Chapter 27 Rehabilitation of Patients with Swallowing Disorders
Swallowing is a complex biologic function essential to human life. Dysphagia, or impaired swallowing, is a common symptom in many disorders. Dysphagia can lead to serious sequelae, such as malnutrition and pneumonia, and can dramatically alter quality of life when it prevents the individual from participating in mealtimes. Dysphagia rehabilitation focuses on the use of therapy and compensatory strategies to improve swallowing and prevent complications. Development of an individualized rehabilitation program requires an understanding of the anatomy and physiology of swallowing, the pathophysiology of swallowing dysfunction, and the nature of the underlying disease process, as well as individual and environmental factors.106 This chapter focuses on oral and pharyngeal swallowing dysfunction, because these are commonly amenable to the rehabilitation approach. We start with the physiology of normal and abnormal swallowing, then discuss the evaluation of swallowing, and finally discuss the treatment of dysphagia.
Normal Swallowing
Physiology
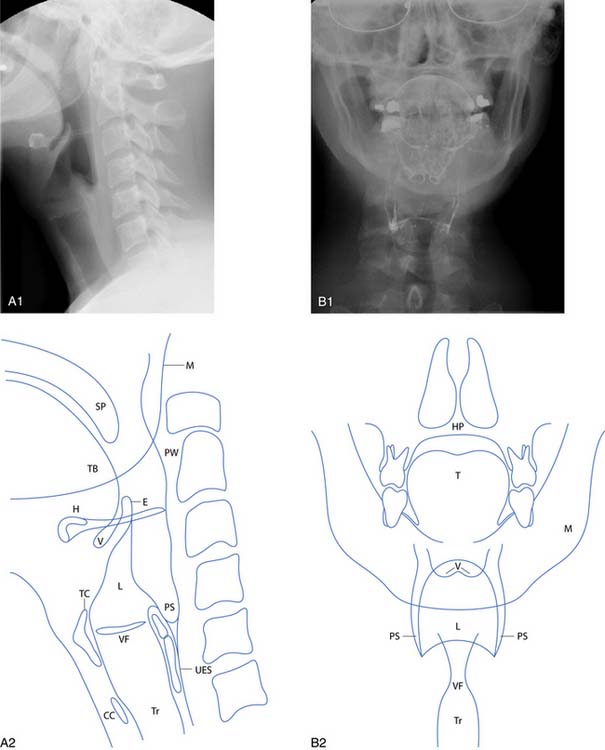
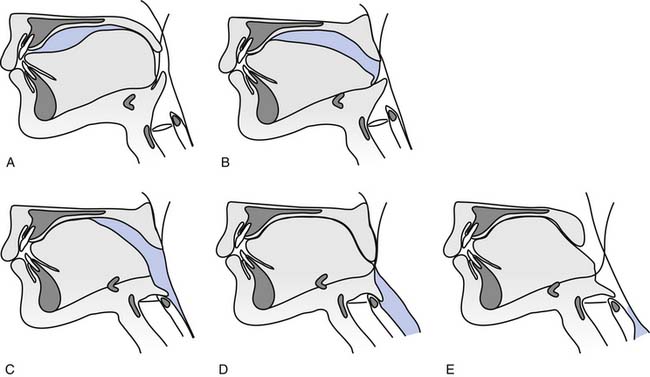
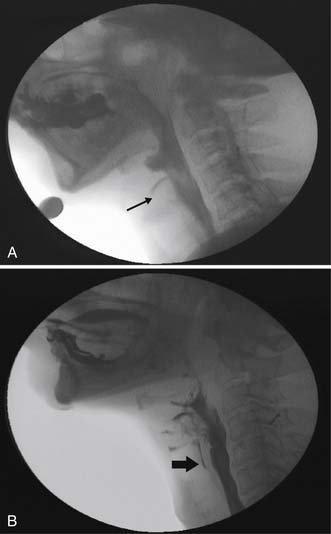
The anatomy of the oral cavity, larynx, and pharynx is shown in Figures 27-1 and 27-2. The swallowing process is traditionally divided into oral, pharyngeal, and esophageal stages (Figure 27-3). The oral stage is further subdivided into oral preparatory and oral propulsive stages.79
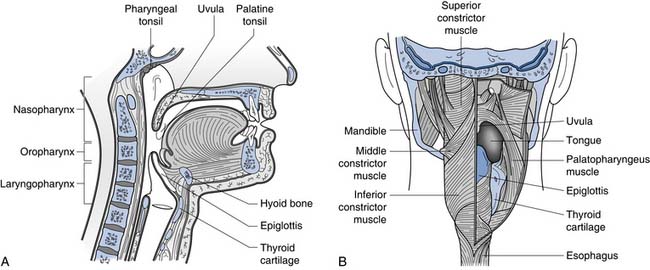
FIGURE 27-1 Anatomy of the oral cavity and pharynx. A, Divisions of the pharynx. B, Posterior view of the pharynx.
(Modified from Banks JC, Nava PB, Petersen D, et al: Atlas of clinical gross anatomy, St Louis, 2005, Mosby, with permission.)
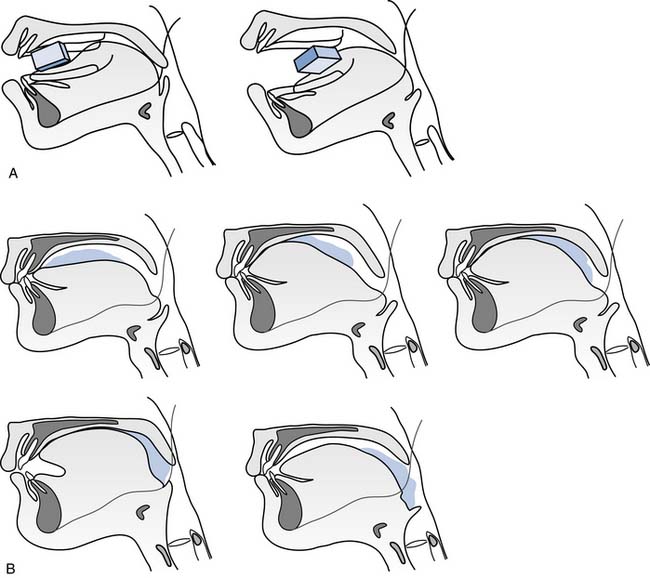
The process is somewhat different when eating solid food (Figure 27-4).28,45,110 When the bite of food enters the mouth, it is moved into position for chewing via a mechanism known as stage 1 transport (see Figure 27-4, A). During stage 1 transport, the food is first placed on the surface of the tongue. The entire tongue shifts bodily backward in the mouth, carrying the food to the molar region. The tongue then rotates (around the anteroposterior axis) and deposits the bite of food on the occlusal surface of the lower molar teeth.
After stage 1 transport is food processing, in which food particles are reduced in size by mastication and softened with saliva. This is accomplished by rhythmic, linked movements of the jaw, tongue, cheek, and soft palate.10,46,92,97,107 The jaw opens and closes cyclically. The food is compressed during jaw closing. The tongue and cheek work in conjunction during jaw opening to reposition between the teeth.10,97
When a portion of the food reaches a swallow-ready consistency, it is positioned on the surface of the tongue and squeezed back into the pharynx by a mechanism known as stage 2 transport (see Figure 27-4, B). The soft palate lifts away from the tongue surface rhythmically during food processing and stage 2 transport to allow bolus transport through the faucial isthmus. The basic mechanism of food propulsion is nearly identical to that described for the oral propulsive phase with a liquid bolus: the tongue compresses the bolus against the palate, and the area of tongue-palate contact expands from anterior to posterior, squeezing the bolus into the oropharynx. Food processing can continue while food accumulates in the oropharynx during multiple stage 2 transport cycles. Bolus aggregation in the oropharynx can last as long as 10 seconds in normal individuals eating solid food.45
In the pharyngeal stage of swallowing, the bolus is propelled from the pharynx into the esophagus (see Figure 27-3). The pharyngeal stage depends on sequential activation of muscles in the oral cavity, tongue, pharynx, and larynx.18,26,59,114 The soft palate elevates and presses against the lateral and posterior wall of the pharynx, closing off the nasopharynx. The tongue base retracts (pushes backward) to compress the bolus against the pharyngeal wall. The pharyngeal constrictor muscles contract around the bolus sequentially from top to bottom, creating a wave of contraction that squeezes the bolus downward.58 The pharynx also shortens to reduce pharyngeal volume.111 The larynx closes to prevent aspiration. The upper esophageal sphincter (UES) opens, permitting the bolus to enter the esophagus.
The hyoid bone and larynx are pulled upward and forward by contraction of the suprahyoid and hypothyroid muscles. These motions are important for protecting the airway and opening the UES. Upward movement of the hyoid is highly variable and is influenced by the initial food consistency, whereas the forward movement is less variable and is related to the opening of the UES.17,54
Several protective mechanisms prevent aspiration during swallowing. Breathing pauses briefly during swallowing.125 The duration of this swallow apnea typically ranges from 0.3 to 1.0 seconds and increases with bolus volume.48,118 The hyoid bone and larynx are pulled upward and forward by contraction of the suprahyoid and thyrohyoid muscles. This tucks the larynx under the base of the tongue. The vocal folds close to seal the glottis.101 The arytenoids tilt forward to contact the base of the epiglottis,80 and the epiglottis folds backward. This deflects food away from the laryngeal airway.
The UES is held closed between swallows by tonic contraction of the cricopharyngeus muscle, but it opens briefly during each swallow.31 Three main factors contribute to UES opening17:
The esophagus is quite different from the pharynx because it is primarily composed of striated muscle in its cervical portion and smooth muscle in its thoracic portion. Because the thoracic esophagus is largely smooth muscle, it has intrinsic contractile activity that can be increased or inhibited by autonomic nerves. Once the bolus has passed through the UES, it is propelled down the esophagus by peristalsis (defined as a wave of inhibition followed by a wave of excitation that propels material down a hollow viscus).44 In the upright position, gravity assists peristalsis. The lower esophageal sphincter is held closed by tonic muscle contraction between swallows. It relaxes during a swallow and is pushed open by the pressure of the descending bolus.
Neuroanatomy
Mastication, swallowing, and respiration are controlled by central pattern generators.9,55,86,144 The neural organization of swallowing requires integration of sensory input, cortical modification, reflexes, and all three of these central pattern generators. The central pattern generator for pharyngeal swallowing is located in the brainstem reticular formation.55 Sensory information gathered from mechanoreceptors, chemoreceptors, and thermoreceptors in the oral cavity, pharynx, and larynx facilitate swallowing and protect the airway.95,126 Sensation is carried through the maxillary and mandibular branch of the trigeminal nerve, the glossopharyngeal nerve, and the vagus nerve to a central pattern generator for swallowing. This central pattern generator is located in the nucleus tractus solitarius of the medulla.55
When a swallow is initiated, motor neurons in the brainstem produce coordinated contraction of striated muscle fibers in the oropharynx. Swallowing consists of sequential excitation and inhibition of more than 50 muscles. Table 27-1 shows the innervation of major muscles related to swallowing. These lower motor neurons have their cell bodies in the trigeminal (V), facial (VII), and hypoglossal (XII) nuclei, and in the nucleus ambiguus (IX and X).
Table 27-1 Innervation of Major Muscles Related to Swallowing
| Cranial Nerve | Muscles |
|---|---|
| Trigeminal nerve (V) | |
| Facial nerve (VII) | |
| Glossopharyngeal nerve (IX) | Stylopharyngeus |
| Vagus nerve (X) | |
| Hypoglossal nerve (XII) |
Human Development and Aging
Swallowing in Infants
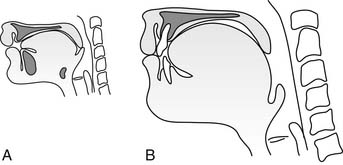
The upper aerodigestive tract of the newborn exhibits anatomic differences from the adult, and these differences support early feeding skills (Figure 27-5). These differences include a smaller, retracted lower jaw; a smaller oral cavity almost completely filled by the tongue; and buccal “sucking pads” to create stability for early sucking patterns. The larynx rests higher in the neck, and the epiglottis approximates and even slightly overlaps the soft palate. This separates the airway and food way between swallows, allowing the nasopharynx to communicate with the trachea while food can collect in the valleculae, thereby decreasing the risk for aspiration.65,99 The hyoid bone and larynx descend in the neck during infancy and childhood, and the contact between the epiglottis and the soft palate is lost.76
Swallowing in the Elderly
Oral, pharyngeal, and esophageal changes occur in the elderly, related to motor performance and respiratory control during swallowing. Labial and lingual strength and coordination decrease, resulting in slower oral manipulation of food. Dentition is often reduced, resulting in increased mastication time and reduced efficiency.43 Multiple gestures of the tongue base and hyoid can occur before pharyngeal swallow initiation, along with increased duration of hyoid motion during swallows. An increased latency might be observed from entry of the bolus into the pharynx until onset of laryngeal elevation. Reduction in esophageal function occurs, with a decreased amplitude of esophageal peristaltic waves and an increased incidence of sliding hiatal hernia. Altered respiratory patterns in the elderly are characterized by an earlier onset and a longer duration of swallow apnea, an increased incidence of swallow initiation in the inspiratory phase of respiration, and an increased respiratory rate immediately after the swallow.47,48,125 An increased frequency of laryngeal penetration is seen in older adults on consecutive swallows, and might be a normal variation.19
Pathophysiology of Swallowing Dysfunction
Dysphagia can be caused by a wide variety of diseases and disorders affecting the structure and/or function of the oral cavity, larynx, pharynx, or esophagus. Structural deficits can masquerade as functional disorders, so careful diagnostic evaluation is necessary in every case. Dysphagia is commonly classified according to the anatomic region affected—that is, oral, pharyngeal, or esophageal dysphagia. Dysfunction of the oral cavity commonly co-occurs with pharyngeal dysfunction. This is commonly termed oropharyngeal dysphagia (although the problem is not limited to the oropharynx). Regardless of site, it is useful to consider whether a given impairment of swallowing affects food transport (preparation and propulsion of the bolus), airway protection (prevention of laryngeal aspiration), or both, because these have implications for treatment. Aspiration of food can occur in structural or functional impairments of the oral cavity, pharynx, or esophagus. It is important to recognize dysphagia because it can cause dehydration, malnutrition, or respiratory sequelae.
Dysfunction of the pharynx can produce impaired swallow initiation, ineffective bolus propulsion, and retention of a portion of the bolus in the pharynx after swallowing. Velopharyngeal incompetence is the inability to close the velopharyngeal isthmus by elevating the soft palate and contracting the pharyngeal walls around it to close off the nasopharynx. In velopharyngeal incompetence, the bolus might be misdirected into the nasal cavity (nasal regurgitation). When tongue base retraction is weak, pharyngeal propulsive force can be inadequate, resulting in retention of all or part of the bolus in the pharyngeal recesses after swallowing. Similar findings can be produced by weakness of the pharyngeal constrictor musculature. If the epiglottis does not invert during swallowing, it might act as a physical barrier, resulting in retention of part of the bolus in the valleculae after swallowing.
Airway protection is a critical function of swallowing. But airway protection mechanisms are not always effective. The failure of laryngeal protective mechanisms can reflect reduced laryngeal elevation, incomplete closure of the laryngeal vestibule, or inadequate vocal fold closure caused by weakness, paralysis, or anatomic fixation. For the purpose of dysphagia rehabilitation, laryngeal penetration is defined as passage of material into the larynx but not through the vocal folds. Aspiration is defined as passage of material through the vocal folds (Figure 27-6). Laryngeal penetration can be observed in normal individuals. Aspiration of microscopic quantities occurs in normal individuals, but aspiration that is visible on fluoroscopy or endoscopy is pathologic, and is associated with an increased risk for aspiration pneumonia or airway obstruction.87 The normal response to aspiration is a strong reflex coughing or throat clearing. Laryngeal sensation is often abnormal, however, in individuals with severe dysphagia.36 Silent aspiration, or aspiration in the absence of visible response, has been reported in 25% to 30% of patients referred for dysphagia evaluations.36,72,129 The effects of aspiration are highly variable, and some individuals tolerate small amounts of aspiration without apparent ill effects.37 Several factors determine the effect of aspiration in a given individual, including the quantity of the aspirate, the depth of the aspiration material in the airway, the physical properties of the aspirate (acidic material is most damaging to the lung), and the individual’s pulmonary clearance mechanism.105 Predictors of aspiration pneumonia risk include diagnoses of chronic obstructive pulmonary disease and congestive heart failure, presence of a feeding tube, oral-dental status, bedbound status, and presence of dysphagia.50,67,88
Dysphagia can result from a wide variety of disorders64; see Box 27-1 for a partial list.11 A major cause of dysphagia is stroke. Dysphagia is found in about half of individuals with a recent stroke.39,103,116 Most recover within the first 2 weeks, but dysphagia can be severe and persistent. Brainstem lesions can result in particularly severe dysphagia, given their proximity to the major swallow centers.27,55,140 Reduced laryngeal elevation, insufficient UES opening, vocal fold weakness, and severe weakness of oropharyngeal muscles are common in patients with stroke. Cerebral lesions can result in dyscoordination of the swallow, with impaired oropharyngeal bolus propulsion and airway protection. Swallowing dysfunction is typically more severe in bilateral cerebral lesions, because there is bilateral cortical representation for swallow function. On the other hand, the brainstem motor nuclei innervate only ipsilateral muscles, so lesions of cranial nerves or their nuclei can result in unilateral sensory or lower motor neuron dysfunction.3
BOX 27-1 Selected Causes of Oral and Pharyngeal Dysphagia
In neurodegenerative disorders, dysphagia can be the first symptom.5 Oral-stage dysphagia is common in Parkinson disease, characterized by lingual tremor and tongue-pumping behaviors, which hamper oral food transport.74 Alzheimer disease can result in agnosia for food within the oral cavity, characterized by oral holding and incoordination of swallowing. In motor neuron disease, progressive degeneration of motor neurons in the brain and spinal cord results in weakness in the muscles of mastication, respiration, and swallowing. Inflammatory muscle diseases, including dermatomyositis and polymyositis, commonly affect striated muscles, resulting in weakness of the pharynx. Progressive systemic sclerosis, on the other hand, affects smooth muscle. It commonly produces esophageal dysfunction, including reduced peristalsis, dilatation of the lower esophagus, and gastroesophageal reflux disease (GERD).
Radiation therapy can cause fibrosis of the oral cavity, pharynx, and larynx immediately after radiation or, in some cases, years later. Xerostomia and edema are common when salivary glands are within the radiation field, hampering bolus formation and timing of oral and pharyngeal transport. The salivary changes are often permanent. Fibrosis can result in delayed swallow initiation, decreased pharyngeal transport, and ineffective laryngeal protection.62
Structural abnormalities can impair pharyngeal transport and airway protection. Cervical osteophytes are common in the elderly and can impinge on the pharynx (Figure 27-7).25 This can also be seen with edema or hematoma after anterior cervical fusion. Webs and strictures can obstruct the food pathway. Diverticulae can form along the pharyngeal or esophageal walls. The Zenker diverticulum is a pulsion diverticulum of the hypopharynx. Its mouth is located just above the cricopharyngeus muscle, but the body of the pouch can extend much lower. Food or liquid collects in the diverticulum and can be regurgitated to the mouth or result in aspiration.
Esophageal dysfunction is common and is often asymptomatic. Webs, rings, or strictures of the esophagus can obstruct the lumen and might require dilatation. Esophageal motor disorders include conditions of either hyperactivity (e.g., esophageal spasm) or hypoactivity (e.g., weakness) of the esophageal musculature. Either of these can lead to ineffective peristalsis with retention of material in the esophagus after swallowing. Retention can result in regurgitation of material from the esophagus back into the pharynx, with aspiration of the regurgitated material.
Dysphagia is often iatrogenic. Several medications can cause dysphagia through sedation, pharyngeal or esophageal muscle weakness, movement disorders, sensory loss, or impaired salivation (Table 27-2).128,135 Postsurgical dysphagia is a common complication of anterior cervical fusion, occurring in about half of the patients.131 The mechanism is unclear but might be related to injury of the pharyngeal constrictor muscles or their innervation. Most patients recover within the first 2 months. Dysphagia can also be a complication of carotid endarterectomy or surgery for cancer of the esophagus or the head and neck.6
Table 27-2 Drug-Induced Dysphagia
| Medication | Effect on Oropharyngeal Swallowing |
|---|---|
| Central nervous system depressants | Depressed brainstem function and control of swallowing |
| Neuromuscular blockade | Weakness of oropharyngeal musculature and cough |
| Dopamine antagonists | Extrapyramidal reactions (dystonia, dyskinesia) |
| Anticholinergic medications | Salivary changes, impaired esophageal peristalsis |
| Anesthesia | Suppressed laryngeal cough reflex |
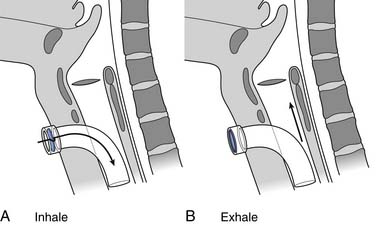
Compromised and altered respiratory function increases the risk for dysphagia. Chronic obstructive pulmonary disease alters the coordination of respiration and deglutition.98,125 Exacerbations can lead to aspiration. Endotracheal intubation and ventilator dependency can cause decreased laryngeal sensation, pooling of secretions in the pharynx and larynx, impaired swallow initiation, and aspiration.142 The presence of a tracheostomy tube alters normal pharyngeal aerodynamics, eliminating the positive subglottic pressure normally associated with swallowing and hampering laryngeal protective reflexes. An inflated cuff does not fully eliminate aspiration,40,63 because secretions can still leak around the cuff into the trachea. A cuffless tracheostomy tube is often better tolerated. A unidirectional tracheostomy speaking valve prevents expiratory airflow through the tracheostomy tube, providing expiratory flow through the larynx and upper airway, and restoring positive subglottic air pressure (Figure 27-8). Use of a unidirectional valve can improve swallow safety by reducing laryngeal penetration and aspiration.40
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree