Repair of Dislocating Peroneal Tendons: Perspective 1
Sheldon Lin
Karl Bergmann
Vikrant Azad
Virak Tan
Enyi Okereke†
Siddhant Mehta
† Deceased.
DEFINITION
Subluxation or dislocation of the peroneal tendon is a relatively uncommon injury, with the majority of the cases attributed to a traumatic event. Chronic subluxation has also been reported without any history of a specific event.
Numerous surgical procedures have been described for the treatment of peroneal tendon subluxation, which may be classified into three categories: primary repair, soft tissue augmentation, and bony reconstruction.
Primary repair of the superior peroneal retinaculum (SPR) is a commonly used surgical procedure. However, the effectiveness of primary repair depends on the quality of the retinaculum and its ability to contain the peroneal tendons. When the SPR tissue is deficient or insufficient, then other procedures are necessary.
Soft tissue procedures other than primary repair involve the augmentation of tissue already present or the rerouting of tissue from other structures to recreate the SPR.
Bony procedures attempt to recreate a more stable fibular sulcus by deepening the fibular groove or extending the fibular rim. In this chapter, we present a soft tissue augmentation procedure using a periosteal-based flap of the retrofibular sulcus.
ANATOMY
Along the lateral aspect of the lower leg, there are two muscles in the lateral compartment, the peroneus longus (PL) and peroneus brevis (PB). These two muscles arise at the proximal fibula and become tendinous before crossing the ankle.
The peroneal tendons are contained in a single sheath located posteriorly and immediately distal to the fibula. Roughly at the level of the peroneal tubercle on the lateral calcaneus, the tendons separate into separate sheaths. The PB muscle belly extends more distal than the PL and it becomes tendinous about 1.5 cm before the tip of the fibula. The PB tendon lies directly posterior to the fibula and anteromedial to the PL tendon as the two tendons course behind the fibula.
The peroneal tendon sheath comprises the SPR, the calcaneofibular ligament (CFL), and the fibular sulcus. Respectively, the fibular sulcus represents the anterior border, the SPR the lateral border, portions of the SPR and CFL the posterior border, and portions of the CFL and posterior talofibular ligament the medial border of the peroneal tendon sheath.12
The PB inserts on the dorsal base of the fifth metatarsal, whereas the PL courses lateral to medial on the plantar aspect of the foot and inserts on the lateral sides of the base of the first metatarsal and medial cuneiform bones.
The SPR is the primary restraint against subluxation of the peroneal tendons within the fibular groove. The SPR can have an extremely varied anatomy, with differences in width, thickness, and insertional patterns. Most commonly, the SPR inserts into both the Achilles tendon and the calcaneus.3 There is no distinct insertion point of the SPR; instead, it blends into the periosteum of the fibula.
The anatomy of the fibula is varied as well. About 50% of fibula have a bony ridge about 2 to 4 mm that augments the fibular sulcus.2 A cadaveric study by Edwards5 found that 82% of the time a sulcus was present at the posterior edge of the distal fibula. The average sulcus dimension was 3 mm deep and 6 mm wide. He found that 11% of the cadavers had no groove and that 7% of the cadavers had a convex fibula. A fibrocartilaginous rim was deficient in 48% of all cadavers and was absent in 30%.
PATHOGENESIS
According to Zoellner and Clancy,16 in acute injury, the peroneal tendons tend to dislocate anteriorly over the lateral malleolus in people who have an anatomic predisposition. The fibular groove that serves as the pulley for the tendons can be shallow or convex and the SPR may be absent or lax. A low-lying PB muscle belly can also cause subluxation (FIG 1). In a study of the effect of a low-lying PB muscle belly, Geller et al7 measured the location of the musculotendinous junction (MTJ) in 30 cadaveric specimens with respect to the fibula tip and peroneal tubercle and also the width of the PB tendon. The PB MTJ was significantly more distal and the tendons had a significantly greater diameter in torn (4 of 30) versus untorn (26 of 30) specimens (Table 1). The authors suggested that the location of the PB MTJ may have an influence on the development of degenerative tears.
Recurrent dislocations are the result of an inciting acute traumatic episode of forceful ankle dorsiflexion with a simultaneous powerful contraction of the peroneal muscles that causes failure of the SPR. The dorsiflexion causes the SPR to tighten, thereby decreasing its diameter. This force is theorized to cause the retinaculum to be avulsed from its periosteal attachment. Eckert and Davis4 stated that the SPR’s attachment on the edge of the fibula does not adhere to a strong band of collagen, but instead blends into the periosteum of the lateral malleolus. They proposed that this weak insertion point is responsible for tendon dislocation secondary to avulsion of the fibular fibrocartilaginous lip and stripping of the SPR from the fibula.
The prototypical mechanism is in skiers as they forcefully con tract the peroneal muscles to grab the ski edge into the snow.

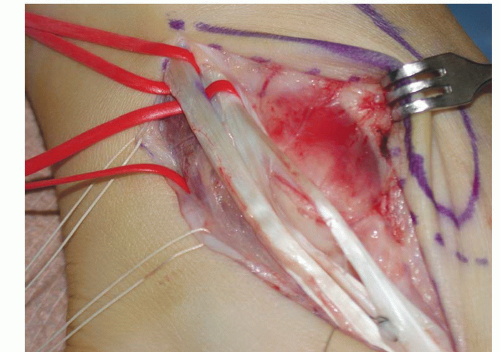
FIG 1 • A,B. Anatomic dissection of a peroneus muscle belly that is too distal. Note the distance to the fibular tip.
Eckert and Davis4 classified SPR injury into three different grades according to severity:
Grade 1 injury: separation of the retinaculum from the cartilaginous lip and the lateral malleolus
Grade 2 injury: The distal 1- to 2-cm dense fibrous lip is elevated along with the SPR.
Grade 3 injury: avulsion of a thin fragment of bone along with the collagenous lip attached to the deep surface of the SPR and deep fascia (Radiographically, this may be represented by a “fleck sign.”)
In grade 1 injuries, the peroneal tendons are easily reducible and are unstable under tension only.
In grade 2 and 3 injuries, the peroneal tendons fail to remain reduced even without tension.
Normally, the peroneal tendons are contained within the fibular sulcus by the SPR.
NATURAL HISTORY
Based on our experience, symptomatic recurrent subluxation does not resolve spontaneously.
Often, peroneal tendon dislocation continues to be misdiagnosed as a chronic ankle sprain. As the tendons dislocate and relocate, direct tendon injury occurs due to repetitive trauma.
Table 1 Low-lying Muscle Belly of Peroneus Brevis and Its Relationship to Peroneus Brevis Tears
Specimen Data
Average Distance to Fibula Tip (cm)
Average Distance Peroneal Tuberosity
Average Width (cm)
No tear (n = 26)
1.62 ± 1.38
3.39 ± 1.3
1.19 ± 0.37
Tear (n = 4)
0.04 ± 1.51
2.13 ± 0.83
1.44 ± 0.39
Zone 1 tendon injuries occur at the fibular groove and usually involve the PB tendon. The action of the PB tendon snapping over the sharp ridge of the fibula leads to a longitudinal tear within the tendon substance (FIG 2).
Zone 2 injuries occur distal to the fibular tip, usually affecting the PL tendon. These injuries are caused by the PL coursing over the lateral wall of the calcaneus and turning 45 degrees at the cuboid facet. As the tears propagate, an inflammatory response may lead to tenosynovitis, tendinopathy, and potential tendon rupture. Peroneal tendon subluxation and dislocation is thought to accentuate the symptoms.
PATIENT HISTORY AND PHYSICAL FINDINGS
The patient may not be able to recall a traumatic event preceding the usual complaints of lateral ankle swelling and pain posterior to the lateral malleolus. Most patients report that the pain radiates proximally. Patients complain of persistent lateral ankle pain and swelling with a sensation of snapping or popping and may note a “pop” laterally before the tendon gives way.
On physical examination, the lateral ankle will be swollen and tender and may be ecchymotic in the acute setting. This can easily be confused with a lateral ankle sprain (Table 2), but the location of the pain may be used to differentiate between the two. Tenderness posterior to the fibula is indicative of peroneal tendinopathy; in contrast, tenderness at the anterior distal fibula suggests an anterior talofibular ligament injury (ankle sprain). However, because the CFL is the floor of the peroneal tendon sheath, there may still be some confusion with more severe ankle sprains. A negative anterior drawer test and pain experienced when the foot is stressed against resisted eversion are more indicative of an injury to the SPR.
Peroneal tendon subluxation test: In the prone position, with the knee flexed to 90 degrees, ankle dorsiflexion and forced hindfoot eversion against resistance is performed. Apprehension and peroneal tendon subluxation or dislocation with this provocative maneuver typically confirms the diagnosis.8
Table 2 Clinical Differentiation of Ankle Subluxation from Ankle Sprain
Signs and Symptoms
Subluxation
Sprain
Tenderness
Proximal to tip of fibula
Distal to tip of fibula
Swelling
Posterolateral
Anteroinferior
History
Snapping
Giving way
Worse on uneven ground?
Possible
Probable
Worse on circumduction?
Yes
No
Worse on flexion-inversion?
No
Yes
Acutely dislocated peroneal tendons are occasionally seen on physical examination, but more commonly, the tendons are reduced upon presentation and are dislocated only with the peroneal tendon subluxation test.
Likewise, chronic peroneal tendon subluxation or dislocation may not present with the tendons frankly dislocated.
Chronic subluxation and dislocation are generally best diagnosed by testing the ankle through a range of motion of inversion and plantarflexion to maximum eversion and dorsiflexion with resistance.
Peroneal compression test: direct compression of the peroneal tendon sheath to identify peroneal tendon injury
IMAGING AND OTHER DIAGNOSTIC STUDIES
Standard weight-bearing ankle radiographs (anteroposterior [AP], lateral, and mortise) define the bony ankle anatomy alignment. In cases of peroneal tendon subluxation, radiographs are usually negative. In a grade 3 injury, a “fleck” of bone can be seen off the posterior distal fibula and is considered pathognomonic of an SPR injury (FIG 3).
Magnetic resonance imaging (MRI) affords detail of the soft tissues. Injury to the SPR, the peroneal tendons, or other supporting tissues may be identified: Anomalous structures such as the peroneus quartus or a low-lying PB muscle belly may be suggested (FIG 4). An MRI is useful for preoperative planning, as other pathology (PB tear, low-lying MJT, fibular sulcus) may also need to be surgically addressed concomitant with repair of the subluxation or dislocating peroneal tendons. We also use MRI to define the morphology of the fibular sulcus. Although MRI may identify dislocated or subluxated peroneal tendons, the tendons are often reduced while the patient is relaxed in the MRI scanner; however, occasionally, dislocated tendons may be identified on axial MRI views.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree