Fig. 24.1
MR of an instability repair after 6 months
Ideal Criteria for Return to Play
No pain
Patient subjectivity
Normal ROM
Near normal strength
Normal functional ability
Normal sport-specific skills
Whether the stabilization is performed by arthroscopy (or open), the athlete likely will need a minimum 14–16 weeks before being ready to return. Typically, the time range for return is from 4 to 6 months and it may take as long 9–12 months: we must distinguish that return to sport is sometimes different than return to competition or game.
Protocols vary for sling use after surgical stabilization, but most use a time frame of about 6 weeks. During this time, the athletes begin on range of motion and some strengthening exercises; again, this is dependent on surgeon preference. As soon as the athlete is out of the sling, more aggressive rehabilitation begins, and neuromuscular training is instituted.
Kim et al. [16] randomized 66 patients who had received arthroscopic Bankart repair into two different therapy protocols. Group 1 had pillow sling immobilization for 3 weeks, followed by pendulum and forward elevation using a pulley. At 4 weeks, external rotation strengthening started, but ER was prohibited. At 6 weeks, ER strength started. At 9 weeks, they allowed more vigorous exercise. Group 2 had sling in sleep only for 2 weeks. Forward elevation was limited to 90° for 2 weeks, and at 4 weeks, full range of motion was allowed but extreme external rotation should be avoided. There was no recurrence in either group but two patients in each group had positive apprehension. This article supports the concept that immobilization need not be extended in many cases after arthroscopic stabilization.
The rehabilitation process must be individualized, because each patient will progress at different level due to quality of tissue health, speed of healing response, adequacy of fixation, number of dislocations, bone defect if present, and type of procedure performed.
It is very important to analyze the patient, his history and motivations, his psychology, and if he plays a professional sport.
Generally, the postoperative rehabilitation can be divided into four phases (see Table 24.1, from 1 to 3).
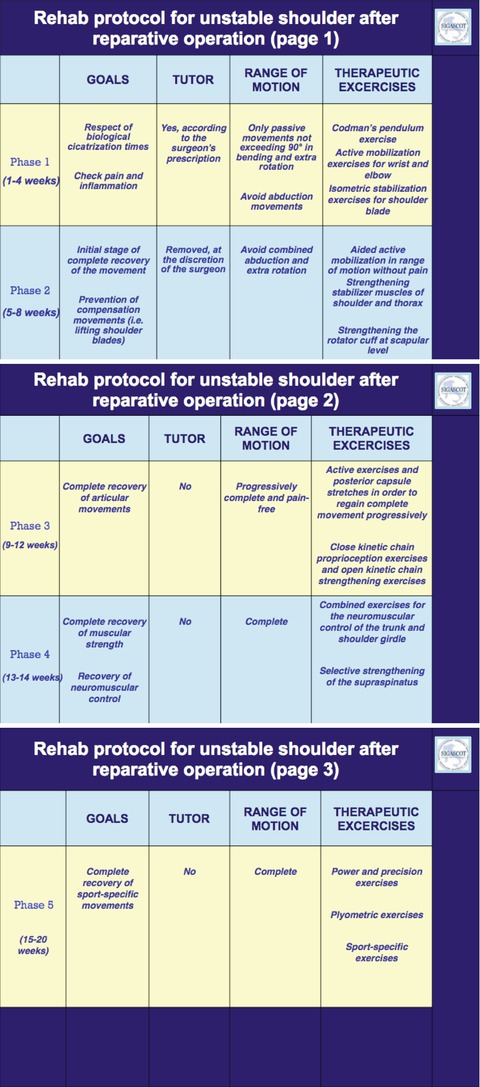
Table 24.1
Instability repair rehab program
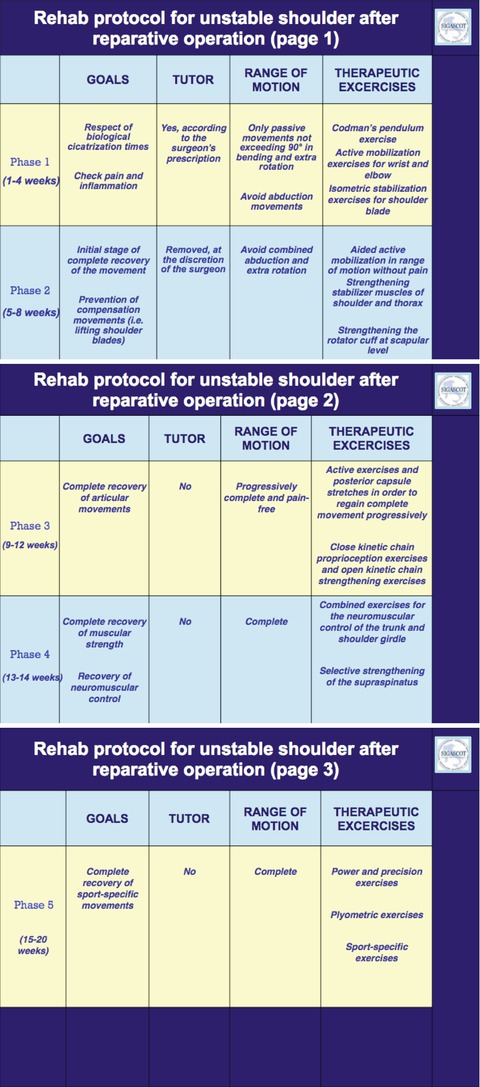
From the fourth to the sixth month (shoulder sport return rehabilitation phase), the full range of motion including stressless ER without loading is allowed. Return to play exercises for the integration of sensorimotor system (proprioception, kinesthesia) and strengthening of synergetic force couple are performed for the functional sport. From the sixth month, stressful exercises for the anterior-inferior capsular labrum complex during rehabilitation and practice are performed for return to play transition. After an adequate return to play transition, the resumption of previous shoulder-dependent sport is allowed (shoulder sport phase).
Ultimately, a careful clinical exam of the patient by the physician is essential before giving clearance for return to sport. It is crucial for the staff to determine how the athlete has achieved appropriate isokinetic strength as well as how he learned any mental skills.
The importance of appropriate rehabilitation cannot be overemphasized.
As the athlete progresses in rehabilitation, goals for return to play are full pain-free functional range of motion, normal strength and endurance, and no apprehension. Once an athlete demonstrates that he is physically and mentally ready, the return may take place.
Murray and Mc Birnie [17] report that surgery achieved successful stabilization in 88 % of patients but only 51 % returned to full sport activity. Patients aged 30 years or under were twice as likely to return to their pre-injury level of sport than those aged over 30 years. Half of those patients who felt unable to return to sport had no subjective symptoms of instability or other physical symptoms related to their shoulder but were inhibited by fear of further injury. In order to increase the number of athletes returning to sport following primary arthroscopic stabilization of the shoulder, those patients with no restrictive symptoms should be encouraged to return to full activity.
Solomon and Provencher [18] report that after instability surgery, the results are generally excellent with appropriate rehabilitation gated toward functional- and sport-specific activities accomplished prior to return. The range for this therapy is about 3–20 months, with most able to return by 6–8 months depending on several factors, such as sport or position played and specific shoulder structures injured and repaired. Often, it can be difficult to define “safe to return” and maximal medical improvement. The decision process for how best to treat an athlete after shoulder dislocation must include a discussion of limitations, anticipated activities, and goals with athlete, parents, trainer, therapist, coach, and surgeon, sometimes also with the manager.
24.2 Multidirectional Shoulder Instability
Historically, open capsular shift techniques have been the standard in the operative treatment of patients with MDI. More recently, however, a number of arthroscopic techniques have been described for treatment of MDI. These techniques include thermal or radiofrequency capsular repair/shrinkage, as well as other arthroscopic approaches using suture techniques and/or suture anchors and the rotator interval closure.
The postoperative rehabilitation and return to sport in MDI after arthroscopic stabilization depend on many factors: first, quality of the tissue and capsula and, second, the type of sport.
Immediately after surgery, the rehabilitation protocol employed the use of an ultra sling brace (DonJoy, Carlsbad, California) that immobilized the shoulder in approximately 30° of abduction and protect the shoulder joint. On the first postoperative day, the patient begins active wrist and elbow flexion and extension exercises as well as gentle pendulums and passive scaption exercises. Patients are immobilized for 4–6 weeks depending on the amount of postoperative stiffness seen at follow-up. After sling immobilization is discontinued, gentle passive ROM exercises are advanced and active assisted ROM exercises are initiated. Range of motion is progressed to full passive and active ROM by 2–3 months postoperatively. At this time, capsular stretching exercises are started and isotonic strengthening continued, with emphasis on rotator cuff. At 4 months postoperatively, patients are progressed into the functional phase of rehabilitation with plyometrics, more aggressive strengthening, and overhead lifting as tolerated. In general, athletes must have painless ROM, strength, and endurance comparable with that of the contralateral side before return to competition. Depending on the sport, most athletes are allowed to return to competition at or around 6–8 months postoperatively.
24.3 Acute Traumatic Posterior Shoulder Dislocation
First described in 1838 by Sir A. Cooper [19], traumatic posterior dislocation of the shoulder represents an unusual and challenging clinical problem. These injuries account for 2–5 % of all shoulder dislocations [19]. Seizures, high-energy trauma, and electrocution are associated with a much greater risk of posterior dislocation [19–21]; diagnosis is missed or delayed in up to 79 % of patients [20, 21]. Early identification of these dislocations reduces morbidity and facilitates treatment.
The treatment can be open (McLaughlin procedure, modified McLaughlin procedure, anterior approach and bone grafting, posterior open Bankart procedure, arthroplasty) or arthroscopic.
In rehabilitation, regardless of management type, the shoulder is braced in 20° of external rotation and abduction for 4 weeks to aid healing of posterior capsule. Pendulum exercise and elbow range of motion three times per day are encouraged. At 4 weeks, unlimited progressive range of motion is initiated as well as isometric posterior rotator cuff strengthening. Noncontact sports are allowed 3 months after reduction or surgery, and contact sports are permitted 4–6 months postoperatively [22].
24.4 Posterior Instability of the Shoulder
Posterior shoulder instability has an incidence between 2 and 12 % in all cases of shoulder instability [23]. While posterior instability is relatively uncommon when compared with anterior instability, it has become increasingly more recognized as a challenging condition in athletic populations. Posterior shoulder instability includes a continuum of pathological changes ranging from a chronic locked posterior dislocation to the more common recurrent posterior subluxation. Athletes typically develop posterior shoulder instability secondary to repetitive, sport-specific motions, which inflict minor traumatic stress to the posterior capsular labrum complex.
Many operative procedures have been described for the treatment of posterior instability, but today, the arthroscopic capsular labrum reconstruction is an effective and reliable procedure (with or without anchors).
24.4.1 Postoperative Rehabilitation and Return to Sport
Immediately after surgery, the rehabilitation protocol employed the use of an ultra sling (DonJoy, Carlsbad, California) that immobilized the shoulder in approximately 30° of abduction while preventing internal rotation. The sling is used for 4–6 weeks depending on the amount of capsular laxity found at time of the surgery. On the first postoperative day, the patient begins active wrist and elbow flexion and extension exercises as well as gentle pendulums and passive scaption exercises. After the sling immobilization is discontinued at 4–6 weeks postoperatively, gentle passive ROM exercises are advanced, and gentle, pain-free internal rotation is allowed. Active assisted ROM exercises and isometric internal and external rotation exercises are also initiated at this time. By 2–3 months postoperatively, the patient progress to full passive and active ROMs. At this time, capsular strengthening exercises are also instituted and isotonic strengthening continued, with the emphasis on the rotator cuff and the posterior deltoid. At approximately 6 months postoperatively, isokinetic testing is performed. Once the patient is able to achieve 80 % strength and endurance compared with the contralateral side, a sport-specific rehabilitation protocol can be initiated. In general, athletes are required to achieve full ROM without pain, full strength, and endurance comparable with the contralateral side before return to competition. Most patients can return to competition by 6 months postoperatively. Throwing athletes deserve special consideration and accordingly are placed on a specific protocol in which their throwing distance and speed are closely monitored and slowly advanced over 2–3 months. Once the throwing athlete is able to perform full-speed throwing for 2 consecutive weeks without symptoms, return to full competition is permitted.
24.5 SLAP Lesion
Tears of superior labrum were initially identified and characterized by Andrews et al. [24] in 1985 during the early years of shoulder arthroscopy. A few years later, Snyder et al. [25] coined the phrase “SLAP” tear to identify the anatomic location and orientation of the lesion: “superior labrum anterior to posterior” (Figs. 24.2 and 24.3). It was thought that these lesions were the result of significant traction on the long head of the biceps tendon during the deceleration phase of throwing [26]. More recently, it has been suggested that forces during the late cocking and acceleration phases of throwing may create a “peel-back” phenomena that leads to SLAP [24, 25].
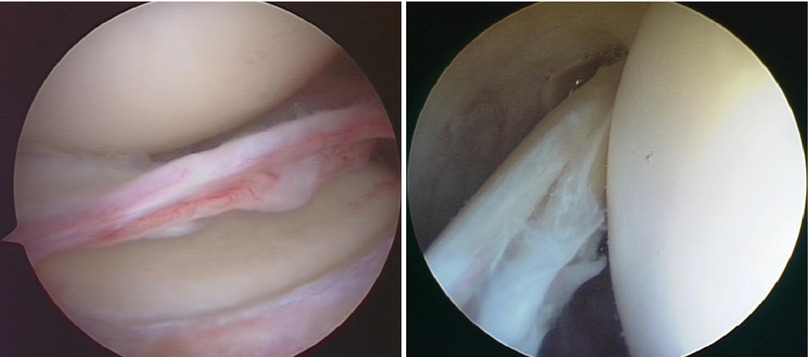
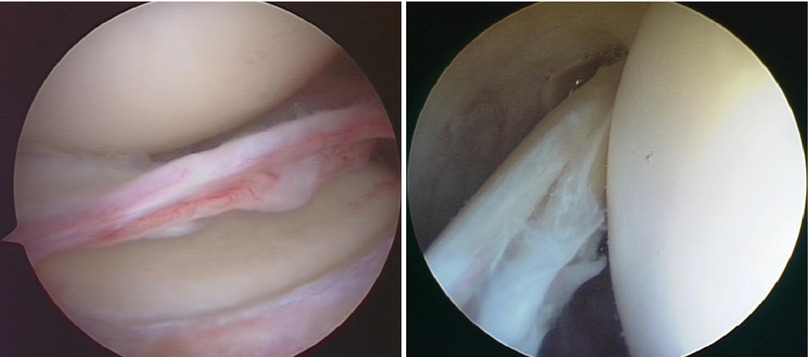
Figs. 24.2 and 24.3
Example of SLAP lesion (type 3 and 4)
While treatment typically begins with a structured therapy regimen, surgery may be necessary in elite and recreational level athletes to allow them to continue in their sport.
After surgery, it is extremely important to protect the biceps/labral complex for 6 weeks postoperatively to allow appropriate healing. Many protocols have been divided into phases. Each phase may vary slightly based on the individual patient and special circumstances.
The overall goals of the surgical procedure and rehabilitation are to:
Control pain and inflammation
Regain normal upper extremity strength and endurance
Regain normal shoulder range of motion
Achieve the level of function based on the orthopedic and patient goals
Early passive range of motion with noted limitations is highly beneficial to enhance circulation within the joint to promote healing. The physical therapy should be initiated within the first week following surgery. The supervised rehabilitation program is to be supplemented by a home fitness program where the patient performs the given exercises at home or at a gym facility.
Important postoperative signs to monitor include:
Swelling of the shoulder and surrounding soft tissue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






