed
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






