Chapter 23 Rehabilitation of Posterior Cruciate Ligament and Posterolateral Reconstructive Procedures
Clinical Concepts
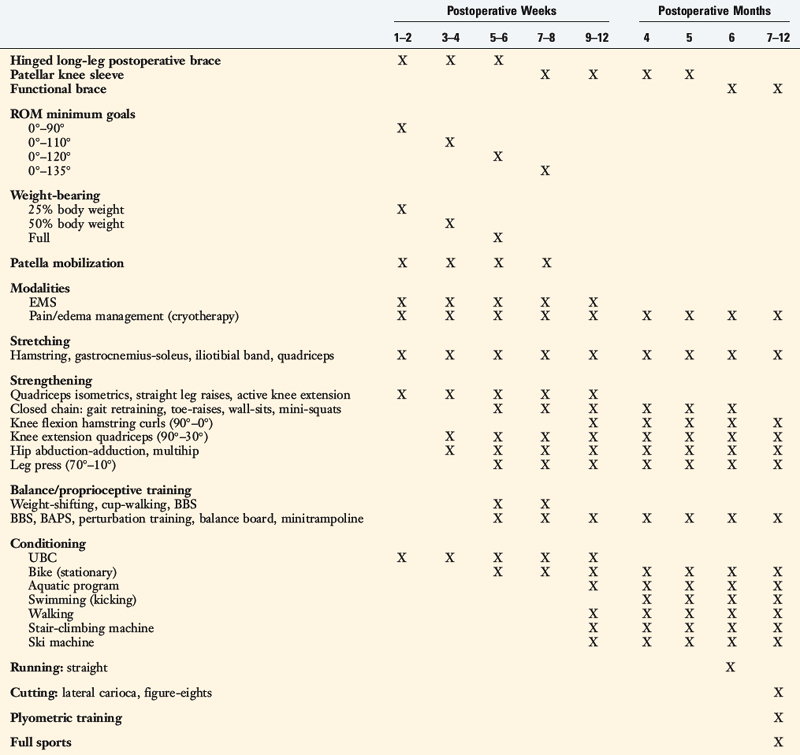
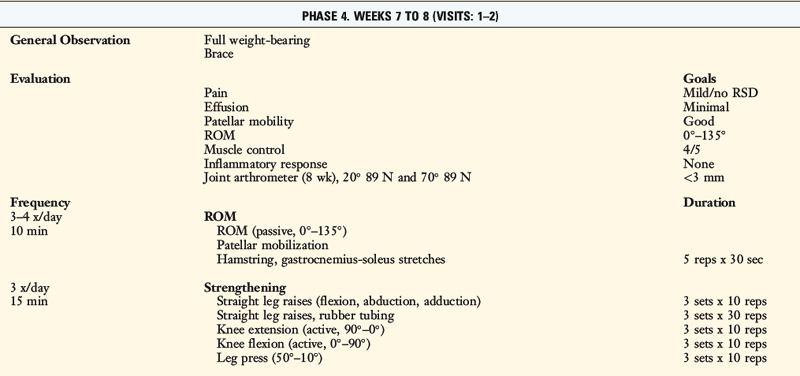
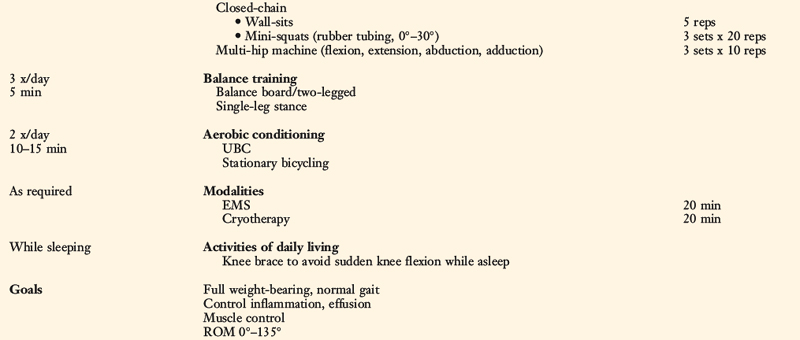
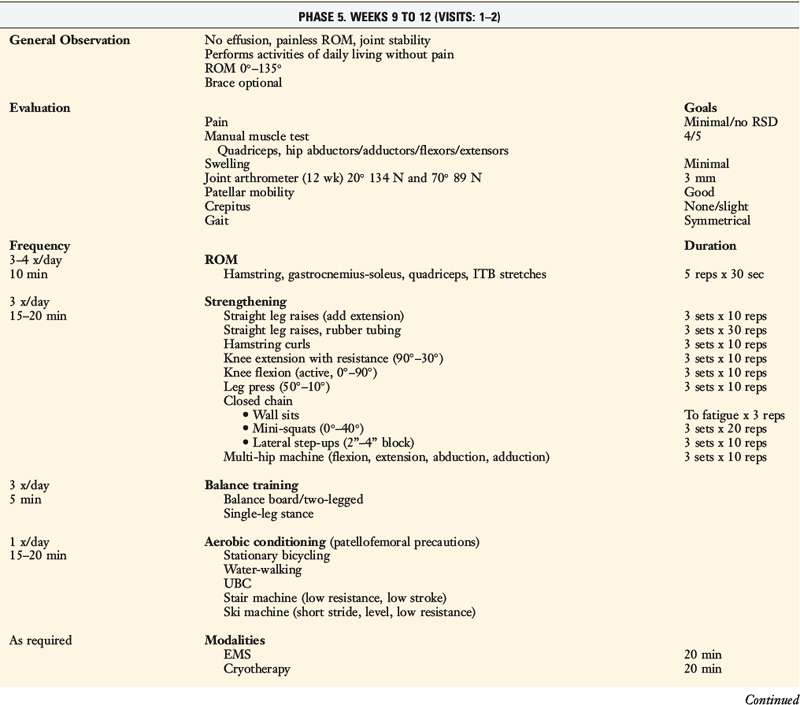
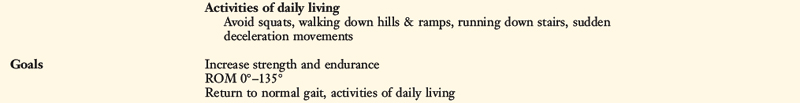
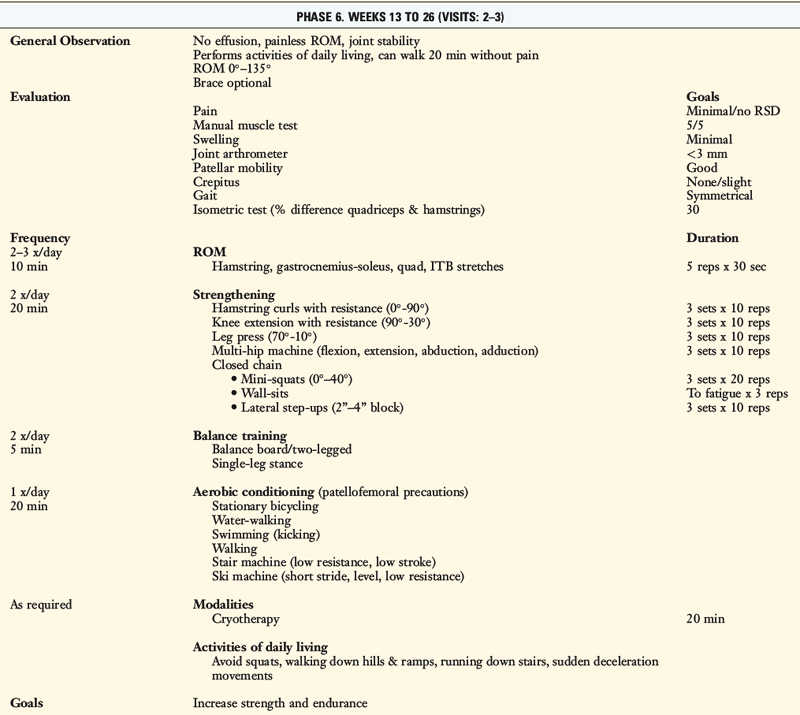
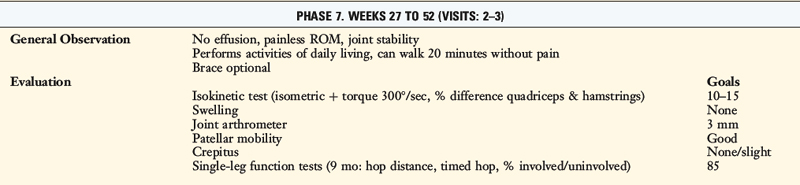
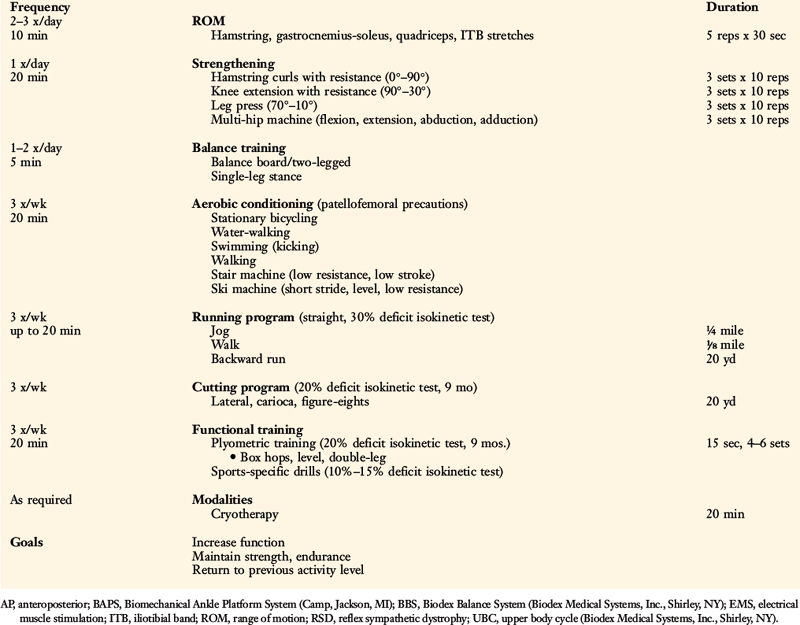
The rehabilitation protocols described in this chapter consist of a careful incorporation of exercise concepts supported by scientific data and clinical experience.3,14,15,17 The goal is to progress a patient on a rate that takes into account athletic and occupational goals, condition of the articular surfaces and menisci, return of muscle function and lower limb control, postoperative graft healing, and graft remodeling. Modifications to the postoperative exercise program may be required if noteworthy articular cartilage deterioration is found during surgery.
The protocol for PCL reconstruction was developed for a high-strength two-strand graft (quadriceps tendon–bone, bone–patellar tendon–bone). The protocol for posterolateral reconstruction may be used after the various operative options described in detail in Chapter 22, including anatomic and proximal advancement techniques of the posterolateral structures and nonanatomic femoral-fibular reconstruction.
Critical Points CLINICAL CONCEPTS
Patients with posterolateral reconstruction are warned specifically at the 4th to 8th postoperative weeks that, with resumption of weight-bearing and weaning of crutches, to avoid a varus or internal tibial rotation position that could place high tensile forces on the posterolateral structures.13,16 It is important that the patient demonstrates good lower extremity control with suitable muscle strength to maintain tibiofemoral compensation and avoid a lift-off of the lateral tibiofemoral joint, which may disrupt the posterolateral reconstruction.
PCL Clinical Biomechanics
Kaufman and coworkers8 used a three-dimensional biomechanical model to predict dynamic patellofemoral and tibiofemoral forces generated during isokinetic exercises at 60°/sec and 180°/sec. During isokinetic extension, posterior shear forces were detected at knee flexion angles of 40° and greater. The maximum posterior shear force occurred at 70° to 80° of knee flexion and measured 0.5 ± 0.1 body weight at 60°/sec and 0.6 ± 0.1 body weight at 180°/sec
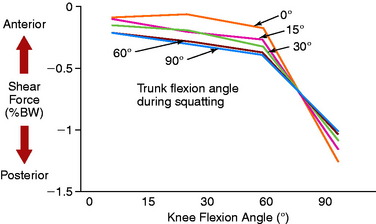
Ohkoshi and associates19 used a two-dimensional model to calculate shear force exerted on the tibia during standing at various knee flexion angles in 21 healthy subjects. Posterior shear forces were found in the upright position of the trunk and at knee flexion angles of 15° to 90° (Fig. 23-1). At 30° and 60°, the posterior drawer force was significantly increased by anterior flexion of the trunk.
Castle and colleagues4 measured posterior tibial subluxation during a static double-legged squat in patients with PCL-deficient knees. The results revealed a statistically significant mean increase of 5.9 mm in posterior tibial translation (P < .05) of the injured knee compared with the contralateral knee at high knee flexion angles. At low flexion angles, the magnitude of increase in mean posterior tibial translation was only 2.1 mm. Tibiofemoral shear forces were small compared with tibiofemoral joint compression forces.
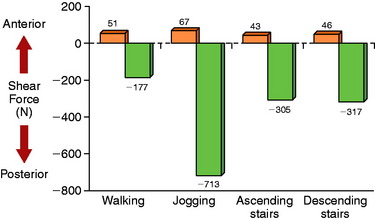
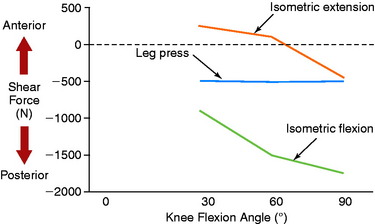
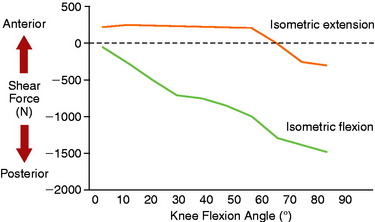
Berchuck and coworkers2 calculated large posterior shear forces during gait analysis for the activities of jogging, ascending stairs, and descending stairs (Fig. 23-2) in five normal subjects. Lutz and associates9 evaluated tibiofemoral joint shear and compressive shear forces using a two-dimensional biomechanical model and electromyographic (EMG) activity of hamstrings and quadriceps muscle activity during a closed kinetic chain (CKC) leg press exercise, an isometric open kinetic chain (OKC) exercise, and an OKC flexion exercise. Measurements of maximum muscle contractions were obtained at 30°, 60°, and 90° of knee flexion. The OKC isometric flexion exercise produced posterior shear forces at all knee flexion angles (Fig. 23-3), ranging from –939 ± 174 N at 30° of knee flexion to a maximum of –1780 ± 699 N at 90° of knee flexion. The CKC exercises produced significantly less posterior shear forces at 60° and 90° of flexion (–538 N; P < .05). These findings were similar to those reported by Smidt21 during isometric knee extension and flexion exercises (Fig. 23-4). Maximum hamstrings EMG activity was detected during the OKC exercise at 90° of flexion (82 ± 15% of maximum contraction). The antagonistic muscle activity was minimal during this exercise at all knee flexion angles. In contrast, co-contraction of the quadriceps and hamstrings was observed during the CKC exercise, which was greatest at 30° and 60° of flexion. The authors concluded that CKC exercise produced significantly less tibiofemoral shear forces compared with OKC exercise (P < .05).
Critical Points POSTERIOR CRUCIATE LIGAMENT CLINICAL BIOMECHANICS
CKC, closed kinetic chain; OKC, open kinetic chain; PCL, posterior cruciate ligament.
Wilk and colleagues23 evaluated tibiofemoral shear forces and EMG activity of the quadriceps, hamstrings, and gastrocnemius muscles during OKC extension and CKC leg press and squat exercises. Both CKC exercises produced posterior shear forces. However, during the squat, these forces were relatively low (245–565 N) from 0° to 45° of knee flexion. A rapid increase in posterior shear forces was detected from 45° to 72° of flexion. In addition, co-contraction of the quadriceps and hamstrings occurred from 0° to 30° of flexion. The authors concluded that vertical squats from 0° to 45° of flexion should not be performed in knees in the early stages of PCL reconstruction rehabilitation.
Wilk and colleagues23 also found that the knee extension exercise produced posterior shear forces from 60° to 100° of knee flexion; however, these forces were lower than those measured during both CKC exercises. The leg press induced minimal hamstring muscle activity.
Hoher and coworkers7 reported that the in situ forces in the PCL significantly increased with knee flexion in response to an isolated hamstrings load, reaching a maximum at 90° of flexion. These findings were in agreement with other authors5,24 who also reported increased strain in the PCL with knee flexion. The addition of a 200-N quadriceps load (simulating co-contraction of the quadriceps and hamstrings) reduced the in situ forces in the PCL.
Toutoungi and associates22 combined noninvasive experimental measurements with geometrical modeling of the lower extremity to calculate ligament forces during isometric, isokinetic, and squat exercises. The data indicated that isokinetic extension at knee flexion angles less than 70° should be safe in the early postoperative period after PCL reconstruction. However, isokinetic flexion and deep squats should be avoided. During isokinetic flexion, only the PCL is loaded and peak forces may reach over 4 times the patient’s body weight at 90° of knee flexion. During squatting, PCL forces may reach 3.5 times body weight at high knee flexion angles. Shallow squats with knee flexion angles kept below 50° may be considered.
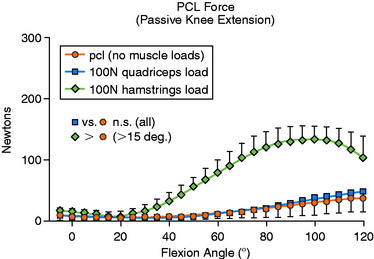
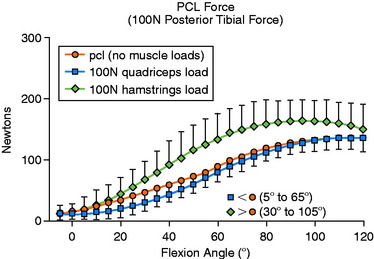
Markolf and colleagues10 studied the effects of muscle loads on cruciate force levels when the knee was subjected to external forces and moments. Load cells were installed into cadaveric knees to record forces in the ACL and PCL under five loading conditions. These force measurements were repeated with a 100-N load applied to the quadriceps tendon and with a combined 50-N load applied to both the biceps and the semimembranosus-semitendinosus tendons.
With no applied tibial force, application of hamstrings load significantly increased mean PCL force from 15° to 120° of knee flexion (Fig. 23-5; P < .05). With the application of a 100-N posterior tibial force, the addition of hamstrings load significantly increased mean PCL force between 30° and 105° of flexion (Fig. 23-6; P < .05). When a 5-Nm external tibial torque was applied, the addition of hamstrings load significantly increased mean PCL force beyond 75° of knee flexion (P < .05). Under a 5-Nm internal tibial torque, application of hamstrings load also significantly increased mean PCL force between 60° and 100° of flexion (P < .05). The authors concluded that, in general, the hamstrings were more effective in producing changes in cruciate force levels. Application of tibial torque in either an anterior or a posterior direction when the knee was flexed greater than 60° increased PCL force, and isolated hamstrings activity (with tibial torque) further increased PCL force.
Protocol for Partial or Acute Isolated PCL Ruptures
The rules to treat partial or acute isolated PCL tears are
PCL Reconstruction Postoperative Protocol
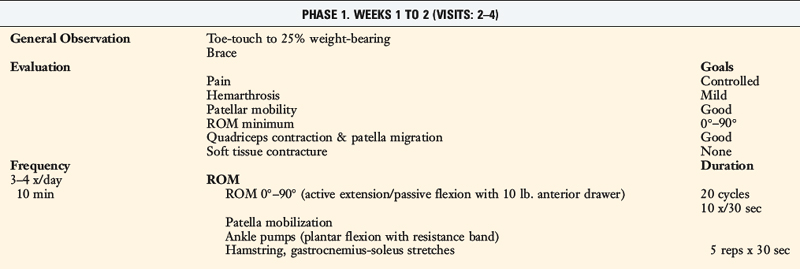
Immediate Postoperative Management
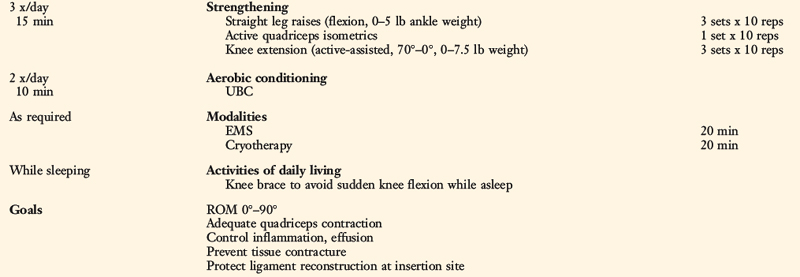
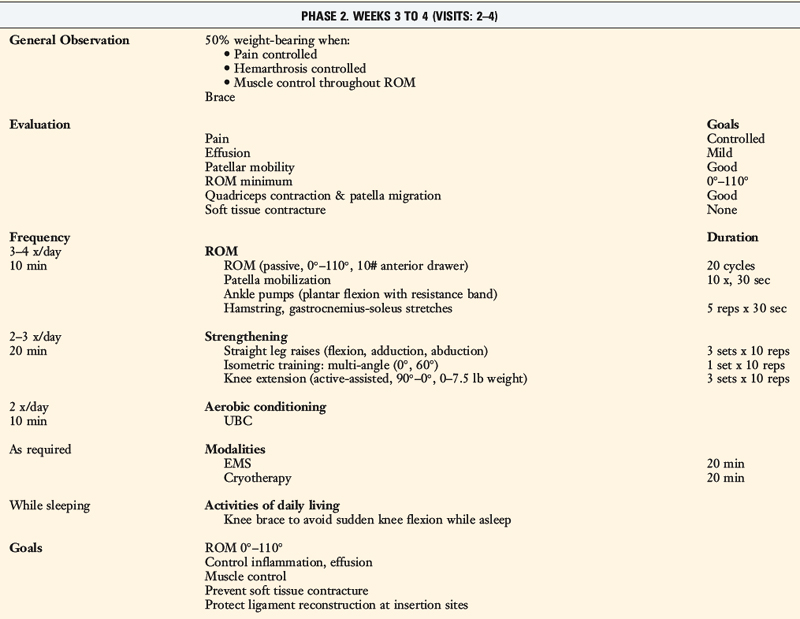
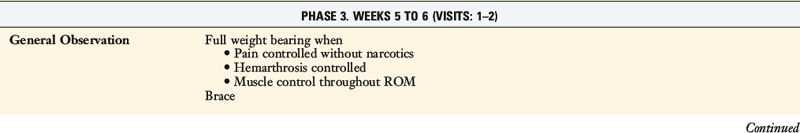
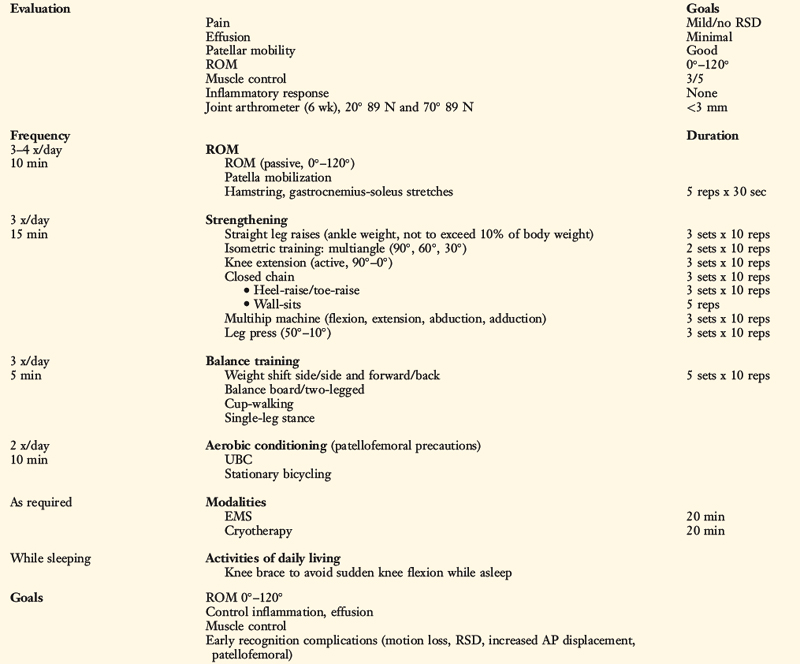
Patients present to physical therapy the 1st day after surgery on bilateral axillary crutches in a postoperative dressing with a long-leg brace locked in full extension (Table 23-1). The postoperative bandage and dressing are changed to allow the application of thigh-high compression stockings and a compression bandage. Early control of postoperative effusion is essential for pain management and early quadriceps reeducation. In addition to compression, cryotherapy is important in this time period.
Critical Points IMMEDIATE POSTOPERATIVE MANAGEMENT
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree