CHAPTER 63 Rehabilitation Methods
INTRODUCTION
About two-thirds of all people will experience neck pain at some point in their lives.1 Diverse rehabilitation methods and techniques are employed by various healthcare clinicians to treat individuals experiencing neck pain. Most of the treatments applied lack substantial scientific support for their application, with very limited information available from randomized, controlled trials into the effectiveness of individual treatment modalities. As substantial healthcare resources are utilized for this condition, more high-quality studies are needed to determine which of these interventions are effective and provide long-term pain reduction and improvement in function.
Neck pain may resolve within days or weeks but often recurs and can become chronic.1 The true natural history, or the frequency and timing of its recovery without treatment, is unknown. In one study, 90% of patients with mild neck pain reported improvement within 30 days, while 76% of those with moderate pain reported improvement at 90 days, independent of treatment.2 Although acute episodes often improve, spinal pain is frequently recurrent, with 43% in one survey reporting 11 or more episodes over a year.3 The frequency with which neck pain becomes chronic and unrelenting is thought to be about 10% and causes severe disability in 5%.1 There is very limited evidence regarding prognostic factors.4 Whiplash injuries are more likely to cause continuing symptoms, with up to 40% reporting continued symptoms 15 years after the injury.1
As there is little scientific evidence supporting the use of any of the current physical modalities and ample evidence that the application of movement provides the best stimulus for repair, this chapter focuses on delineating exercise and manual therapy approaches for the interventional spine physician. Exercise and maintenance of normal activity have support in systematic reviews,1,5–8 while most conclude that rest and passive therapy can have a negative effect. There are numerous concepts of utilizing exercise and manual therapy with some overlap in reasoning and techniques of application. The authors will highlight features of commonly used approaches that have some support for their efficacy.
SOURCES OF NECK PAIN
In the clinical practice of treating acute neck pain, it is difficult to base treatment on a pathoanatomic model. The source of pain could be discogenic, zygapophyseal, ligamentous, myofascial, or a combination. Radiologic imaging cannot conclusively determine the pain generator. Neck pain correlates poorly with spondylosis as it is equally present in those with and without neck pain. Furthermore, many patients with neck pain show no signs of spondylosis.9,10 Magnetic resonance imaging cannot reliably identify discogenic pain. Schellhas found normal-appearing discs on magnetic resonance imaging (MRI) proved to have painful annular tears with discography.11 Additionally, injuries to the zygapophyseal joints frequently are undetectable with X-ray or MRI.9 Many diagnoses later confirmed with diagnostic injections exhibit similar initial symptomatology, with overlap between zygapophseal, discogenic, and myofascial pain patterns.12,13
Just as radiology does not always conclusively provide a diagnosis, neither does a clinical examination.12 Often, a structural source is suspected based on particular pain behaviors and clinical presentation, but no clinical tests have conclusively been shown to prove the structural source of the pain. Tender points or trigger points are neither reliable nor a valid sign of the cause of neck pain.12 Clinicians often speculate that patients who present with a large obstruction to movement in one direction that lessens with repetition of that movement, as well as centralization of pain with repeated movements, have pain of discogenic origin. Likewise, studies have shown that abnormal quality of movement, abnormal end feel, and pain reproduction upon examining the passive accessory movements of the joint are predictive of zygapophyseal joint pain.14 Speculation and hypotheses about pain sources should not be interpreted as dogmatic certainties.
In the case of chronic symptoms, further diagnostic information may be available from diagnostic injections or cervical discography. Despite the potential for these procedures to assist in diagnosis, it should be kept in mind that both a symptomatic disc and a symptomatic zygapophyseal joint have been identified in a high percentage (41%) of chronic neck pain patients.9 Furthermore, Bogduk et al. also reports a potentially high false-positive rate with provocation discography.12
Another complicating factor in diagnosing an anatomical pain generator is that due to alterations that occur in the central nervous system with chronic pain, there may be less of a direct relationship between the pathology and the resultant symptoms. If pain persists beyond the normal healing time, persistent nociceptive input from the peripheral nervous system may cause changes in the central nervous system, ultimately reducing thresholds for pain and causing increased responses to afferent input. Generalized muscle hyperalgesia has been shown to occur in chronic whiplash syndrome, confirming this central hyperexcitability.15,16 As a result of the altered nervous system, nociceptive signals can be initiated, producing a ‘phantom’ pain in an area that previously had tissue damage.9
Changes in the muscular control system have been shown to occur, which may be a contributing factor in chronic neck pain. Irrespective of the initial tissue injury, increased muscle fatigability, altered muscle activation patterns, and decreased neuromuscular efficiency have all been shown to occur.15 Rehabilitation may need to address these multiple physiologic changes.
REHABILITATION INTERVENTIONS
Exercise for acute nontraumatic neck pain
Exercise interventions are deemed essential for the effective management of patients with neck pain and are commonly used by clinicians in the treatment of acute nontraumatic neck pain. Regardless of the involved musculoskeletal tissue, the beneficial effects of early motion are well supported in the literature. Early motion results in strengthening tendons and ligaments, restoring full range of motion, preventing adhesion formation, improving collagen alignment, and preserving articular cartilage.17,18 The optimal function of musculoskeletal structures is restored and maintained by activity. Exercise involves active participation of the patient and has been shown to be superior to passive treatments.1 Active participation gives the patient a sense of control over his or her symptoms and helps lessen the fear of movement. Those who fear movement and re-injury often avoid activity, thus creating disability and depression.19 According to Vlaeyen,20 those who confront their pain and follow a progressive return to normal activity are more likely to make a full recovery.
The McKenzie method of mechanical diagnosis and therapy
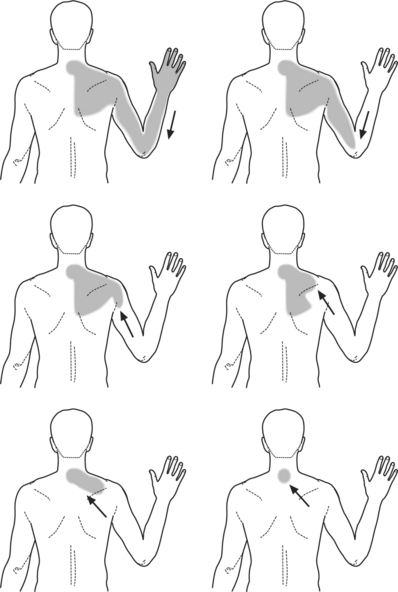
One commonly applied method of determining what type of exercise to provide is called Mechanical Diagnosis and Therapy, developed by Robin McKenzie. McKenzie developed an assessment tool that utilizes repetitive motion in cervical flexion, extension, sidebending, and rotation.21 The symptomatic and mechanical response to these motions gives the clinician a framework to determine how to most effectively apply movement or exercise. Many times, a movement is found during assessment that causes the pain to reduce in intensity, or other times to ‘centralize’ and then subsequently to resolve. Centralization, first observed by McKenzie, describes a ‘situation in which pain arising from the spine and felt laterally from the midline or distally is reduced and transferred to a more central or near midline position when certain movements are performed.’22 This process occurs in those with arm pain as well as in those with axial pain only (Fig. 63.1). Pain that is referred into the scapular and upper trapezius region may localize to the midline of the cervical spine. Ultimately, the midline pain is also eliminated with continued performance of the centralizing movement.
In a sample of 86 neck pain patients, Donelson et al.23 found centralization occurred in 45.3% of patients. Sixty-seven percent centralized with extension tests while 33% centralized with flexion. The examiners in this trial only assessed flexion and extension. As centralization also may occur with lateral movements, including these in the assessment may have increased the centralization rate. Centralization most commonly occurs in patients with a significant obstruction to one movement. As the pain centralizes, the obstruction to movement in that direction progressively becomes less, creating a symptom and mechanical response that occur together. McKenzie theorizes that mechanical displacement or internal derangement is lessening as centralization is occurring.21
Centralization may occur immediately during the first assessment or may occur more gradually over a few days of repetitive motion applied in one direction. This rapid change in the patient’s condition is inconsistent with the slower recovery more often observed with natural history. Werneke24 assessed 289 acute cervical and lumbar patients for the occurrence of centralization. Thirty percent centralized in one session, while another 46% were classified into a ‘partial reduction’ group. This group had a slower movement of their pain toward the midline, occurring in anywhere from 2 to 7 sessions.
If centralization and abolition of the pain occurs rapidly, it makes the use of any other type of treatment for the pain unnecessary, as the patient has learned to eliminate the symptoms independently. Such favorable findings should clearly guide the patient’s treatment by instructing the patient to continue to utilize the exercise that centralized or eliminated the symptoms. For instance, if a patient can eliminate the symptoms with lower cervical extension (Fig. 63.2) (i.e. retraction followed by extension), the patient is instructed to perform this exercise hourly and maintain very erect posture in between the performance of the exercise. An erect posture is very important, as a slouched sitting position will allow the lower cervical spine to fall into flexion, thus creating a return of symptoms. If at any point the pain begins to return, the patient independently performs the exercise that returns the pain to the midline and then abolishes it.
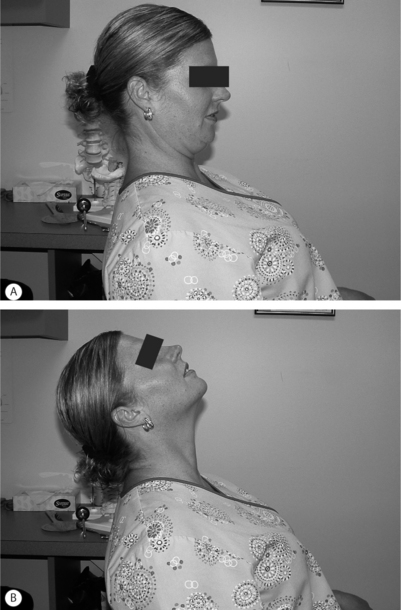
Fig. 63.2 Cervical retraction followed by extension.
(Adapted from Figure 16.1 in McKenzie, 1990)21.
Centralization has been associated with greater improvements in pain severity, improved functional disability scores, and better return to work rates.25,26 In Werneke’s study, the centralizers had fewer visits than noncentralizers (3.9±4 versus 8±0.4). Patients categorized into centralization or partial reduction had greater improvements in pain intensity and perceived function than noncentralizers. Conversely, failure of centralization has been associated with poor outcomes and is highly predictive that the patient will not make improvements with this type of exercise approach.25 Werneke found if centralization did not occur by the seventh visit, no improvement in pain intensity or perceived function occurred.
The performance of repeated movements also helps distinguish chemical from mechanical pain. One movement in each direction often does not provide enough information to distinguish between mechanical and chemical pain. Chemicals (histamine, bradykinin, serotonin, etc.) are released by cells in damaged tissue and cause pain production when their concentration is sufficient to irritate free nerve endings. Mechanical pain occurs when normal tissue is held for prolonged periods at end range (as in the case of poor posture), when displacement occurs within the motion segment causing increased tension on certain structures, or when stress is placed on tissue that has healed in a shortened position.22 If pain is primarily chemical in nature, the pain will be constant and repeated movements in all directions will aggravate the pain.27 In these cases, mechanical therapy will be unsuccessful until the chemical component is addressed. Mechanical pain, on the other hand, may be constant or intermittent and the repetitive movement assessment will reveal what increases and decreases mechanical deformation. The information gained about the behavior of the lesion allows the clinician to specifically tailor the treatment to addressing the chemical component or correcting the faulty mechanics.
Segmental stabilization exercises
Another emerging method of applying exercise is based on the work of an Australian group of researchers, including Sterling, Falla, and Jull.27–29 They have published a series of research papers investigating motor activity in patients with neck pain. Prior to their work, a reduction in strength of the cervical flexors and extensors had been shown in those with neck pain.30–32 Vernon33 also found a progressive anterior-to-posterior muscle imbalance, with the cervical flexors becoming relatively weaker as compared to the extensors. The Australian group’s contribution is their series of studies showing that both those with insidious-onset neck pain and those with whiplash-associated disorder develop deficits in motor activity and control. This manifests itself as altered patterns of cervical muscle recruitment and deficits in particular groups of muscles.29
Maintenance of the stability of the cervical lordosis requires action of the superficial larger muscles that cross more than one joint, such as the sternocleidomastoid and the scalenes, as well as action of the segmental vertebral muscles, the longus colli, and the longus capitus muscles. Winters and Peles34 showed, using a computer model, if only the superficial muscles were used to produce movement of the neck, regions of local segmental instability were produced. Muscle activity of the deep segmental muscles was required to stiffen or stabilize the segments, especially in functional midranges.
Jull et al.35 and Falla et al.36 have found dysfunction in the neck flexor muscles in both traumatic and insidious-onset neck pain. They developed the craniocervical flexion test (CCF), or nodding of the head (Fig. 63.3), which is a task that in normals utilizes the deep cervical flexors (longus colli, longus capitus, rectus capitis anterior, and rectus capitis lateralis) and the superficial neck flexors (scalenes and sternocleidomastoid).37 During performance of the CCF test, a pressure unit was inserted behind the neck to monitor the flattening of the cervical lordosis that accompanies this motion. Subjects were asked to progressively increase the pressure in the unit by performing five repetitions of CCF, increasing the pressure by 2 mmHg with each repetition. The control group was able to do this quite accurately, while patients with neck pain demonstrated large pressure shortfalls. With electromyogram (EMG) recordings, they demonstrated that the diminished ability to perform this task accurately resulted from reduced activity in the deep cervical flexors. EMG recordings also found increased activation of the superficial neck flexors.
This deficit in the deep neck flexors has been shown to occur within 1 month following whiplash injury, but the timing of its onset has yet to be determined in those with a spontaneous onset of neck pain. In the lumbar spine, Hides et al.38 found deficits in the deep segmental stabilizers (transverse abdominus and multifidus) occurred early within an episode of acute back pain.
The Australian researchers advocate having patients perform exercises in an attempt to restore the action of the deep cervical flexors and minimize the action of the superficial flexors.28 Patients perform craniocervical flexion exercises through their full range of motion in an attempt to retrain the segmental cervical muscles. They are given feedback to minimize the contraction of the superficial flexors. The theory is that performance of these exercises will minimize recurrent episodes of neck pain. This is based on research in the lumbar spine which demonstrated that deficits of the segmental stabilizers (the transverse abdominus and the multifidus) remained following an acute low back pain episode despite resolution of pain.39 In a follow-up study, patients were given a specific exercise program to train the deep stabilizers of the lumbar spine. Recurrence rates over the next year were 30% for those who performed the specific exercises, compared to 80% for those who did not. Future studies in the cervical spine will need to address if deep stabilizer deficits spontaneously resolve with pain, if specific exercises are needed, and if these exercises have an effect on recurrence rates.
In addition to training the deep cervical flexors, these authors advocate exercises to train the tonic postural function of the scapular muscles.40 The forward head position, so commonly adopted by those with neck pain, involves increased thoracic kyphosis and abduction of the scapula. The scapular stabilizers, in particular the lower trapezius and serratus anterior, play a postural supporting role when sitting in an erect position, holding the scapula in a relatively adducted and depressed position. It is proposed by some authors41 that those who chronically sit with forward head and thoracic kyphosis lose the postural function in the scapular muscles, although there is no research evidence to support this finding. Exercises for these scapular muscles are similar to training of the deep cervical flexors; training initially involves holding a low-level static contraction to improve tonic postural control. Patients are taught to retract and depress their scapula in a prone position and then attempt to carry it over to a sitting position.
Evidence for exercise for acute nontraumatic neck pain
Most randomized, controlled trials (RCTs) of exercise for acute neck pain have studied patients with whiplash. However, there is some evidence that specific exercises may help certain patients recover faster from acute neck pain episodes. The work of Donelson et al.23 and Werneke et al.24 showed a frequent occurrence of directional preference. In acute spinal pain, many studies24–26 have indicated that patients with a directional preference recover more swiftly and predictably using exercises, posture, and activity modifications determined by their directional preference. In one RCT that included patients with acute and chronic neck pain, Kjellman et al.42 compared three groups. Group one received exercise prescribed utilizing the McKenzie method, group two received general exercise, and group three received ultrasound. The McKenzie group had a more rapid improvement in pain intensity during the first 3 weeks and lower pain scores at 6 months. At 12-month follow-up, all three groups showed significant improvement with no significant difference among the groups. This study adds more evidence that directional preference exercise may help patients recover faster, but also shows the tendency for most acute neck pain to get better with time, irrespective of treatment.
Exercise for acute traumatic neck pain
Most systematic reviews of treatment for whiplash injury conclude that an active approach is superior to passive treatment.43,44 The optimal management of whiplash-associated disorders is unknown, but some concepts for improving outcomes are emerging. Musculoskeletal dysfunctions observed following whiplash are a decreased ability to move the cervical spine, altered patterns of muscle recruitment, and deficits in kinesthetic awareness, balance and eye movement control.15 Rehabilitation of these deficits will be addressed in this chapter in those with neck pain, decreased range of movement, and/or point tenderness with no neurological signs (Quebec Task Force grade II).45 The authors present evidence in support of an early active approach to management.
Lesions may occur in virtually any cervical structure including the ligaments, muscles, discs, zygapophyseal joints, and the bony elements. Experimental studies have shown that with rear-end collisions the torso motion causes the vertebrae to extend from the lowest vertebra to the upper vertebrae, causing the inferior articular facet to collide with the superior facet of the lower vertebrae.46 Kaneoka et al. hypothesized that this collision impinges on and inflames the synovial fold in the zygapophyseal joint. In fact, painful facet joints have been found in 54% of those with chronic pain associated with whiplash.46 Other common injuries are reported to be posterior disc herniations and anterior annular rim lesions.47
Just as with nontraumatic neck pain, radiologic imaging does not provide a conclusive diagnosis. Yoganandan et al.48 simulated a whiplash injury in four cadavers. The purpose was to determine type of injuries sustained with whiplash and whether these injuries could be viewed with conventional imaging. Impact speed was comparable to 75–90% of those who suffer a whiplash injury. There results suggest that multiple injuries occur that cannot be visualized with X-ray or CT scan. These included capsular tears of the zygapophyseal joints, tears of the ligamentum flavum, and disc anulus ruptures.
Regardless of which tissue is injured, a uniform sequence of events shaping repair is set in motion. When developing a rehabilitation program for optimizing repair and preventing chronicity, determining the stage of healing and understanding the primary events occurring will improve outcomes. The primary means of tissue repair is by formation of granulation scar tissue.49 The formation of scar tissue is a three-phase cycle and is a normal reparative process following an injury. A review of this highly organized process and the role of graded movement in assisting optimal healing make it apparent why active rehabilitation of whiplash injuries appears to be superior to passive rehabilitation.
Tissue healing following injury starts immediately with the inflammatory phase and generally lasts 1–5 days.49 Vasodilation and a release of prostaglandins and histamines in the area of damage results in increased blood flow. Peripheral neutrophils and monocytes migrate into the injured area to destroy bacteria and maintain a clean environment.49 These tissues create an inflammatory edema that seals the area to allow healing to occur. Neovascularization brings increased oxygen to the damaged area. Optimal management includes rest of the structures involved for this very short period of time. Excessive inflammatory edema causes larger quantities of scar tissue.19 Ice during this phase will help minimize edema. Ensuring a good sitting, standing, and sleeping posture (as opposed to the commonly adopted forward head position with increased thoracic and cervical kyphosis) decreases the stress placed on the tissues and subsequently decreases pain.
The fibroblastic phase begins in the middle of the first week following injury.50 This is when the necessary components for repair are accumulated and the architectural make-up of the tissue is being formed.49 Scar tissue is created and strength is imparted to the tissue, depending on the forces placed on it. Fibroblasts synthesize collagen, which is the substance of scar tissue, and glycosaminoglycans, which fill in the space in and around collagen fibers. The glycosaminoglycan ground substance provides lubrication and acts as a spacer between moving collagen fibers. Immobilization during this phase causes a loss of ground substance, which creates cross-links between the collagen fibrils, rendering them immobile.51 Additionally, fibrofatty tissue proliferates within the joint and forms adhesions as it matures into scar tissue. Articular cartilage joins with this tissue and degrades.52 Ligaments have been shown to loose their orientation, and their insertions into bone are weakened.
Mobilization during this phase is essential. The joints and cartilage are stretched and lubricated by synovial fluid and their metabolic activities are enhanced.52 Cartilage repair in injured joints that were subsequently treated with CPM showed marked improvement in the rate and end point of the healing process.51 DePalma et al.53 noted that early motion and weight bearing had a beneficial effect on the repair of full-thickness cartilage defects. Salter54 and Houlbrooke et al.55 have also reported on the beneficial effects of early passive motion on joints and articular cartilage. Regular passive motion in progressively increasing ranges kept the needed space between collagen fibers and allowed better alignment of collagen and cros-links. Early mobilization has also been shown to improve outcomes in tendon repair.51
To gain the beneficial effects of movement during this phase, movements should be started once the initial inflammatory stage is nearing completion and the fibroblastic phase is underway. Several authors21,56 have outlined programs to determine how much movement to apply during healing. To allow the patient to gain confidence and to prevent a return to the inflammatory phase, movement should start in midrange with low repetitions, with a progression to end range movement as the patient tolerates it. If movement is too painful in a loaded position, the patient may need to lie down. If a movement hurts as it is occurring, but the pain ceases when the movement is complete, an acceptable amount of movement has occurred. If pain continues for more than a few minutes after the movement is complete or the pain becomes constant in nature, the movement was likely too far and the repetitions or the vigor with which they are being applied should be decreased.
The remodeling phase begins at about 21 days following injury and provides the final form to the scar. All of the collagen mass is assembled, but the tensile strength is only 15% of normal.49 This process of scar remodeling continues for up to 12 months as collagen turnover rearranges the scar tissue, depending on the stresses placed on it. Many authors have demonstrated that the absence of controlled stress results in a weak, fibrous scar.54,57 Other researchers have shown that the application of stress during healing can lengthen a scar and positively influence the characteristics of the collagen repair. In response to internal and external influences, scar differentiates to become quasi-specific. One of the goals of motion during this phase is to enhance the potential of the scar to resemble its original tissue.
Motor control exercises
The Whiplash and Cervical Spine Research Unit at the University of Queensland, Australia, has provided a significant amount of new information about physical and psychological changes with acute whiplash injuries. They followed 76 whiplash patients from a few weeks until 6 months postinjury and found changes in motor control, kinesthetic awareness, and certain psychological factors which might help predict chronicity.
Changes in motor function develop early after a whiplash injury and may need to be addressed in a rehabilitation program.58 Changes in motor activity and control observed are the same as for insidious-onset neck pain: increased EMG activity of the superficial neck flexors, and decreased activity of the deep segmental neck stabilizers. Altered patterns of muscle recruitment were apparent in all whiplash patients within a month of injury and persisted to 6 months even in those patients who reported full recovery of pain. Altered patterns of muscle activation have also been shown in the shoulder girdle with chronic WAD.59–61 The Whiplash and Cervical Spine Research group propose having patients perform craniocervical flexion exercises for WAD just as described for insidious-onset neck pain prior to a general strengthening program. The efficacy of such an exercise program has yet to be investigated in whiplash patients.
Sterling et al.58 have shown that kinesthetic disturbances occurred soon after injury. Joint position error (JPE) was measured by blindfolding subjects and then asking them to perform a series of movements and then return to their original head position. JPE was compared between the whiplash group and the controls. In those with moderate to severe symptoms, there was a statistically significant higher JPE, present within a month of injury and persisting at 6 months of injury. Whether specific exercises addressing these deficits improves outcomes in acute whiplash patients is still to be addressed.
Sterling15 have also found some sensory and psychological changes which they believe may help predict chronicity of WAD. Local cervical mechanical hyperalgesia (decreased pressure pain thresholds using pressure algometry) occurred in the acute stage of whiplash injury, but resolved by 2–3 months in those who recovered and those with persisting mild symptoms. In contrast, those with persisting moderate to severe symptoms not only had local hyperalgesia, but widespread mechanical and thermal hypersensitivity soon after injury. According to Sterling et al., optimal initial management of this subgroup would include pharmaceutical management, and a slower approach to restoring movement with minimal pain provocation.
Additionally, the early presence of moderate levels of acute post-traumatic stress was a distinguishing factor of those who became chronic in their group of patients. The whiplash research group gave all participants a battery of questionnaires measuring psychological distress. The group that had persistent moderate or severe symptoms could be distinguished from the others even a few weeks after injury. All whiplash patients displayed initial psychological distress, but the group with significant persistent symptoms had one distinguishing factor. They had moderate levels of acute post-traumatic stress as measured on the Impact of Events Scale.62 Sterling et al. proposes that utilization of psychological testing scales would help institute early psychological referral for this subgroup who might benefit from a multiprofessional approach to their management. Traditionally, this type of treatment has not been instituted until it becomes clear that symptoms are not resolving.
Evidence for exercise interventions in acute traumatic neck pain
In a randomized, controlled trial, Rosenfeld et al.56 compared an early active movement program to instruction to rest for 2 weeks with optional use of a collar, followed by movement of the head 2–3 times a day. The active group performed cervical rotation every hour starting 2–3 days after injury. If symptoms were still present at 20 days, the evaluation was supplemented by a mechanical evaluation using repeated movements, as described by McKenzie, to determine if any direction of movement might be more beneficial than others. There was also a third group that performed the active intervention but waited until 2 weeks postinjury to begin the exercises. At 6 months postinjury, the groups that moved frequently, instead of gradually after a period of rest, had significantly greater pain reduction. The group that did the best was the one that started movement the earliest. Most importantly, only 10% of the actively treated patients had symptoms at 6 months, compared to 50% of the patients who were given standard of care. The active group only required an average of 4 visits, and no passive modalities were used with any of these patients.
More information can be gained when comparing this study to the RCT of Sodelund et al.63 Two groups of acute whiplash patients performed range of motion exercises three times daily. One group also received kinesthetic exercises. At 6-months follow-up, the average patient in both groups remained in pain and disabled. Comparing the study of Sodelund et al. to that of Rosenfeld et al. may provide information on dosage. Only 10% of subjects in the Rosenfeld et al. study who exercised their necks hourly remained in pain at 6 months, whereas most subjects in the Sodelund et al. study who exercised their necks three times a day remained in pain at 6 months. Additionally, exercises in the Rosenfeld et al. study were not standardized to all patients, but tailored, based on each patient’s specific response.
Most studies looking at the efficacy of soft collars do not support their use.64,65 Immobilization not only has physiologic ramifications, but enhances fear of movement and disability. When immobilization in a soft collar combined with time off of work was compared to a group who were told to act as usual during the first 14 days following injury, there was a significantly better outcome for the act-as-usual group in terms of pain, memory, and concentration.66
Two other studies have been published comparing early movement to use of a collar. Pennie and Agambar67 found no difference at 2-year follow-up between a group given a collar with instructions for subsequent self-mobilization to a group that received traction and physical therapy. Crawford et al.68 placed one group in a collar for a few days and another group in a collar for 3 weeks and then had them both perform self-mobilization exercises. The group in the collar for the shorter time returned to work much earlier (17 versus 34 days) although there was no difference in pain and range of motion at 1-year follow-up.
Summary of exercise for acute neck pain
Exercise for chronic or recurrent neck pain
McKenzie method for chronic neck pain patients
In other patients with chronic neck pain, avoidance of particular movements secondary to pain or poor posture can create shortened or dysfunctional tissue.21 In this case, repetitive motions reveal a particular pattern of symptom production: movement into the shortened end range produces pain which ceases once the movement is complete. In these cases, the patient is taught to exercise into the direction or directions that are limited, producing the pain with each repetition as long as the pain stops when the exercise is ceased. This is an effective way to remodel tissue without creating microtrauma. It is not unlike a patient restoring elbow flexion and extension after a fracture once the cast has been removed. To gain motion, patients must perform the movements frequently.
General strengthening programs
Numerous studies have shown reduced strength and endurance in the cervical flexor and extensor muscles in patients with neck pain.28 There are many methods available to perform strengthening. Strengthening programs currently used run the gamut from extremely low-tech to extremely high-tech. Most exercise programs focus on the cervical muscles as well as the scapular stabilizers. A typical low-tech strengthening program either involves isometrics or utilizing a head lift in supine and prone positions to strengthen the flexors and the extensors, respectively. Resistance can be increased with a free weight or by elastic bands. Scapulothoracic exercises may involve free weights or closed-chain exercises, such as push ups. The difficulty of closed-chain exercises can be increased infinitely by decreasing the stability of the surface (exercise balls) or performing them unilaterally, tasks for the very highly fit.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree