Chapter 34 Rehabilitation of the Elbow
Introduction
Epidemiological studies report the incidence of elbow pain in the general population as being between 8% and 12%.1 The elbow has proved to be the ‘poor relation’ in terms of academic investigation with regards to the effects of rehabilitation as, other than in ‘tennis elbow’, there is a paucity of literature regarding evidence-based management of most elbow pathologies. When considering the role of rehabilitation clinicians must often rely on their knowledge of the pathophysiology of common elbow conditions rather than evidence-based treatment strategies; these continue to remain elusive in the majority of elbow conditions.
This is perhaps reflective of the relatively low incidence of elbow pathology in comparison to the spine, knee and the shoulder (and the natural history of many elbow conditions). Elbow fractures account for only 7% of all fractures and authors report that half of all cases of cubital tunnel syndrome and ulnar neuropathy will resolve spontaneously.2 However, the socioeconomic implications of conditions such as tennis elbow must not be underestimated and emphasize the importance of both understanding and optimizing the role of rehabilitation in managing elbow pathology. While there is currently limited evidence to support the efficacy of rehabilitation in most elbow pathologies, increased understanding of underlying pathophysiology in terms of local tendon pathology, abnormalities in the pain system and impairments in the motor system enable the application of evidence-based rehabilitation strategies.
Background/aetiology
Pain and functional disability are the predominating symptoms that prompt patients to seek treatment.3 Developments in pain science emphasize the importance of considering both peripheral and central mechanisms which will directly impact rehabilitation options. Active trigger points have been identified in the forearm muscles of patients with tennis elbow and are believed to indicate peripheral sensitization; however, the presence of latent trigger points in the unaffected side of patients with unilateral tennis elbow is suggestive of central sensitization processes.4 Similarly the pain pressure threshold is shown to be significantly decreased (by an average of 45–54%) in the affected arm of patients with chronic elbow pain compared to the unaffected arm, but is decreased bilaterally when compared to controls. This provides further evidence of peripheral and central pain hyperalgesia and is suggestive of altered processing within the neuraxis (spinal or supraspinal centres).5 This central sensitization is illustrated by the widespread distribution of reduced mechanical pain threshold beyond that of the original site of symptoms. This indicates that symptoms of lateral and medial elbow pain can arise from the cervical spine and neural tissues, which are neurologically related but not local to the injured tissue site. Modern rehabilitation approaches must consider both peripheral and central pain mechanisms to ensure that treatment is directed appropriately.
It has been suggested that the pain associated with some chronic elbow conditions may relate to altered neuronal afferent input to the cervical spine.6 It is, however, difficult to elucidate the true nature of this relationship as many studies on common elbow pathologies such as tennis elbow exclude patients with significant cervical spine signs. Studies have reported an incidence of cervical or thoracic spine pain in up to 70% of subjects with lateral elbow pain compared to 16% of controls.7 Furthermore, several studies report that mobilization techniques addressed to the cervical spine in patients with lateral elbow pain produce a significant hypoalgesic effect and a concomitant sympathoexcitatory response at the elbow when compared with placebo or control groups.8 Interestingly treatment focused to the cervical spine has also been shown to increase pain pressure threshold bilaterally in asymptomatic elbows. The role of the cervical spine is not only relevant in chronic pathologies; cervical spine signs have been shown to predispose individuals to the development of joint stiffness post surgery or injury. In view of these findings the cervical spine should be included in the assessment and treatment of elbow pain to elucidate local segmental stiffness that may contribute to neural sensitization.
The treatment of stiffness in the elbow is an area surrounded by much controversy and has been hindered historically by the belief that inappropriate mobilization can predispose to the development of heterotrophic ossification in the posttraumatic elbow. A review of the literature advocating that passive mobilization should not be performed reveals that most opinion is based on animal studies that employed forcible passive mobilization.9 This evidence is misleading as passive range of movement exercises and mobilization techniques employed by clinicians are not synonymous with the forcible manipulation described in these studies. Furthermore many of the papers published are either anecdotal, purely based on expert opinion or lacking in methodological rigour. In reality there are several papers which advocate the use of passive range of movement exercises. Crucially these authors have demonstrated that there is no significant difference in groups that are mobilized and those that are not in terms of heterotrophic ossification formation. Furthermore those patients with demonstrated heterotrophic ossification do not show a worsening or increase in formation if subjected to a passive mobilization regimen.9,10 Consequently, patients at risk of developing stiffness post trauma should have appropriate physiotherapy intervention. In addition, clinicians are well placed to employ preventative strategies in risk groups post trauma or surgery. It is important, however, to appreciate the different factors affecting range of movement in the joint. Page et al11 investigated electromyographic activity in elbow muscles during active elbow flexion and extension and during prolonged elbow extension in stiff and normal elbows. All muscles in the stiff elbow group had greater activity compared with controls during active elbow flexion and extension. Biceps brachii showed particularly significant increased activity during sustained extension especially when load was added. This suggests an active muscle-mediated stiffness that does not respond well to sustained loaded stretching or traditional active range of movement exercises. This clearly questions the use of commonly used rehabilitation exercises and stretching approaches and demands the application of more evidence-based approaches.
Deficits relating to the motor system, i.e. muscle function, are well reported in tennis elbow, golfer’s elbow and elbow instability, and are postulated but not proven in conditions such as snapping triceps syndrome and elbow neuropathies.12–15 Diminished strength, morphological changes and alterations in muscle timing are well described in chronic elbow conditions. Similarly, authors report a common sequela of trauma and surgery resulting in inhibition of those muscles providing local stability to the joint and increased activity in the global mobilizers of the joint. These ‘muscle imbalances’ are well described as a feature of elbow pathology and have been proposed as aetiological factors in the onset of musculoskeletal disorders.16 Proprioceptive deficits resulting from pain and swelling further impact the muscle sequencing patterns around the elbow joint. Rehabilitation has been demonstrated to successfully address these deficits, however, it is essential to recognize the specific dysfunction associated with different pathologies.
The consequence of motor system dysfunction must also be considered in terms of the kinetic chain. The kinetic chain depicts the body as a linked system of interdependent segments, working in a proximal to distal sequence imparting a desired action at the distal segment. Researchers have demonstrated that there is a coordinated pattern of muscle activation and force development from the legs to the arms as unilateral rapid arm movements are initiated.17 This illustrates the contribution of the whole body during upper limb activity. The elbow’s position at the distal end of the kinetic chain results in the transmission of high repetitive loads in upper limb sporting activity. The measured forces reported in specific sporting activities are higher than the load to failure forces of the elbow’s ligamentous structures. Local factors such as muscle action have been suggested to stabilize the joint against these forces, however, the cross-sectional area of the muscles and their direction of action are not sufficient to withstand the magnitude of these forces. Consequently, other factors must contribute to load regulation and protection of the intrinsic elbow structures. These factors relate to the sequential activation and integration of body segments.
It has been proposed that deficits in the kinetic chain resulting in insufficient proximal activation can increase the distal loads at the elbow and as a result, create acute or chronic stresses that may cause injury or decreased performance. Kibler and Sciascia evaluated the effect of altered proximal kinetic chain function on load at the elbow.17 They studied Olympic tennis players who developed the same ball speed and found that the group that exhibited knee flexion less than 10° in the cocking phase of the tennis serve increased the valgus load at the elbow by 21%. The resulting absolute load was in the range documented to be above the safe level of repetitive load. These authors evaluated 199 patients with medial elbow pain.17 In patients with signs consistent with medial collateral ligament injury nearly 50% had deficits in front leg hip/leg function. In the group requiring surgery, over 70% demonstrated these deficits. In addition 95% of patients had a glenohumeral rotation deficit and 92% had clear evidence of scapula dyskinesis. These proximal deficits are not only reported in the sporting population; electromyographic (EMG) studies have demonstrated a global weakness in the upper limbs of patients with tennis elbow affecting not only the wrist flexors and extensors, but also the shoulder abductors and external rotators.18 In addition, internal and external rotation deficits at the glenohumeral joint have been described in patients with lateral elbow pain. Importantly, it has been demonstrated that correction of these deficits correlates with relief of symptoms.17 Rehabilitation strategies must, therefore, consider the elbow in the context of the kinetic chain.
Presentation, investigation and treatment options
Pain
Pain relief is often the primary goal of rehabilitation and the commonest reason that patients seek treatment. In view of what is understood regarding peripheral and central pain mechanisms it is important that clinicians consider the different pain generators to target rehabilitation appropriately. Relevant assessment tools enable appropriate treatment selection. Pain-free grip measured with a dynamometer has been shown to be a valid and sensitive marker in measuring outcome in patients with lateral elbow pain and correlates well with the patient’s perceived outcome.19 It is a measure of the local structures both in terms of symptom production and compromise of motor function. Pain pressure threshold has been used to examine the relative importance of peripheral and central pain mechanisms in myofascial pain conditions and has been shown to be a reliable tool. Pressure algometry is used to compare the affected and unaffected sides and helps to identify reductions in pain pressure threshold indicative of central sensitization.
Ascertaining predominance of pain-free grip strength (PFGS) or pain pressure threshold (PPT) deficits aids appropriate technique selection. Vincenzino et al8 suggests that patients with greater deficits in pain-free grip compared with pain pressure threshold are likely to have more peripherally driven pain and therefore manual therapy techniques should be addressed directly to the elbow. Conversely, they suggest that patients with greater pressure pain threshold deficits, relative to pain-free grip force deficits, should be treated with techniques directed at the cervical spine. While this proposed classification system is based on current evidence it requires validation. It does, however, emphasize the importance of using appropriate assessment tools to guide rehabilitation. In view of what we understand regarding the link between central sensitization and the development of increasing pain and/or stiffness post injury or trauma, pain pressure threshold is arguably an essential tool in assessing all elbow pathologies, both traumatic and non-traumatic, to direct treatment and preventative strategies accordingly.
Rehabilitation of pain: role of manual therapy
Mobilizations with movement (MWM) are a group of techniques with a common theme – the application of a joint glide (mobilization) that is sustained while the patient performs a physical task or specific movement. In the case of tennis elbow the physical task is commonly pain-free grip. These techniques are performed without pain and in the case of lateral elbow pain a significant improvement in grip force is expected (>25%).20 Essentially these techniques can be applied to any patient with chronic elbow pain where an active movement or task produces pain. These techniques are reported to achieve improvements in pain and function immediately after their application and achieve rapid improvement in persistent musculoskeletal pain states that have been recalcitrant to other forms of therapy. Much of the initial theory regarding the mechanism of action of this treatment approach focused on mechanical effects such as the restoration of bony positional faults. More recent research, however, shows that MWM techniques are capable of producing concurrent hypoalgesic effects during and following their application, as well as altering sympathetic nervous system function.21
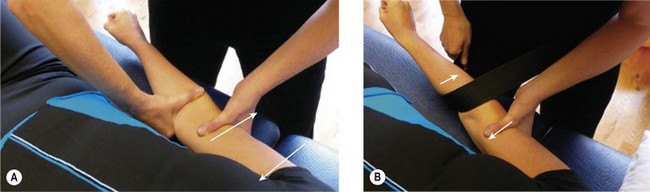
To perform a MWM technique the clinician identifies a pain provoking activity, e.g. in tennis elbow this commonly involves the patient clenching their fist. This is then repeated while the clinician performs a laterally directed glide to the elbow (Fig. 34.1A). The direction in which the lateral glide is applied and the force with which it is applied are important in maximising the hypoalgesic effect. The therapist should apply the lateral glide at a force approximately two-thirds of the maximal force to optimize the treatment effect. The technique is performed with the patient in a supine position with the affected limb fully supported on a treatment table in relaxed elbow extension and forearm pronation. When treating the right elbow the clinician stands by the patient’s right side, and facing the patient’s head, stabilizes the distal humerus laterally with their left heel of hand and first web space. The clinician then applies a laterally directed glide from the medial side to the ulna through the first web space of their right hand. The therapist sustains this glide while asking the patient to perform a pain-free grip or perform the previously provocative task/movement. The change in force of grip is noted with the glide in situ. The technique is only repeated if there is a substantial change in pain-free grip or symptoms (>25%) during application of the technique.22 If it is successful then it can be repeated up to 10 times during a single treatment session. Minor adjustments can be made to optimize the effect of the technique by altering the direction of the glide and force applied. A mobilization belt can be used to optimize the pressure applied and allow the clinician to sustain the lateral glide with less physical effort (Fig. 34.1B). Generally the glide is applied in a direction that unloads the symptomatic location, e.g. in golfer’s elbow the glide would be applied in the opposite direction, i.e. medially.
Studies reporting the efficacy of this therapy stress the importance of the technique being performed as part of a home exercise programme between treatments.23 An effective way for patients to perform the self-glide at home is to use a doorway. Patients should stand with their upper arm against a door jamb so that the elbow joint is level with the opening. They should be instructed to push the ulna laterally using the web space between the index finger and thumb of the free hand (Fig. 34.2). After several repetitions of self-MWMs the patient should be able to exercise without pain. These techniques enable patients to self-manage symptoms and improve their functional level between rehabilitation sessions.
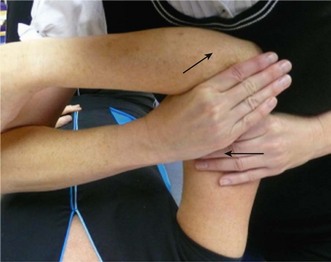
As previously discussed those patients with greater pressure pain threshold deficits, relative to pain-free grip force deficits have been shown to benefit from techniques directed at the cervical spine. Several studies report that mobilization techniques addressed to the cervical spine in patients with lateral elbow pain produce a significant hypoalgesic effect and a concomitant sympathoexcitatory response at the elbow when compared with placebo or control groups.24 A retrospective review by Cleland et al25 has suggested that patients with elbow pain receiving cervicothoracic mobilization in addition to local treatment require significantly fewer visits to achieve similar success rates in terms of pain relief and PFGS. In terms of specific manual therapy techniques the cervical lateral glide technique has been shown to achieve significant improvements in pressure pain threshold and an increase in PFGS, and also to produce a sympathoexcitatory response across sudomotor, cutaneous and vasomotor functions.26 In terms of preventative intervention in patients post trauma and post injury, the physiological results of this technique clearly show a pain-modulating effect and provide a treatment option when local treatment may be limited by necessary immobilization of the elbow. Arguably it can play a role in preventing the development of stiffness by modulating neural sensitivity. The technique is performed with the patient in a supine position and with the involved upper limb in a degree of abduction and internal rotation with the hand supported on the thorax. The clinician then applies lateral cervical glides at C5–C6 from the contralateral side towards the symptomatic side using their web space (Fig. 34.3) oscillating at a slow steady rate of approximately one per second. The technique can be repeated for up to a minute and several sets can be performed. Repetition is determined by improvements in pain pressure threshold.
Rehabilitation of pain: role of taping
Taping is a useful adjunct to treatment particularly in the initial stages of rehabilitation to reduce pain during function. Vincenzino et al27 have demonstrated an initial ameliorative effect of a specific diamond taping technique for lateral epicondylalgia, with significant improvements in PFGS of 24% and an improvement in PPT of 19%. Consequently it may have a specific application as an adjunct to the manual therapy techniques already described. Specific taping can be used to facilitate the pain-free implementation of an exercise programme for chronic elbow pain. Similarly these principles of treatment can be applied to medial elbow pain. While there is only limited evidence available regarding the diamond elbow taping, it is clear that it achieves a more significant improvement in PFGS and PPT than ‘off the shelf’ braces. The tape is applied to the lateral aspect of the elbow with the patient in a supine position and the elbow slightly flexed. Four strips of non-elastic adhesive backed sports tape are applied to the skin. They are laid onto the skin distally to proximally in a diamond shape. It is essential to simultaneously apply a tractional force on the soft tissues towards the lateral epicondyle and perpendicular to the line of the tape (Fig. 34.4A). The strips must overlap at their ends and are secured with four additional strips. This will result in an area of bulging tissue resembling ‘orange peel’ in the centre of the diamond (Fig. 34.4B). Retesting of PFGS immediately post application of the tape should reveal an improvement to reinforce its purpose.
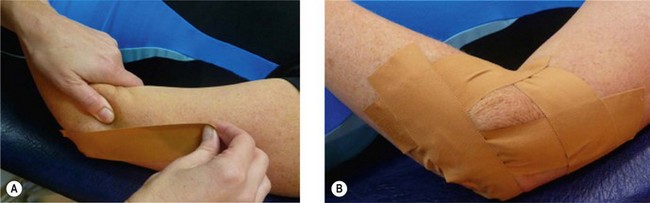
Figure 34.4 (A) Diamond taping: the tape is applied to the lateral aspect of the elbow. As each strip is applied the clinician should simultaneously apply a tractional force on the soft tissues towards the lateral epicondyle and perpendicular to the line of the tape. (B) Four strips of non-elastic tape are applied to the skin and are laid onto the skin distally to proximally in a diamond shape. If the tractional force illustrated in Figure 34.4A is applied correctly this will result in an area of bulging tissue resembling ‘orange peel’ in the centre of the diamond.
Currently there is a lack of evidence as to the mechanism of action by which the diamond taping achieves its effect on PFGS. Two explanations are currently theorized.27 The first relates to a direct mechanical effect on the muscles of the forearm resulting in a change in loading pattern. This is similar to the theory proposed but not proven for the effectiveness of orthotic braces. The second theory relates to its neurophysiological effects on the nervous system, particularly the nociceptive system. However, it is unclear whether this results from inhibition of nociceptive action and facilitation of large afferent fibre input into the spinal cord or by stimulating endogenous processes of pain inhibition.
Stiffness
Rehabilitation of stiffness: exercise
Current evidence regarding the activation patterns of the musculature in stiff elbows challenge the use of commonly utilized techniques such as sustained stretching. The biceps is highly responsive post injury to the elbow, often resulting in muscle spasm and sustained contraction of the elbow flexor musculature.11 Consequently the loss of motion in some patients has an active muscle co-contraction component in addition to passive restrictions such as the capsule. This helps to elucidate why elbow flexion contracture is the most common reported restriction post trauma. Page et al11 demonstrated that sustained extension stretching and loaded stretching (both techniques employed for increasing extension range) result in increased activity in the elbow flexors. This suggests that these techniques are, in fact, counterproductive. It would appear that the triceps is relatively inhibited in the presence of elbow flexor dominance and difficult to isolate; exercise prescription must reflect this.
Rehabilitation of stiffness: manual therapy
Manual therapy techniques can be employed to improve range of movement and expert opinion currently proposes mobilization with movement as an effective treatment choice.28 This technique can be employed to optimize the effects of the extension exercises described. The patient lies in a supine position with the shoulder flexed at 90°. A mobilization belt is wrapped around the therapist’s hips and the patients forearm so the proximal edge is level with the elbow joint. The therapist stabilizes the lower end of the humerus with one hand and supports the forearm with the other. The therapist can then glide the ulna laterally with the belt by moving their hips away. This technique must be pain-free. The patient is then asked to actively extend their elbow while the therapist maintains the lateral glide. As the patient extends it is important to remember that due to the carrying angle (as the patient extends) the treatment plane will alter slightly, and so the direction of glide must be adapted accordingly. This technique can be done without a belt if the therapist fixes the lower end of the humerus with one hand and applies the glide with the other hand (Fig. 34.5). The glide is applied with the lateral border of the second metacarpophalangeal joint over the upper end of the ulna at the joint margin. It is important that the therapist assesses the primary direction of glide restriction as in some patients the medial glide may be more restricted. The same technique can be applied by simply changing the direction of the glide and fixing the humerus on the opposite side.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree