Repair of Peroneal Tendon Tears
Christopher E. Gross
Selene G. Parekh
James A. Nunley II
Mark E. Easley
DEFINITION
Pathology of the peroneal tendons may be due to a singular traumatic episode or recurrent ankle sprains.
In patients undergoing surgery for ankle instability, 25% have peroneal tendon tears; however, the true incidence is unknown.4
Isolated tears of the peroneus brevis and longus are rare.
Delays in diagnosis are common, as up to 40% of peroneal tendon disorders are missed at first evaluation.5
ANATOMY
The peroneus brevis and longus are innervated by the superficial peroneal nerve and reside in the lateral compartment of the leg.
The peroneal longus attaches to the base of the first metatarsal and medial cuneiform and is responsible for plantar flexion of the first ray and eversion. Its muscular antagonist is the tibialis anterior.
The peroneal brevis attaches to the base of the fifth metatarsal and acts to evert and plantarflex the foot. Its muscular antagonist is the tibialis posterior. The brevis often has a low-lying muscle belly.
At the level of the lateral malleolus, the peroneus brevis is directly posterior to the bone; the longus is posterior to the brevis.
Both peroneal tendons are tethered at the level of the lateral malleolus in the fibular groove by the superior peroneal retinaculum, a 1- to 2-cm fibrous sling that extends from the tip of the lateral malleolus to the calcaneus. Disruption of this retinaculum can cause a subluxation of the tendons.
The inferior peroneal retinaculum is continuous with the inferior extensor retinaculum anteriorly and passes obliquely down to insert onto the lateral surface of the calcaneus. At this level, the peroneal tubercle of the calcaneus is a bony ridge that separates the brevis and longus. Injury to the inferior retinaculum does not allow for tendon subluxation.
PATHOGENESIS
The peroneal tendons may be injured in an inversion ankle sprain (FIG 1) or in chronically unstable ankles.
Contributing factors to tearing include tendon subluxation, superior retinacular stenosis,1 a low-lying peroneal brevis muscle belly,7 the presence of a peroneus quartus,17 and tenosynovitis.
The most common location for longitudinal peroneus brevis tendon tears is at the fibular groove,12 whereas the most common location for a peroneus longus tear is at the peroneal tubercle, at the entry of the cuboid tunnel.
At the fibula, both the peroneus longus and brevis have reduced vascularity.13
NATURAL HISTORY
Peroneal tendon pathology can be commonly overlooked in a patient with chronic lateral ankle pain.
Anatomic variants may predispose to peroneal tendon tears. For example, a shallow retromalleolar groove predisposes the peroneals to subluxation or dislocation.15
Peroneal tendons that frequently subluxate or dislocate causes fraying at the tip of the fibula, as the tendons are constantly exposed to abnormal loads.
Additionally, the fibrocartilage of the distal fibula may hypertrophy and cause splitting of the brevis tendon.
PATIENT HISTORY AND PHYSICAL FINDINGS
Patients may present after a severe ankle sprain or chronic lateral ankle instability.
Acute or chronic swelling and pain along the posterior border of the distal fibula is an important clinical indicator of peroneal pathology.
Palpation along the course of the peroneal tendons is important in eliciting pain. Pain at the tip of the fibula is usually due to a tear of the peroneus brevis10 as compared to the peroneus longus tear, which presents as pain close to the base at the fifth metatarsal or cuboid tunnel.
Pain may be associated with active, resisted eversion and ankle dorsiflexion. The patient may also experience subluxation of the tendons with this maneuver.
On eversion strength testing, patients can have considerable weakness and pain.
Alignment of the affected lower extremity must be assessed. A fixed hindfoot varus deformity may need to be corrected at the time of surgery.
The single heel rise is helpful to evaluate the normal inversion (varus) alignment of the hindfoot.
The peroneal tunnel compression test is used to evaluate peroneus longus tears. One applies manual pressure along the peroneal tendon sheath in the retromalleolar groove with the knee flexed to 90 degrees and the foot in a resting plantar flexed position.14 A peroneal longus tendon tear may be present if the first ray does not plantarflex.
Circumduction of the foot may reveal subluxating or dislocating peroneal tendons.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Weight-bearing ankle and foot radiographs must be obtained.
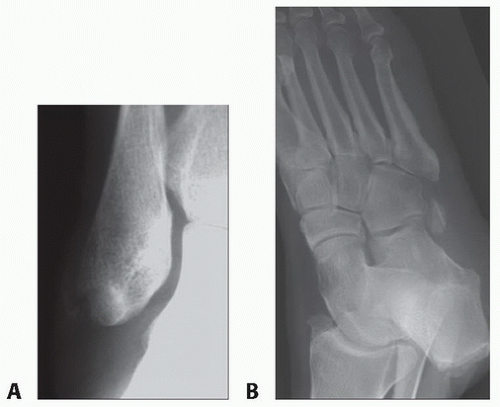
Radiographs may show a “fleck sign” (FIG 2A) at the lateral most border of the fibular tip. This represents an avulsion of the superior peroneal retinaculum and is pathognomonic.6
The os peroneum (FIG 2B), if present, should be identified. Any fragmentation or displacement of this sesamoid may indicate peroneal longus disruption.
Ultrasonography can identify peroneal tendon tears with 90% to 100% accuracy, 100% sensitivity, and 85% to 100% specificity.8,11,16
DIFFERENTIAL DIAGNOSIS
Stress fracture of fibula, cuboid, or fifth metatarsal
Lateral ankle instability
Acute fracture of os peroneum or lateral process of the talus
Ankle or syndesmosis sprain
Talar osteochondral lesions
Sinus tarsi syndrome
Calcaneocuboid syndrome
Degenerative joint disease
Accessory muscle/bone
Hypertrophic peroneal tubercle
Sural neuritis
NONOPERATIVE MANAGEMENT
Functional rehabilitation includes range of motion for the ankle and hindfoot, concentric and eccentric muscle strengthening, endurance training with particular attention to the peroneal musculature, and proprioceptive exercises.
Functional bracing or taping may be useful to help prevent recurrent injury during “at-risk” activities.
The senior author avoids performing corticosteroid injections to avoid any unnecessary risk of causing rupture or further damage to the tendons.
SURGICAL MANAGEMENT
Preoperative Planning
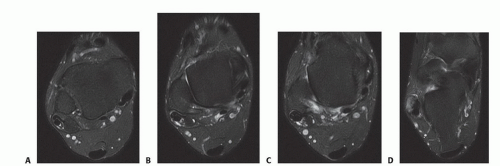
All imaging studies must be reviewed so that the location of the lesion is identified. MRI is often useful in identifying the exact level of peroneal tendon pathology.
Plain films must be reviewed for associated pathology, including degenerative changes, malalignment, and fractures. The ankle radiographs may reveal an avulsion of the superior peroneal retinaculum.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree