Revision Acl and Pcl Reconstruction
Daniel R. Stephenson
Darren L. Johnson
Anterior cruciate ligament (ACL) injuries are one of the most common sports injuries in the United States. In fact, it is estimated that there are over 200,000 ACL injuries each year (1). As they are such common injuries, ACL reconstruction is one of the most common procedures performed by orthopedic surgeons, at a near similar rate. Injuries to the posterior cruciate ligament (PCL) are considerably less common, with reports that they account for 1% to 30% of all acute knee injuries. They are more often seen in trauma patients than in athletes, but nonetheless pose a risk to knee stability and late degenerative arthritis is left untreated. Of concern with ACL reconstruction is that it is estimated that 85% of ACL reconstructions performed in the United States are done by surgeons that do fewer than 10 ACL surgeries a year (2). Despite this ACL reconstruction is generally considered a good procedure to restore normal or near normal knee stability and kinematics. With this high number of injuries and surgery, there are also a relatively high number of failures that require revision. On the other hand, PCL injuries are less common, less commonly recognized and therefore treated operatively and thus much less frequently revised.
Any surgery can fail for a myriad of reasons, and ACL and PCL reconstructions are no different. One must generally ascertain the reason of failure in order to succeed in the designing a treatment algorithm for operative revision reconstruction. The goal of a revision surgery of either cruciate is to provide a stable and functional knee that will recreate the normal kinematics of the knee. In order to restore normal knee kinematics, our belief is that the ligaments must be reconstructed anatomically, just as one attempts to achieve in fracture management. Increasing research in the past decade has focused on the detailed three-dimensional (3D) and insertional anatomy of the cruciate ligaments. The ACL is now known to have two functional bundles—the anteromedial (AM) bundle and posterolateral (PL) bundle. Likewise, the PCL is also recognized to have two functional bundles—the anterolateral (AL) bundle and posteromedial (PM) bundle. This knowledge and detailed studies as to the exact locations of the femoral origins and tibial footprints of the cruciate ligaments are transforming the approach to the operative reconstruction of these ligaments (3, 4).
How we assess a failure remains somewhat controversial. Some clinical failures are a failure to the patient but may not be to the clinician. An elite athlete who does not return to the same level of performance after surgery, may consider that a failure, whereas a surgeon may feel the kinematics and stability to be acceptable. There are subjective complaints following an ACL or PCL injury such as pain, stiffness, or recurrent instability. These require further investigation as to the source of the problem. Objectively, these complaints may be seen with laxity, degenerative joint disease, and decreased range of motion.
This chapter will discuss the evaluation and treatment of failures of both ACL and PCL reconstruction. Our philosophy is that the restoration of the true anatomic location of the ACL and PCL is critical to restore the function of the knee. We utilize an anatomic double-bundle technique in a majority of our ACL revisions to achieve this. In the setting of a revision PCL reconstruction, the rate of recurrence and rate of reoperation are both low. As such, there is much less known and published in regard to revision PCL surgery. Decisions about graft selection and single-versus double-bundle reconstructions are often individually based on the patholaxity of the involved knee as well as the patients own unique anatomy.
ACL REVISION
Etiology
ACL failures are attributed to an array of causes. To best understand these, we must begin by defining what constitutes a “failure.” Nearly all would agree that a rerupture with patholaxity is a failure. Most would then consider the realm of “clinical failures” as any situation where there is either recurrent instability or significant arthrofibrosis with limitations in range of motion. We would also consider most situations that result in significant pain, which precludes the participation in activities of daily living (ADLs) or the inability to return to level 1 sports as failures. There are also the failures that some would consider
significant, but many would exclude the athlete that returns to their chosen sport but remains at a suboptimal performance level. This group is estimated at nearly 40% of elite athletes and those who participate in level 1 sports year round. These are the outcomes that are most difficult to quantify or even achieve agreement that they are in fact failures. The literature reports failure rates from 3% to 52%, a large range likely due in part to the poor consensus on what constitutes failure (5).
significant, but many would exclude the athlete that returns to their chosen sport but remains at a suboptimal performance level. This group is estimated at nearly 40% of elite athletes and those who participate in level 1 sports year round. These are the outcomes that are most difficult to quantify or even achieve agreement that they are in fact failures. The literature reports failure rates from 3% to 52%, a large range likely due in part to the poor consensus on what constitutes failure (5).
We generally think of failures in broad categories: (1) recurrent pathologic laxity or instability (including traumatic rerupture), (2) decreased motion or arthrofibrosis, (3) persistent pain, and (4) extensor mechanism dysfunction. There are multiple reasons that a failure can result in any of the above situations. In order to best approach the failed primary surgery, you must begin by knowing which of the etiologic mechanisms caused the particular problem. Armed with this knowledge you can begin to determine the underlying cause, and design a treatment algorithm for that particular patient.
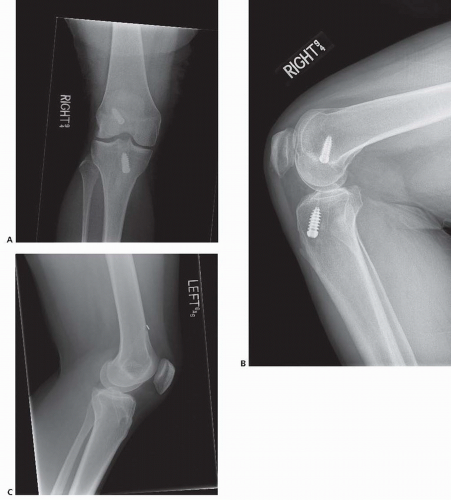
When examining recurrent instability, there are four major reasons for failure. The most likely cause of failure is technical error—most commonly nonanatomic tunnel placement. Battaglia et al. (6) estimate that 70% to 80% of failures are a result of nonanatomic tunnels. There are various forms of tunnel malpositioning; the most common being vertical tunnels (Fig. 79.1). This occurs when the tibial tunnel is too posterior and the femoral tunnel is more central in the roof of the intercondylar notch often from transtibial single incision ACL surgery. The resulting complaint tends to be related more toward rotational instability, rather than complaints of anterior posterior instability. On physical examination, this patient may have a positive pivot-shift in light of a negative Lachman’s or Anterior Drawer test (7, 8). We find this error is most commonly seen in ACL reconstructions performed via a transtibial technique versus creating femoral tunnels through the accessory anteromedial (AAM) portal or twoincision technique. Error in tunnel placement can also be attributed to inadequate visualization due to portal placement. While a large notchplasty may not be required in all patients, enough must be removed to allow adequate visualization of native anatomic bony landmarks.
A second cause of recurrent instability that is commonly encountered is the failure to address other injuries, such as meniscal injuries, injury to the medial collateral ligament (MCL), posterior oblique ligament (POL), or posterolateral corner (PLC) including the popliteal fibular ligament, and the fibular collateral ligament. It is estimated that 15% of ACL failures occur because of the failure to recognize or treat concomitant injuries (9). This will cause nonphysiologic strain on the graft and ultimately end in graft attrition and surgical failure in the relative short term. Third, there are failures associated with fixation. This can be frank failure, or error in the tensioning of the graft, these are much less common but may occur. Graft-tunnel mismatch and interference screw divergence are the most common technical errors. Finally, there is the true traumatic rerupture. This is perhaps the hardest to prevent, as often times it is a result of the player in the wrong place at the wrong time. The caveat to this would be the use of bracing in downhill skiers. This has shown to be protective of further injury. The use of bracing has not shown to be beneficial in the prevention or recurrence of ACL injuries in the majority of athletes.
The next major category to examine is that of stiffness or decreased range of motion. One of the most difficult problems to address after ACL reconstruction is the loss of terminal extension. Patients that are unable to fully extend their knee (even 5° from full extension) often complain of significant discomfort and functional disability. This is one area where being aggressive with range of motion therapy in the 1st month after surgery is crucial. Difficulty with flexion is much less commonly seen and more functionally tolerated. Flexion deficits tend to achieve better resolution with manipulation and lysis of adhesions. Aside from these issues, there are other reasons that range of motion may be affected. Certainly, the “cyclops lesion” is of concern. This is created by scarring of the tibial stump in the intercondylar notch if the athlete does not get full extension within the first 2 weeks, which may then prevent full extension. This, however, is easily treated with arthroscopic debridement. Nonanatomic tunnels may also contribute to decreased range of motion. The phenomenon of a “captured knee” is generally associated with a femoral tunnel that is too far anterior—thus creating what is effectively a shortened graft. The third major cause of loss of motion is arthrofibrosis. These patients have generally lost greater than 10° of knee extension and more than 25° of knee flexion, with decreased patellar mobility. Failure to recognize this condition, and its associated swelling and inflammation can result in infrapatellar contracture and patella baja. It is also important to distinguish between primary or iatrogenic arthrofibrosis and secondary arthrofibrosis (acute surgery, technical errors, delayed rehabilitation) (10). Primary arthrofibrosis is a diagnosis of exclusion, and other causes must be ruled out. Management focuses on therapeutic exercises and modalities to regain patellar mobility and passive stretching. Secondary arthrofibrosis is generally preventable by performing surgery at the proper time, with proper technique and adequate, early rehabilitation. Primary surgery should generally be delayed at least 3 weeks from injury, with adequate decrease in swelling and inflammation. Surgery performed in this period of acute inflammation may actually accelerate the healing process, resulting in increased fibrotic scar formation. In regard to arthrofibrosis, it is important to distinguish between primary or iatrogenic arthrofibrosis and secondary arthrofibrosis (acute surgery, technical errors, delayed rehabilitation).(10) Primary arthrofibrosis is a diagnosis of exclusion, and other causes must be ruled out. Management focuses on therapeutic exercises and
modalities to regain patellar mobility and passive stretching. Secondary arthrofibrosis is generally preventable by performing surgery at the proper time, with proper technique and adequate early rehabilitation. Primary surgery should generally be delayed at least 3 weeks from injury, with adequate decrease in swelling and inflammation. Surgery performed in this period of acute inflammation may actually accelerate the healing process, resulting in increased fibrotic scar formation. Less common causes of decreased range of motion include simultaneous additional ligament surgery, complex regional pain syndrome, poor rehabilitation compliance, and prolonged immobilization.
modalities to regain patellar mobility and passive stretching. Secondary arthrofibrosis is generally preventable by performing surgery at the proper time, with proper technique and adequate early rehabilitation. Primary surgery should generally be delayed at least 3 weeks from injury, with adequate decrease in swelling and inflammation. Surgery performed in this period of acute inflammation may actually accelerate the healing process, resulting in increased fibrotic scar formation. Less common causes of decreased range of motion include simultaneous additional ligament surgery, complex regional pain syndrome, poor rehabilitation compliance, and prolonged immobilization.
The third major cause of failure of ACL reconstructions is extensor mechanism dysfunction. There are a variety of problems that can affect the function of the extensor mechanism; the most catastrophic is a patellar fracture. This can be seen most often with technical error associated with bone-patellar tendon-bone (BTB) and quadriceps autografts. Another problem that can arise with ACL reconstructions is anterior knee pain, which is most often
associated with BTB autograft. This complication can often be prevented by getting the patient into aggressive postoperative rehabilitation immediately after surgery. The rehabilitation program should focus on the restoration of patellar mobility including maintenance of patellar glide and patellar tilt symmetric to the uninvolved knee. Finally, there can be problems that occur due to general quadriceps weakness. Specifically, weakness in the vastus medialis (VMO) can result in patellar maltracking and be problematic in the first 2 months of rehabilitation. Fortunately, this is a problem that is treated with reassurance and continued work in therapy.
associated with BTB autograft. This complication can often be prevented by getting the patient into aggressive postoperative rehabilitation immediately after surgery. The rehabilitation program should focus on the restoration of patellar mobility including maintenance of patellar glide and patellar tilt symmetric to the uninvolved knee. Finally, there can be problems that occur due to general quadriceps weakness. Specifically, weakness in the vastus medialis (VMO) can result in patellar maltracking and be problematic in the first 2 months of rehabilitation. Fortunately, this is a problem that is treated with reassurance and continued work in therapy.
The fourth and final major source of failure is degenerative joint disease. This is an issue that can arise in the 1st year (most often if there is an isolated chondral defect or menisectomy) or with time. Chondral injuries generally will require a second operative intervention to help restore the cartilage surface, which is beyond the scope of this chapter. Several studies have shown that ACL deficient knees can have radiographic evidence of osteoarthritis in greater than 50% of patients in 5 to 15 years after injury, but many of these are poorly designed studies, and the natural history has not been well studied particularly with current anatomic ACL techniques. Neuman et al. (11) found that there was a 16% incidence of radiographic knee OA 15 years after injury, with that number decreasing to 14% in patients less than 30 years of age. More indicative is the presence or absence of meniscal injury, where rates approach 44% after menisectomy 10 years after reconstruction (12). Graft selection has not been shown to be associated with development of osteoarthritis (13). Patients may also present with unicompartmental arthritis (most often in the medial compartment), or tricompartmental arthritis, generally several years down the road. This patient population presents a unique challenge based on the age of the patient, as options may range from conservative measures to a partial or total joint arthroplasty.
Preoperative Evaluation and Planning
As with most evaluations, it is crucial to begin with a thorough history and physical examination. Begin with discussing the initial injury, surgery, and rehabilitation. When discussing the issues with your patient, it is important to discern the following: What was chronicity of the problem? Was there or was there not a traumatic event? Did the onset of symptoms develope late after ACL reconstruction or in the immediate postoperative period? It is important to know whether the patient ever made it back successfully to level 1 ACL dependent sports and if so, for how long? Often times this will let you start focusing on whether you are looking at a technical error, biologic problem, or at simply bad luck. It is also important to discuss what the patient is or is not able to do, and their expectations of the activities they would like to return to. Are the patients complaints related more to pain or to instability or a combination of both? This will help to assess if a revision is the correct treatment, as patients with pain may not have a problem that can be addressed by a revision surgery. In regard to instability, we have found that patients with instability will often describe the “double fist” sign. This is when they make a fist with both hands and show the knee feels like the two fists rotating against each other. This is almost always indicative of rotatory instability or a knee that will have a remarkable pivotshift in surgery. It is also important to try to obtain any operative notes and intraoperative photographs to determine the plan of action. The Multicenter ACL Revision Study group recently reported that a mere 10% of patients will have normal articular cartilage or menisci when they undergo revision surgery (14). Armed with this information, the surgeon can begin to effectively plan for revision surgery treatment alternatives. This includes equipment, potential pitfalls (fixation, grafts, bone loss), and the expectation of the surgeon and the patient in regard to the outcome if surgical treatment is considered.
Physical Examination
For revision ACL reconstructions, it is crucial to perform a complete physical examination. Initial observation will allow the surgeon to see prior incisions, generally alignment and any gait abnormalities, which may show a varus or valgus thrust. The range of motion and tests for extensor mechanism dysfunction should be performed to assess for any potential adversity they may cause in regards to revision surgery and graft selection. The range of motion is best objectively measured with the patient in the prone position, and patellar mobility (glide and tilt) is compared with the uninvolved extremity. Furthermore, one needs to not only assess the stability of the ACL, but also any laxity relating to the MCL, PLC, PM corner, and the menisci. Having an idea of concomitant injuries will help assessment of additional procedures that may need to be addressed. This is the time to begin explaining the current understanding of the involved injuries to the patient. But it is also important to stress that during the examination under anesthesia, in the operating room, other injuries may be detected that should be addressed, for example, most patients will not permit a good pivot-shift exam in the office setting, which would help in determining the degree rotatory instability, which may influence your specific anatomic technique.
Imaging Studies
The work-up of the knee after previous ACL reconstruction also includes a return to basic imaging studies. Getting an anteroposterior (AP), lateral, Merchant or sunrise, and posteroanterior weight-bearing view with 45° of flexion (Rosenberg view) are routine. This will help to identify the majority of concerns. One can assess tunnel placement, location and type of hardware, degenerative joint disease, tunnel lysis, and notch geometry (15). By beginning with plain films, much needed information can be obtained,
and may help exclude the need for advanced imaging. If there is a high index of suspicion of additional pathology or significant tunnel widening, MRI or CT may be indicated. A CT is generally more useful when there may appear to be significant tunnel lysis to aid in determining the degree of bone loss. The use of newer technology, such as 3D reconstructions, may be of the greatest value when there is a concern for lysis or tunnel positioning. When there is more a suspicion of missed on new injury to the menisci, articular cartilage, or other ligaments in the knee, MRI tends to be of greater value. MRI should not be used to diagnose an ACL failure but can be used to confirm the clinical diagnosis. Based on the plain films, MRI and CT scans, one can usually determine if anatomic graft placement is possible or whether a staged surgery is required. On occasion, it may also be required to get full-length hip-to-ankle standing films if there is concern that limb malalignment may have contributed to the graft failure. Once all the appropriate studies have been gathered and analyzed, focus can turn to the surgery.
and may help exclude the need for advanced imaging. If there is a high index of suspicion of additional pathology or significant tunnel widening, MRI or CT may be indicated. A CT is generally more useful when there may appear to be significant tunnel lysis to aid in determining the degree of bone loss. The use of newer technology, such as 3D reconstructions, may be of the greatest value when there is a concern for lysis or tunnel positioning. When there is more a suspicion of missed on new injury to the menisci, articular cartilage, or other ligaments in the knee, MRI tends to be of greater value. MRI should not be used to diagnose an ACL failure but can be used to confirm the clinical diagnosis. Based on the plain films, MRI and CT scans, one can usually determine if anatomic graft placement is possible or whether a staged surgery is required. On occasion, it may also be required to get full-length hip-to-ankle standing films if there is concern that limb malalignment may have contributed to the graft failure. Once all the appropriate studies have been gathered and analyzed, focus can turn to the surgery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree