Fig. 34.1
(a, b) Vestibular retraining (VOR, horizontal canal)
Fig. 34.2
Oculomotor retraining. (a) Convergence; (b) unilateral ocular focus retraining
Concussion management can be daunting for both the medical professional and the extreme sports athlete. This area continues to be a focal point for research. As more evidence and information is produced regarding management, clinicians as well as the athlete will feel more comfortable and confident working through the evaluation and rehabilitation process. There is evidence pointing us in the direction of a strong clinical examination to aid our diagnosis, a thorough step wise return to activity and sport, and cervicovestibular rehabilitation if symptoms are protracted [24]. We can use this information to better assess, and assist the extreme sport athlete to full recovery after a concussion.
34.3 Shoulder Dislocation
Shoulder dislocation is common in several extreme sports, including windsurfing, surfing, snowboarding, skiing and kayaking [25–30]. As with most shoulder dislocations, the anterior variety appears to be the most common [31]. Traumatic anterior shoulder dislocation (ASD) commonly occurs with the arm in abduction and external rotation and leads to predictable anatomic injuries (Table 34.1). Generally, a combination of shoulder abduction with external rotation and extension can lever the humeral head out of the glenoid fossa and dislocate the shoulder. Extension of the elbow also increases the force transmitted along the arm, increasing the risk of wrenching the humeral head out of the glenoid fossa [32–34].
Injury | Description |
|---|---|
Bankart lesion | Avulsion injury of the labrum ± capsular injury inferior to the equator of the glenoid |
Anterior labral periosteal sleeve avulsion (ALPSA) | Lesion of the anterior band of the inferior glenohumeral ligament, the labrum, and the anterior scapular periosteum |
HAGL lesion | Humeral avulsion of the glenohumeral ligament |
IGHL damage | Plastic deformation or tear ± complete mid-substance tears of the capsule |
Glenoid rim fracture | Shear fracture or avulsion fracture of the IGHL attachment |
Hill-Sachs fracture | Impression fracture of the posterosuperolateral humeral head |
Greater tuberosity fracture | Fracture of greater tuberosity of humerus – serves as the insertion site of the rotator cuff tendons |
Rotator cuff tear | Full- or partial-thickness tendon tear to one or more of four muscular divisions: (a) the subscapularis, (b) the supraspinatus, (c) the teres minor, and (d) the infraspinatus |
Examples in pertinent sports are the following: in kitesurfing and wakeboarding shoulder dislocations are generally the result of unsuccessful tricks and jumps, in particular handle pass maneuvers [35, 36]. ASD is the most common upper extremity injury in windsurfing, usually caused by hanging onto a boom during a fall. Among skiers and snowboarders, shoulder dislocation is usually a consequence of a fall onto an outstretched hand with an element of rotation [29, 30]. In surfing, shoulder dislocation usually occurs while paddling with a poor, wide armed technique or in rough water [38–43]. In white water paddle sports, strenuous high brace supports to avoid capsizing have been associated with traumatic ASD as poor high brace technique is considered to make the shoulder vulnerable [31, 41].
Also, in skydiving a threat to the shoulder joint stability may depend on “swimming around in thick fluid airstreams” [43].
34.3.1 Diagnosis and Management
It is always important to obtain an accurate history and examination to assess the presence of intrinsic and extrinsic factors that may have predisposed the dislocation or can influence the course of treatment. Rotator cuff, surface area of contact and capsulolabral complex may be damaged by the trauma but could also be congenitally disposed to dislocation or have damaged traumatic forces over time. It is appreciated that asymptomatic individuals greater than 60 years old had 28 % incidence of full thickness rotator cuff tears, 26 % partial thickness tears, and this increases to 80 % in the eighth decade of life [44].
Therefore, treatment options should be dependent on patient’s goals, etiology and depth of the tear. Wolf et al., states, considerable thought should be given to differentiating between articular and bursal-sided tears and nonsurgical treatment with rehabilitation is successful in most patients and may be a viable option for management [45].
In the initial phase, clinical diagnosis of a rotator cuff tear may be difficult secondary to pain, guarding, and previous shoulder pathology [46]. Imaging may be obtained to identify the severity of intrinsic variables after injury.
The diagnostic performance of MRI and ultrasonography (US) may be similar for detection of any rotator cuff tears. However, the sensitivity of US may be much lower than that of MRI for detecting partial thickness tears [56]. Although radiographs are important screening tools, the definitive imaging assessment is obtained with cross-sectional imaging. CT is the first-line imaging modality for the evaluation of glenoid bone loss and Hill-Sachs lesions. MRI can also be used to identify Hill-Sachs lesions, glenoid bone loss and for the evaluation of the soft- tissue injuries [57]. Diagnostic arthroscopy is useful to look at the subtleties of internal lesions such as deep surface cuff or bicipital lesions.
Extreme sport athletes may have a lower threshold for surgical reconstruction than the general population due to patient goals, expectations, and participation in sports with forced overhead activities, which may increase the risk of recurrence of shoulder dislocation [58, 59]. If there are structural damages to the capsulolabral complex (eg. Bankart or SLAP lesion) and the patient is returning extreme sport, then surgery is often recommended to avoid recurrence [60, 61]. However, literature within overhead throwing athletes is most profound and, although hard to generalize to the extreme sports population, it is to be noted that anywhere between 40 and 50 % of throwing athletes will have a recurrent dislocation [62, 63]. This evidence suggests discussion with the patient’s surgeon should be comprehensive and consider all avenues of treatment options. It is also important to be clear about expectations with the patient as return to overhead activity is complex with a myriad of intrinsic and extrinsic factors.
Details regarding various surgical options are outside the scope of this chapter but common surgeries seen in clinic include arthroscopic surgical rotator cuff repairs, labral repairs, and anterior shoulder stabilization (shoulder stabilization described with suture anchors, proper suture placement, capsulorrhaphy, and occasional rotator interval plication) [31, 64, 65]. Participation in extreme sports is not contraindicated for the above-described surgeries after proper healing times and rehabilitation is implanted within the discretion of the therapist and surgeon. After arthroscopic shoulder stabilization no statistical difference was found in recurrence rates comparing collision athletes with non-collision sports participants [66].
34.3.2 Rehabilitation
Rehabilitation after ASD is paramount to avoiding future dislocation and allowing the athlete to return to their sport.
Surgical rehabilitation following a traumatic anterior dislocation of the shoulder may allow return to sporting activity after an average period of 4–6 months [61].
This is dependent on injury type and/or surgical procedure performed [31]. It is important to note that all rehabilitation programs should be independently developed to the patient with special consideration of intrinsic (age, gender, surgery performed, injury) and extrinsic factors (patient goals, patient expectations, participation, previous injury).
During the initial period of rehabilitation, goals of the therapist and patient are to manage pain, swelling, stiffness, weakness, loss of proprioception and maladaptive postures that may impede proper healing of tissue. As expected, icing, taping and patient education are vital in primary phases of recovery. If the patient is non-operative, special considerations at this phase include bracing. Bracing with sling use may be utilized per patient comfort as evidence is inconclusive on duration and position although bracing in external rotation may be beneficial for the younger athlete [67].
Postural taping, although limited in its research, can provide sensory feedback as it is important that the patient becomes proficient in proper positioning of the scapula during elevation, lowering, retraction and protraction along with dissociation of the glenohumeral joint [61]. This may also play a role in pain modulation for the guarded patient.
The following intermediate phase permits recovery of a full range of movement within pain free planes. At first this occurs passively: keeping the elbow bent at a 90° angle, the therapist guides the limb through a series of shoulder movements, applying a downward caudal translation through the elbow to increase congruency of the glenohumeral joint [61]. Protection of vulnerable positions of the glenohumeral joint may be implied at this phase to allow proper healing of injured structures. These must be performed as far as the pain permits, and should in any case be avoided when there is the risk of instability. Again, special non-operative considerations here would be arthrokinematic mobilization of the glenohmeral joint to allow freedom of movement and assist with pain modulation as well as improvement in range of motion. Although this may also be utilized post-operatively, consideration of surgeon preferences must be noted.
Arthrokinematics of the glenohumeral joint are important to consider but not well defined. In terms of manual therapy, if the therapist is attempting to improve external rotation pain free, Johnson et al. demonstrated that a posterior glide of the humeral head was more effective to increase external rotation than anterior glides, thus challenging the idea that external rotation would be limited by the anterior capsule [68]. Regardless, testing and re-testing impairment of focus after use of manual therapy would prove important to the patient in physiotherapist’s office.
With the patient lying supine and the arm supported, active glenohumeral rotation at 90° abduction can be initiated, seeking to maintain good control of the scapula and glenohumeral joint [61]. The patient can gain proprioceptive feedback by placing the hand of the unaffected side on the front of the shoulder. The addition of a lightweight bar encourages activation of the biceps, another important glenohumeral stabilizer.
Early submaximal isometric exercises for the rotator cuff may be proposed if pain permits in all planes of movement [61]. It is noted, to isolate activation of the subscapularis muscle from that of the pectoralis major, one technique is for the patient to place their hand on a cushion positioned on the belly, with the elbow out to the side. Maintaining this position, the patient should push on the pillow (5–10 s submaximal contraction), avoiding contraction of the pectoralis major secondary to its role in possible poor posturing [69]. This technique is extremely useful because the subscapularis muscle plays a role in glenohumeral stability [70].
The rotator cuff acts as servomechanism crucial to joint stability: it must be activated with closed chain exercises to enhance recovery and stimulate muscular co-activation and proprioception. During this phase, rotator cuff exercises must be performed with the aid of a fixed support to encourage co-activation of the muscles and stability of the scapula, limiting the shear forces across the shoulder joint as much as possible [71–74]. This is of obvious consideration of the therapist secondary to mechanism of injury although not all patients can tolerate this approach, patient specific modifications are appropriately made.
Progression of rotator cuff exercises can then be performed by focusing on repetitions rather than increasing load: the ideal workload is 10–40 % of maximal voluntary isometric contraction [61]. Prone or side lying positions inhibit the effect of the pectoralis major and latissimus dorsi: inappropriate compensation by using these muscles may increase the risk of developing recurrent instability. At this stage, the introduction of closed chain exercises on unstable surfaces such as Swiss ball may enhance neuromuscular control at a reflex level and improve proprioception [75].
The third stage is functional rehabilitation, which includes strength, endurance and dynamic stabilization (Figs. 34.3, 34.4, and 34.5). Plyometric exercises, for example medicine ball throws and dynamic movement patterns that replicate preferred sport can be considered [61]. Lower extremity strengthening, included with upper extremity management, can be utilized for movement retraining; such as single leg squats with dynamic upper extremity control.



Fig. 34.3
Demonstration of external rotation strengthening

Fig. 34.4
Flexion strengthening
Fig. 34.5
(a, b) Scapular strengthening in prone position
During this phase, it is important to focus on patterns of movement biased toward functional tasks specific to the sport practiced. This not only improves control and strength but as a special consideration of extreme sport athletes, speed and confidence need to be ingrained as well. The element of speed should not be introduced into rehabilitation exercises until the strength of the shoulder during elevation and rotation is at least 80 % as compared to the unaffected side [76]. Furthermore, they should not be performed unless the pain is minimal or absent.
If confidence is lacking, there is the risk of compensating with inappropriate movements, increasing the risk of re-injury and instability. Return to sporting activity should be undertaken gradually, in favorable environmental conditions, temporarily avoiding demanding and risky activities such as rough water in water sports, or wet snow slopes in winter sports. It is also useful to determine if the athlete’s specific sporting technique can be improved to prevent recurring symptoms and injury by encouraging the use of the entire kinetic chain in athletic technique, making inappropriate muscle activation at the shoulder girdle less likely.
Overall, shoulder dislocations are common in the extreme sport athlete but with proper treatment and rehabilitation, athletes may return to their sport safely.
34.4 Acute Low Back Pain
Acute low back pain (LBP) is defined as 6–12 weeks of pain between costal angles and gluteal folds that may or may not radiate into lower extremities [77]. Non-specific LBP is defined as LBP not attributed to identifiable, known specific pathology (e.g., tumor, infection, ankylosing spondylitis, osteoporosis, fracture, cauda equina syndrome) [77]. Most patients resolve symptoms however, 31 % of patients with LBP will not fully recover in 6 months [77].
LBP is a commonly managed condition in most care providers’ offices, as two thirds of adults will be affected in their lifetime [77]. For scope of this chapter and following suit of previous two conditions, acute LBP will be focused on from diagnosis to best evidence based management. It is appreciated that chronic LBP differs in management and will be outside the scope of this chapter.
Prevalence rates have been speculated to be higher in endurance athletes, and although no large studies have been performed for LBP in extreme sport athletes, studies have been performed in skiers and rowers, which can be generalized with understanding of its limitation. Endurance athletes in skiing and snowboarding have no increased incidence of LBP than the general population; although a slight increase in prevalence of LBP in rowing type sports secondary to obvious environmental requirements are noted [78, 79]. Incidence rates are also prevalent in water sports, including: sailing, and wind surfing, where 79 % of professional wind surfers report to having LBP [80–83].
34.4.1 Diagnosis and Management
The acute LBP present in most patients is non-specific in origin [84, 85]. Thorough examination should be performed to rule out sinister pathology. Red flags should be systematically evaluated in this population, especially after contact injury; these include: assessing changes in bladder function, major or progressive motor or sensory deficit, saddle anesthesia, history of cancer or suspected spinal infection. Once the first round of screening is exhausted, the medical provider should continue to evaluate for renal, cardiac, or other non-musculoskeletal disorder until the care provider is confident that the patient is presenting with solely a musculoskeletal condition [84].
After considering appropriate placement of patient in physioterapist’soffice, ruling out traumatic injury to the spine is crucial. Although possibly less severe than cervical spine traumatic injuries, secondary to imperative nature of cervical structures, lumbar spine injuries are still important to assess concerning bony pathology for the athlete. Spondylolysis is most common in clinic and is defined as a defect in the pars interarticularis of the vertebral arch. Eighty-five to 95 % of the cases affect L5 and 5–10 % affect L4, with more proximal vertebrae being affected much less often [86]. This can be a relatively common finding in radiologic studies of lumbar spine and it may be completely asymptomatic or can be pain-provoking structures. Painful spondylolysis is particularly a problem in adolescent athletes. Spondylolisthesis may be associated with spondylolysis (about 25 % of occurrences), which is defined by the forward displacement of the vertebral body on the subjacent one [87].
Symptomatic spondylolysis usually presents with focal LBP, occasionally with radiation into the buttock or proximal lower extremities. The onset of the symptoms may be gradual with an acute worsening after a particular event or may suddenly occur after an acute injury depending on the pathogenesis [87–89].
Even if pathogenesis can recognize several mechanisms (Table 34.2), in extreme sports types II, III and IV are of specific interest (Fig. 34.6). Pars interarticularis elongation caused by overuse (type II) is common among sailors, windsurfers, divers, weight lifters and rowers [82, 87, 90]. In addition to this, however, a single traumatic event may precipitate a stress fracture that has been developing secondary to faulty movement behaviors, or may cause the initial microfracture in the pars intertarticularis.
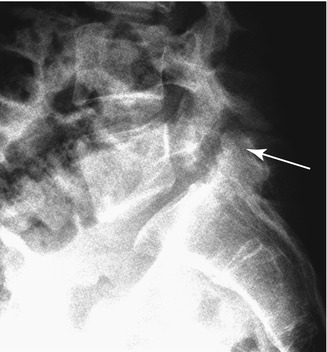
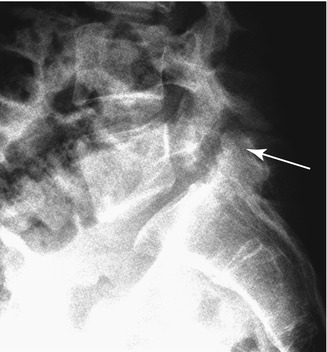
Fig. 34.6
Radiologic demonstration of spondylolysis (arrow) associated with low-grade spondylolisthesis, affecting a 36-year-old female athlete practicing different extreme sports, including windsurfing and diving
Type | Pathogenesis | |
|---|---|---|
I. Dysplastic | Congenital abnormality | |
II. Isthmic | Lytic | Fatigue fracture |
Elongated | Elongated as a result of overuse but not interrupted pars | |
Acute | Acute fracture | |
III. Degenerative | Remodeling of the articular processes | |
IV. Traumatic | Acute fracture in vertebral arch other than the pars | |
V. Pathological | Osteolysis related to generalized or focal bone disease | |
Other area of common focus is disc pathology. Adolescents in elite sports with severe lumbar anterior end plate lesions may have an increased risk for LBP. However, in the acute patient, this may lend little information to treatment in conservative management. Often, asymptomatic patients demonstrate disc pathology indicating possible lack of use for clinical decision-making.
In asymptotic individuals disc degeneration is 37 and 96 %; disc bulges 30 and 84 % of 20 year olds and 80 year olds respectively [91].
Therefore, severe changes may be implied to diagnosis but does not under-credit proper valuation and treatment of the lumbar spine for acute pain [92, 93]. Finally, there is no evidence on the association between degenerative signs at the acute stage and the transition to chronic symptoms [85].
With above noted “normal” changes in lumbar spine, imaging use is often discussed within health care professionals in management of acute LBP. A recent review of the diagnostic imaging literature concluded that imaging does not improve treatment of LBP [85]. Therefore, American and European guidelines do not recommend imaging unless severe pathology is suspected for acute LBP [77, 85].
If the patient is deemed appropriate for rehabilitation management for their acute LBP, discussion changes from pathology to progression of training, correcting faulty technique and use of manual techniques for pain management.
34.4.2 Rehabilitation
As discussed above, a pathology-based approach to diagnosis for LBP has proven difficult because of the inability to identify a structural pathology in the vast majority of patients with LBP [94]. As previously stated, numerous items may require further evaluation in chronic LBP patients that may differ in treatment methods to that of an extreme sport athlete with acute LBP. In lieu of these points, a classification system may be useful for organization of management of patients with LBP. Many classification systems have been presented, some based on pathology, and some based in rehabilitation methods.
Patho-anatomical models are challenging for management in the physiotherapists’ office as pathology can correlate with <20 % of reasons for LBP [94]. Therefore, Fritz et al., proposes a method to gather data and subgroup this overall heterogeneous group to guide therapists in their decision making processes. The four categories include: manipulation, stabilization, specific exercise and traction [95–97]. The remainder of this section will evaluate literature within the first three categories as these are used primarily for the extreme sports athlete with acute LBP and cross-examine them with international guidelines.
European and United States guidelines for acute non-specific LBP appear similar including: education to remain active, medication if necessary for pain management, and spinal manipulation [77, 92]. It is generally accepted that bed rest is not recommended to patients secondary to increased weakness and stiffness along with fear avoidance behaviors [98].
Although medication management and education may be enough to treat many with acute LBP,, extreme sport athletes may have higher demands of return to athletics and may require specific guidance to their sport and/or manual techniques to hopefully shorten duration of episode [77].
Often considered in early phases of non-specific acute LBP is spinal manipulation. In most guidelines, spinal manipulation is considered to be a therapeutic option in first weeks of LBP. The UK, US, New Zealand and Danish guidelines state that spinal manipulation can be a useful tool to modulate pain [98–101]. Australian, Israeli and Dutch guidelines do not recommend manipulation in acute LBP [102–104]. Challenges in developing heterogeneous population samples in this group provide difficulty in clear delineated guidelines for management. Therefore, an often-referenced study by Flynn et al., and subsequently validated by Childs et al., demonstrates use of prediction rule criteria to identify responders to this treatment [105–107]. Patients who benefit most from spinal manipulation presented with four of the following five criteria: symptom duration less than 16 days, symptoms not distal to the knee, score of 19 or less on fear avoidance measure (work subscale of the Fear-Avoidance Beliefs Questionnaire), one hip with more than 35° of internal rotation and one hypomobile lumbar segment [105]. Patients with five of these factors demonstrated a 50 % improvement in disability within 1 week of onset of care [98, 107].
Subsequent category of specific exercise is commonly referred to as McKenzie method, directional preference, or mechanical diagnosis and therapy. Referencing back to Fritz et al., this is considered most classically used for patients with symptoms past the knee [97]. United States and Danish recommendations state that McKenzie method and spine stabilization exercises to decrease repeat episodes of LBP may be useful in management of acute LBP [77, 85].
Again, recommendations for stabilization exercises are not clearly stated across country-to-country guidelines. Common to the theme of manipulation, this may be secondary to heterogeneous population samples concerning LBP. Per European guidelines, back-specific exercises (e.g., strengthening, flexion, extension, stretching) are considered not useful during the first weeks of an episode. Yet again, variability of guidelines lends little guideline to rehabilitation programs and therapist choices of interventions therefore, best available evidence should be considered when managing the extreme sport athlete with acute LBP.
Even with variability within literature and guidelines, management of acute LBP in extreme sport athletes seems to state importance of use of manual techniques in addition to progression to any pain free strengthening program with advance to return to sport specific strengthening. Although generally recommended, strengthening is not strongly supported within literature for acute LBP; understanding of this population’s demands is imperative and varies from general population. Focus should be placed on re-training rectus abdominus, transversusabdominus, internal oblique, and multifidus for stability [108–113] (Figs. 34.7 and 34.8


). Progression of these exercises begins in supine, transitioning to quadruped, then in closed kinetic chain positioning and finally transitioned into dynamic environments often encountered by the athlete.

Fig. 34.7
Transverse abdominus strengthening

Fig. 34.8
Bridging with marching
The athlete should demonstrate adequate positioning of the spine to reduce lumbar loading forces seen in their sport to reduce pain and future episodes and also to increase patient’s comfort level with returning to activity. For example, transverse abdominus is retrained supine with drawing in maneuver, progressed to quadruped control, then into squat form retraining, and finally sport specific retraining to ensure athlete maintains control of lumbar spine in static and dynamic environments. Once the athlete demonstrates spine control, confidence and understanding of back management patient is discharged to independent program.
Overall, management of the athlete can derive along classification systems with a dose of expert opinion. Use of manual techniques to reduce acute pain are indicated in non-specific LBP, use of directional preference to reduce initial pain and/or centralize symptoms, progression of strengthening from static to dynamic environments are all commonly used, and evidence based techniques are used internationally for this population.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








