Chapter 50 Revision Anterior Cruciate Ligament Surgery
One-Stage versus Two-Stage Technique
As the need for anterior cruciate ligament (ACL) revisions increases, it will be imperative for surgeons to identify the causes of failure of the primary procedure accurately and address them in a systematic fashion. Pitfalls must be recognized and avoided to optimize the success of the revision procedure. The accurate placement of femoral and tibial tunnels should not be compromised by the index tunnel placement.9 Depending on the type and location of the fixation, the location and size of the existing tunnels, and the quality of the bone, the surgeon must be prepared to use a number of different techniques.
The revision surgery can be performed all at once (one-stage) or as two separate procedures (two-stage), if necessary. The two-stage surgery ensures adequate healing of bone tunnels, which will then provide a good bed for fixation of the ACL graft without compromising the location of the bone tunnels.23 However, this technique exposes the patient to the inherent risks of two surgeries and the hazards of an unstable knee while waiting for the graft to incorporate, causing meniscal injury or cartilage damage. An obvious advantage of the one-stage surgery is to avoid the need for a second surgery. For the technique to be successful, it requires good bone quality with acceptable tunnel size and location or the ability to bypass existing tunnels or fill bone defects with adequate density and strength.3,5,13,17,25 This chapter presents a treatment algorithm based on different scenarios and describes the surgical techniques for both procedures.
Approximately 100,000 to 175,000 ACL reconstructions are performed in the United States annually.6,16,22 With respect to pain relief, stability, and return to function, the reported long-term results after primary ACL reconstruction are 75% to 95% good to excellent.10,27
With an increasing number of ACL reconstructions being performed each year,16 however, there will inevitably be an increasing need for revision procedures. The Danish registry recently published a report indicating that 3% of all ACL reconstructions were revised within the first 2 years.15 Historically, the failure rate of primary ACL reconstructions caused by instability has been reported to be as low as 0.7% and as high as 8% in the United States.8,10,27 Based on our calculations, there are potentially 700 to 14,000 revision ACL procedures to be performed annually in the United States alone.
Chapter 49 addressed the causes of ACL failure and the planning and decision making for revision surgery. One of the most challenging aspects of ACL revision surgery is how to deal with the previous technical errors, methods of fixation, and tunnel widening. Old tunnels may be poorly positioned and interfere with new tunnel location, hardware may block the path of the new tunnel or fixation device, and an enlarged tunnel or large bone defect may jeopardize graft security and incorporation.
Preoperative Workup
Determining the cause of failure is crucial to achieving a successful outcome and avoiding a repeat failure. The most common cause of failure of the primary ACL reconstruction is related to errors in surgical technique.11,14,18,24 A vast majority of the time (70% to 80%), this is caused by nonanatomic tunnel placement.1,20,27 Other technical errors include improper graft tensioning, inadequate fixation, graft impingement, and failure to address unrecognized pathology.
Poor tunnel location results in excessive changes in graft length, plastic deformation, and ultimately failure. It can occur on the femoral and tibial sides (one or both) and in the saggital (too anterior or too posterior) and coronal planes (too vertical or too horizontal). Usually, the femoral tunnel is nonanatomic. Specifically, it is usually placed too far anterior because the posterior femoral cortex is not adequately visualized (Fig. 50-1).9,12
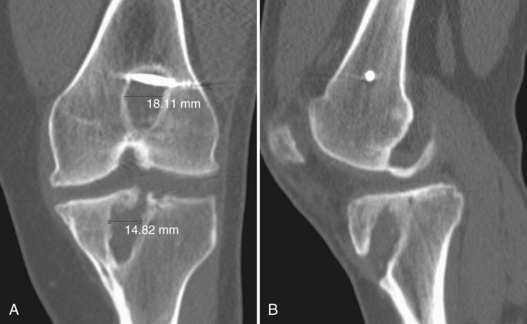
Posteroanterior (PA), lateral, sunrise, and lateral hyperextension radiographic views should be obtained to determine previous tunnel and hardware position, whether tunnel expansion has occurred, and whether any degenerative changes are present (Fig. 50-2). Consider standing views on a long cassette to determine the mechanical axis. If significant bony defects are present on the radiographs, a computed tomography (CT) scan is often beneficial in planning new tunnel placement and to help determine whether bone graft or void fillers will be needed (Fig. 50-3).

Figure 50-2 PA (A) and lateral (B) x-rays of the knee showing tunnel lysis and early degenerative changes.
The hospital or surgery center must have the necessary equipment and implants for the revision surgery (Fig. 50-4). Custom-sized allograft materials should be ordered in advance, if needed. Consider having soft tissue allografts in stock as a backup for unexpected occurrences. A variety of sizes and types of bone graft should be readily accessible (Fig. 50-5). Specific instrumentation (if possible) or a universal screw removal set (Fig. 50-6) should be available to remove the previous hardware. It is also often useful to use fluoroscopic guidance to facilitate removing retained hardware or assist in tunnel placement, especially if one is attempting to bypass the previously placed hardware.
The patient must be appropriately counseled preoperatively about the surgery and expected outcomes. The patient should have realistic goals and understand that the results of revision surgery are less predictable and generally less favorable.4,6,24,27 Occasionally, it is not possible to determine preoperatively whether a one- or two-stage procedure will be performed, and the patient should consent to the possibility of additional surgery if necessary.
Treatment Options
In general, one-stage surgery can be performed in the setting of adequate bone quality and tunnel placement, when the hardware is not in the way. In the ideal scenario, the alignment of the initial tunnels is so malpositioned that the normal landmarks and bone stock will be preserved (see Fig. 50-1). If this is the case, the previous tunnels and hardware can simply be bypassed with new anatomically placed tunnels.17 Frequently, however, it is not this simple.
If small or moderately sized bony defects are present, either caused by tunnel widening or from the removal of previous hardware, these must be addressed intraoperatively. The defect can be filled with autograft plugs7,19 or allograft dowels.3,5 Other techniques use structural grafts, including bioabsorbable interference screws2,13 or calcium phosphate cement,25 to fill the void. These rigid bone void fillers allow new tunnels to be drilled anatomically (without compromising location) and the graft to be securely fixed in one procedure.
Paessler19 has described a technique in which iliac crest corticocancellous autograft bone plugs can be used during a one-stage procedure. The iliac crest graft is harvested through a 2- to 3-cm incision using a specialized harvesting tube. The trajectory for the tube harvester is marked with a Kirschner wire (K wire) passed into the iliac crest. A harvesting tube is used that matches the diameter required for the corticocancellous plug and the plug is removed with a removal device. The harvested plugs can then be inserted into the tunnel defects in an arthroscopic or open fashion.
Battaglia and Miller5 have recommended using cylindric bone allografts, or Cloward dowels, to fill bone voids (Fig. 50-7). The previous tunnel is aggressively débrided and reamed and the corresponding sized dowel is inserted. The most common sizes are 12 mm in diameter by 25 to 35 mm in length, although up to 18-mm diameter dowels have been used successfully. A variety of different sized dowels must be available. This study noted that even with meticulous preoperative planning, the exact size of the defect is often difficult to predict.
A similar technique involves replacing an existing metal interference screw in the femoral tunnel with a bioabsorbable screw.13 If the existing tunnel is partially overlapped by the new tunnel, the reamer can drill through the corner of the absorbable screw; the remaining screw fills the void and provides structural support. The stacked interference screw concept specifically refers to inserting a second interference screw, adjacent to the one providing structural support, to reinforce fixation.2
In a recent study by Vaughn and colleagues,25 the authors performed a cadaveric study to determine the load to failure of a bone-patellar tendon-bone graft (BPTB) placed after filling bone defects with calcium phosphate cement. They found that using standard fixation techniques and anatomically drilled tunnels, the load to failure of the reconstruction using the bone cement was not significantly different from that of the control group, a primary ACL reconstruction with standard interference screw fixation. However, although it has been shown that calcium phosphate bone cement is stronger than cancellous bone, this biomechanical study on cadavers did not necessarily correlate to in vivo results. A significant question that remains is whether the cement would inhibit incorporation of the graft into bone.
Two-stage surgery should be considered for significant widening of the tunnels when tunnels are close but not ideal (causing an hourglass shape or tunnel confluence) and when an excessive amount of bone is removed during the hardware extraction process. Many authors suggest bone grafting and staged revision if the amount of cystic widening (or osteolysis) is greater than 15 mm.1,12 The initial procedure involves removing the existing hardware and filling the bony defects with bone graft. Typically, the bone graft is incorporated over a period of several months. Then, during the second stage, new tunnels can be drilled and the ACL revision procedure can be performed.
A two-stage technique should also be considered in the setting of decreased range of motion (arthrofibrosis) following index ACL surgery. If there is a flexion contracture more than 5 degrees or a flexion loss more than 20 degrees, a manipulation under anesthesia, lysis of adhesions, and aggressive physical therapy should be performed to improve motion prior to revision.12 In addition, a staged revision must be performed in the setting of an underlying infection. Obviously, the definitive reconstruction should be delayed until the infection is eradicated.
Thomas and associates23 have advocated a two-stage procedure if the tibial tunnel from the index procedure would overlap the correctly placed new tibial tunnel either partially or fully. After débriding the old tunnel, bone was harvested from the iliac crest in the form of dowels and impacted in the tunnel. The femoral tunnel was not grafted because it was later drilled in virgin bone via a different technique (outside-in). A CT scan was obtained 4 months later to confirm adequate healing of the bone graft. A revision ACL procedure was then performed similar to a primary procedure.
Acceptable Femoral and Tibial Tunnel Locations