Rehabilitation for Children with Limb Deficiencies
Joan E. Edelstein
Learning Objectives
On completion of this chapter, the reader will be able to do the following:
4. Compare prosthetic options for children of various ages who have upper- or lower-limb deficiencies.
6. Design a habilitation program for an infant born with multiple limb deficiencies.
Maria, who was born without a left forearm and hand, Bobby, who caught his foot in a powered lawn mower, and George who is recovering from femoral sarcoma have different skeletal, neuromuscular, learning, and psychosocial challenges from those of adults with amputation. Children share some rehabilitation issues with adults, particularly the basic components of the prosthesis and the essential elements of postoperative care. Other considerations, however, are unique. Because children are smaller than adults, the choice of prosthetic components is not as broad. Youngsters grow and develop through the rehabilitation process. In addition, young people legally, financially, and emotionally depend on adults for their medical, surgical, and rehabilitation care.
Clinicians concerned with comprehensive management of children with limb deficiencies need to consider the causes of limb deficiency, the relationship of developmental milestones to prosthetic selection and use, and the psychosocial factors that affect children in order to design optimal programs.1–3 Care of the infant born with a limb anomaly is habilitation, whereas management of someone who undergoes amputation because of trauma or disease is rehabilitation. Unless the distinction is relevant, however, habilitation and rehabilitation are used interchangeably in this chapter. Similarly, limb deficiency is used to designate both congenital and acquired limb absence. The overall goal of physical therapy is to facilitate the normal developmental sequence and prevent the onset of secondary impairments and functional limitations such as contractures, weakness, and dependence in self-care.
Comprehensive considerations in childhood
The philosophy of this chapter is that the child with a limb deficiency is first and foremost a person, with the beauty, delight, and promise inherent in all young people.
Classification and Causes of Limb Deficiencies
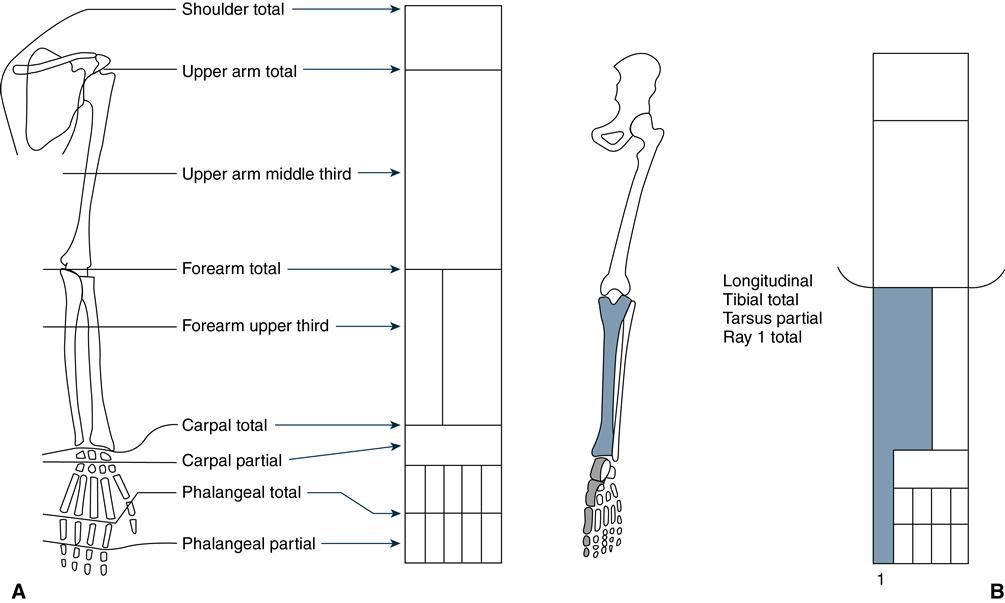
The International Organization for Standardization approved a system of limb deficiency classification in 1989 (Figure 29-1).4 Congenital limb anomalies are described anatomically and radiologically as transverse, in which no skeletal elements exist below the level of normal development, or longitudinal, in which a reduction or absence of elements is present within the long axis of the limb, with normal skeletal elements usually present distal to the affected bone (Figure 29-1). This system replaces older terms, such as phocomelia (distal segments attached to the torso), amelia (complete absence of a limb), and hemimelia (partial absence of a limb).
Limb deficiency is caused by congenital deficiency, trauma, cancer, and disease. In the total U.S. population, peripheral vascular disease among adults accounts for more than 80% of amputations, with a greater than 25% rate of increase in the latter half of the twentieth century. Rates of trauma- and cancer-related amputations are declining, whereas the incidence of congenital deficiencies remains stable.5 A recent survey of all children with lower-leg deficiencies in The Netherlands indicated 73% with congenital deficiencies and 27% with amputations as a result of malignancies (9%), trauma (8%), infection (4%), and other pathologies (6%).6
Among those with congenital limb anomalies, transverse deficiency of the upper limb, especially the left extremity, is the most common.7 McGuirk and associates found the overall prevalence of limb deficiency among 161,252 newborns to be 0.7 per 1000 births. Thirty percent of the defects were caused by genetic factors, 4% by teratogens, 35% by vascular disruption, and 32% by an unknown cause.8
Powered lawn mowers9–11 and all-terrain vehicles12 are responsible for many traumatic amputations among children and adolescents.
Long-term followup of the Childhood Cancer Survivor Study, which is composed of 14,054 individuals who have survived for 5 or more years after cancer treatment, indicates that osteosarcoma or Ewing sarcoma of the lower limb or pelvis is the most common tumor; the median age at diagnosis is 14 years.13 Some patients with tumor are treated by various limb-sparing procedures, and others undergo amputation. Long-term outcome is similar, although more patients with amputation used walking aids and were less satisfied with their status as children.14–19
Developmental Milestones
Motor skills develop in a predictable sequence, with well-established milestones that mark achievement of important functional abilities.20–22 In the absence of cerebral maldevelopment or malformation, the infant born with a limb anomaly or a young child who undergoes amputation demonstrates physical control at approximately the same time as an unaffected child does. Limb deficiency, however, often alters how the developmental tasks and activities are performed. For example, the 5-month-old infant who has only one intact leg will develop a distinctive style of crawling. Therapists who conduct initial evaluations of these children focus on muscle strength, range of motion, gross motor patterns, coordination, attention span, and interests.
All children, not just those with limb deficiency, display varying rates of neuromuscular development. Chronological age cannot provide a complete picture of a child’s developmental level. In this chapter, milestones pertaining to upper and lower limb development are related to habilitation of children with limb disorders.
Physical conditioning programs, especially active sports, are important to enhance general health and endurance, particularly for those who wear a prosthesis. Play and games increase coordination and improve strength. Swimming is particularly beneficial because it does not traumatize the limbs and does not require a prosthesis; nevertheless, some children may be reluctant to display an anomalous limb.
Accommodating Growth
All children grow, regardless of congenital anomalies or amputations. Prosthetic planning should incorporate measures to maintain comfortable socket fit and symmetrical limb length. The preschool-age child may need a new prosthesis almost yearly. Those in grade school often require a new prosthesis every 12 to 18 months, and teenagers outgrow prostheses every 18 to 24 months.1
Longitudinal growth is typically more rapid than circumferential growth, a troublesome fact for children with lower-limb deficiency. Reconstructive surgery, especially circular (Ilizarov) fixation, suits children with minimal length discrepancy, whereas amputation remains preferable for those with severe limb loss.23 Too short a lower-limb prosthesis disturbs the quality and efficiency of gait and substantially increases energy cost. In contrast, an upper limb prosthesis that is slightly short will probably not present a noticeable asymmetry and will have little effect on bimanual activities. Endoskeletal prosthetic components facilitate lengthening and substitution of more sophisticated components.
Vigorous play causes considerable wear of the mechanical parts of prostheses. These parts are also vulnerable because of their small size and the sand, grass, and mud which children find inviting. Youngsters are likely to wear out prostheses from everyday use before circumferential growth necessitates a change. Signs of an outgrown socket include a tendency of the residual limb to slip out of the socket, pain or skin reddening caused by socket tightness, and a flesh roll around the margin of the socket. Socket liners are a convenient way to accommodate circumferential growth; as the child grows, liners can be removed. Alternatively, the prosthesis can be fitted with several layers of socks; the child eventually wears fewer socks to accommodate the added residual limb girth. Flexible sockets fitted to extra-thick frames are another way to accommodate growth. To fit the larger residual limb, a new flexible socket is made and material is ground from the frame.23
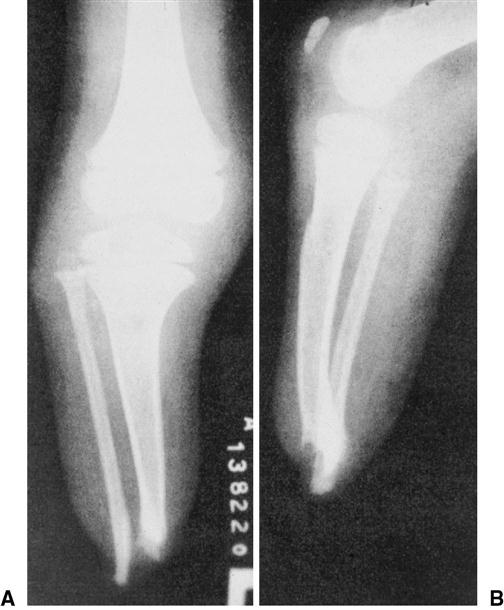
Prosthetic alignment should complement the immature skeleton and joint capsules. Children with surgical amputations through the bony diaphysis or metaphysis may have terminal bony overgrowth (Figure 29-2). As these children grow, terminal periosteal new bone may protrude beneath the terminal subcutaneous tissue and skin. Without treatment, a bursal sac forms and the skin becomes ecchymotic and hemorrhagic. The underlying bone then ruptures the bursal sac, and infection can occur.1 Overgrowth is a particular problem when the adolescent growth spurt begins. Customary treatment is excision of the periosteal sac, transection of the distal 2 to 3 cm of bone, and primary closure of the incision. Children may require this procedure several times during the growth period.24 Another approach is continuous skin traction, which can be used to maintain skin and soft-tissue coverage over the distal end of the residual limb until skeletal growth is complete. The difficulties of keeping distal force on the limb day and night usually preclude this method. Disarticulation preserves the distal epiphyseal plate and thus is not associated with overgrowth.
Near-normal range of joint motion is an important determinant of effective prosthetic use in children with limb deficiencies, as well as in adults with amputation. Active therapeutic exercise designed to increase joint excursion is preferable to passive stretching, especially in the presence of congenital contracture.2
Postoperative Care
Postoperative care is simpler for young children who undergo amputation than for adolescents and adults. Ordinarily the residual limb presents little or no edema and the wound heals rapidly. Phantom pain can occur and is associated with the extent of preoperative pain. Approximately one-fourth of those with congenital limb deficiency or amputation before the age of 6 years have phantom sensation, with far fewer reporting phantom pain.25 A pain diary may help older children and adolescents cope with phantom pain from traumatic amputation.
Psychosocial Factors in Habilitation and Rehabilitation
Habilitation amounts to more than selecting a suitable prosthesis and devising appropriate training. All children have personalities that develop along with their physical growth. Optimal emotional development occurs when parents and clinicians promote wholesome interactions. The essential message is that the child has a unique personality and that independence commensurate with age can be fostered.
Infants
Infants learn trust when their basic needs are met. The baby with limb anomaly has as much need for trusting, responsive care as does the infant with normal limbs. Infants respond to the anxieties of parents and others who interact with them. Successful habilitation depends on the parents’ replacing the expectation of a “perfect” infant with the reality of a baby who happens to have a limb deficiency. Birth of a baby with a limb deficiency can elicit intense emotion. Because such an event is rare in any hospital, medical staff may display shock and feelings of helplessness or revulsion. Some parents characterize the first few weeks after birth as a nightmare. They believe they are alone with a unique and hopeless problem when questions go unanswered or evaded. Reactions of the infant’s grandparents, siblings, and other family members influence habilitation. Mourning for the loss of the ideal child is part of the coping process.1
Newborns are too young for prosthetic fitting; nevertheless, early referral to a specialized clinic is highly desirable. The core team is composed of a pediatrician, physical therapist, occupational therapist, and prosthetist. The team should be able to draw on the expertise of psychologists, social workers, orthopedists, and engineers, depending on the needs of the child and family.2 Effective clinical team management involves the family in rehabilitation decisions and weighs management recommendations in light of the immediate impact on the child’s welfare and the long-term consequences on his or her appearance and function as an adult. An important resource is the Association of Children’s Prosthetic-Orthotic Clinics (6300 North River Road, Suite 727, Rosemont, IL 60018-4226; www.acpoc.org). The association, founded in 1958, has held an annual interdisciplinary conference since 1972.
The clinical team creates an atmosphere in which parents and their baby are welcome, encouraging conversation about feelings and obtaining answers to questions. The team’s approach aims to maximize the child’s function, while learning the parents’ style of dealing with unexpected events. Team members should empathize with parents’ grief, which can bear little relation to the extent of the infant’s disability.1 Some parents resist holding the baby, hide the deformity, avoid direct contact, or withdraw into silence. When clinicians hold the baby, parents usually realize that the infant really is lovable. Rather than denying any difference, the team fosters the attitude that, yes, they know the child is different, but they recognize and accept the baby for what the baby is and what the baby can do.
Families may be interested in seeing pictures or examples of the type of prosthesis that the child will probably use. Expectations regarding the extent of prosthetic restoration, however, may be unrealistic. Parents should understand what prosthetic and surgical possibilities exist so they can make rational decisions for their child. Infants usually receive the first prosthesis at approximately 6 to 9 months of age.2,25 Comparing the performance of children fitted with an upper-limb prosthesis before 1 year of age with those fitted later indicates no difference in satisfaction with the prosthesis nor functional use.26 Some parents find it difficult to accept the prosthesis, believing that it draws attention to the limb deficiency.
The team can also help parents of children who undergo amputation because of trauma or disease cope with feelings of guilt and shock. Team members assist the family in realizing that they were not negligent in protecting the child against injury or not recognizing symptoms of a disease process early enough to prevent amputation.
In addition to clinical team management, families benefit from participating in peer support groups in which they can share concerns, exchange information, and observe children of various ages playing with and without prostheses. Some groups publish newsletters that share information with those who live too far from the meeting site. The Amputee Coalition of America (900 East Hill Avenue, Suite 205, Knoxville, TN 37915; www.amputee-coalition.org) is a peer advocacy organization that produces a magazine, monographs, and videos; has annual conferences; operates the National Limb Loss Information Center; sponsors a youth camping program, national peer network, and limb-loss education and awareness program, among many other activities.
Parental acceptance of and active cooperation in the training program are the most important factors in its success and largely determine whether the child regards the prosthesis as a tool in daily activities.1 Families need to learn skin care, prosthetic operation, maintenance, and the capabilities and limitations of the prosthesis. Outpatient training is preferable to avoid homesickness, which can interfere with the child’s learning. In addition, the constant presence of one or both parents during therapy sessions enables the entire family to learn about prosthetic use and maintenance. Putting a prosthesis on an active child is a skill that takes time for parents to master. Scheduling appointments after naps and meals is generally more productive than attempting to coerce a tired and hungry child to participate in therapy. Clinicians should incorporate many brief activities in the treatment session, recognizing that infants have short attention spans. Therapists who treat infants need to interpret nonverbal indications of comfort or discomfort and satisfaction or dissatisfaction with the prosthesis. For example, the infant who coos, smiles, and engages in play is probably content with the prosthesis and the function it offers, whereas a cranky, crying child may be contending with an ill-fitting socket. As with all patients, the clinician must frequently examine the child’s skin, with particular attention to persistent redness, indicating high pressure, and irritation, which may signal dermatitis.
Toddlers
Toddlers must develop self-control to acquire the autonomy necessary to cope with their environment. The interval between 1 and 3 years of age is characterized by the development of language and functional communication, assertion of independence, and interpersonal control. Children as young as 3 years should be informed of any impending surgery, whether to revise a congenital anomaly or treat disease or injury. Doll play can help the child understand surgery and rehabilitation. Special dolls that depict amputations at various levels, with and without prostheses, are available.
Children must resolve feelings of deprivation and resentment that accompany the visible alteration of their bodies.1 Mobility, control, exploration, initiative, and creativity are prime emotional developmental milestones for older toddlers and young school-age children. Parents and professional staff should encourage the child’s independence. Facile use of a prosthesis can help children maximize their psychological potential. Children compare themselves with others and ask, “Where is my other hand (or leg)?” Children form two body images, one with and the other without the prosthesis. Parents should be able to give a simple and truthful answer, clearly stating that the child will not grow another hand, saying something like “you were born this way.”1 Similarly, children who undergo amputation need a realistic answer to the question, “What happened to you?” The child may engage parents in a power struggle regarding prosthetic wearing. A firm yet gentle approach with a range of acceptable choices usually enables the child to incorporate autonomy needs while gaining prosthetic proficiency.
The clinical team should value the parents’ comments about their child and involve the family in all aspects of care. The waiting room should have a variety of safe toys to make visits more pleasant. Parents should be present during the child’s examination and prosthetic fitting to increase communication and thereby reduce anxiety and maximize effectiveness of the prosthetic prescription and fitting process.
School-Age Children
School-age children need to become industrious and engaged in planning and executing tasks. The upper- or lower-limb prosthesis can be instrumental in fostering this important psychological task. The clinical team can help prepare the child and family for encounters with teachers, scout masters, clergy, and other adults.
In group experiences, the child may have to deal with feelings of social devaluation. The teacher or other group leader is in a position to bolster the child’s sense of self-worth. The first day at school or camp can be the occasion when the child displays the prosthesis and demonstrates its function. The presentation usually dispels the mystery of the appliance and shows that the prosthesis is simply a tool that makes it easier for its wearer to engage in certain activities. The teacher should be aware of the appearance of the residual limb, the child’s function with and without the prosthesis, any environmental or programmatic adaptations that the child may need, and how to cope with prosthetic malfunction. Anticipating awkward situations helps develop coping strategies. For example, in a circle game, classmates may be reluctant to hold hands with someone who wears an upper-limb prosthesis. If the teacher holds the child’s prosthetic hook, the other students are likely to realize that it is not scary or unacceptable to do so. School officials may be concerned about the ability of a child with a prosthetic leg to maneuver in the classroom and playground. Classmates’ natural curiosity should be dealt with through honest, simple answers. Although teasing is inevitable, the young child who feels secure understands that taunts are merely crude expressions of interest.
Among school-age children with limb deficiencies, demographic variables (such as age, sex, socioeconomic status, and degree of limb loss) are not significant predictors of self-esteem. In contrast, social support, family functioning, self-perception, and microstressors affect the child’s adaptation. Many school-age and older children respond favorably to scouting, camping, and other group recreational activities. Sports programs, such as skiing, horseback riding, and track events, are fun and give children with disabilities pride in athletic achievement.
Older Children and Adolescents
Adolescents face the critical step of developing a satisfying identity within themselves and with their peer groups. The teenager may select times when prosthetic wear is not desirable, for example, eschewing an upper limb prosthesis during a football game or discarding the leg prosthesis when swimming or playing beach volleyball. Adults should nurture young adults so they develop sufficient self-esteem to make satisfying decisions about when to use or remove the prosthesis. Teenagers with limb loss must cope with being visibly different. Young adults have to adapt to a culture designed for those who do not have a disability and must evaluate whether people relate to them as individuals or as people with handicaps. During adolescence, feelings such as “Why did this happen to me?” are often intensified. Adolescents constantly reexamine their body image; group showering after physical education class may be especially stressful for those with limb loss. Other developmental concerns in which limb loss plays a role are choosing a vocation, obtaining a driver’s license, and engaging in sexual activity. The clinical team needs to be sensitive to concerns about privacy, confidentiality, and independence.
Adolescents with bone cancer who undergo an amputation typically pass through a stage of initial impact when they learn that the treatment plan includes amputation. This news may be met with despair, discouragement, passive acceptance, or violent denial. Informing the adolescent of the rehabilitation process and the achievements of others can be helpful. The next stage is retreat, during which the adolescent experiences acute grief. Anger may be part of the coping process. The goal of grieving is relinquishing hope of retrieving the lost object. The staff can reinforce the patient’s strengths and encourage maximal independence. The third stage is acknowledgment, when the adolescent is willing to participate in rehabilitation and has incorporated the changed appearance into his or her body image. Reconstruction, the final stage, involves the return to developmentally appropriate activities, such as school, sports, and dating.
Rehabilitation and prosthetic decision making
Not all children with limb deficiency benefit from prostheses. With certain upper-limb anomalies, the remaining portion of the limb is more functional when bare than it would be if it were covered by a prosthesis.1,25 Some children who are born with bilateral arm absence generally use their feet to play and can do almost everything they need to without using complicated and heavy prostheses.25,27,28 In one large study, approximately half of the children with unilateral congenital deficiencies and two-thirds of those with amputation received prostheses. By the age of 12 years, two-thirds of those who had prostheses were still using them.29
Rehabilitation of Children with Upper-Limb Amputation
Because functional use of an upper-limb prosthesis often involves control of a terminal device (substitute for the missing hand), the prosthetic design and the rehabilitation program should be appropriate for the child’s level of motor, cognitive, and perceptual development.
Infants
Prosthetic fitting and training should complement an infant’s development. Although a prosthesis usually is not fitted until babies are at least 6 months of age, earlier developmental accomplishment paves the way for successful prosthetic use.
The average 2-month-old infant can hold objects with both hands. The baby who lacks one or both hands typically attempts to hug a stuffed animal with the forearms or upper arms, capitalizing on the tactile sensitivity of the skin. The normal 3-month-old can bring grasped objects to the mouth. Three months is also the age when babies attempt two-handed prehension, although this skill is not perfected until the child attains sitting balance at age 6 to 9 months.3
The 4-month-old infant props on the forearms, shifts weight to reach, and usually enjoys shaking noisy rattles by using rapid elbow flexion and extension. An important developmental step is reached at approximately the same age when the child can manipulate objects with one hand while the other hand stabilizes the toy. Simultaneous sitting and manipulating are still challenging at this age. Increased trunk strength enables the baby to reach unilaterally and bilaterally. Bilateral coordination at 4 months allows the infant to reach objects at the midline. Two-handed holding of a bottle typically occurs at approximately 4.5 months.22
By the fifth month, the infant can transfer toys from one hand to the other and is thus aware of the usefulness of holding objects. The infant’s dominant interest is in getting food; exploring surroundings; and making social contact with those who feed, hold, and provide care. Holding a large ball encourages the infant to clasp objects between the arms. Manipulating blocks or beads promotes stabilization of proximal body parts to allow fine movements with distal parts. Although a baby with intact limbs can get to the quadruped position and shift weight from side to side,22 the infant who is missing one or both arms will probably find that crawling is impossible and will have difficulty coming to a sitting position and pulling to a standing position.
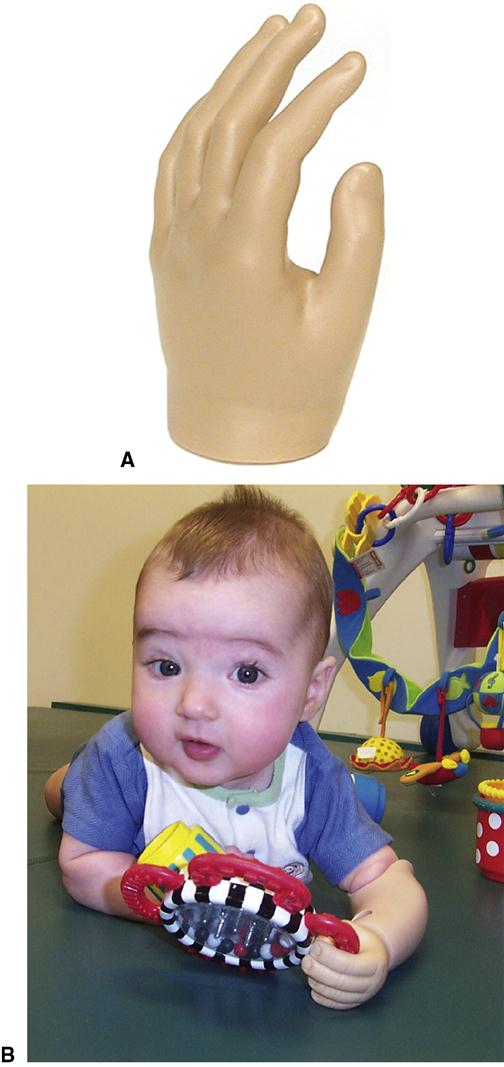
Six months is generally considered the optimal age for upper-limb prosthetic fitting (Figure 29-3).1 The baby with unilateral amputation has achieved good sitting balance, can free the sound hand for manual activities while sitting, and is actively engaged in exploring the environment. The prosthesis restores symmetrical limb length and enables the infant to hold stuffed animals and similar toys at the midline. The prosthesis also accustoms parents to the concept that a prosthesis will likely be a permanent part of their child’s wardrobe. Fitting can assuage parental guilt or shame regarding their infant’s abnormal appearance by replacing negative reactions with a constructive device that enhances the baby’s development. Many parents seek a prosthetic hand to disguise the limb anomaly. Early fitting provides experience that will be the basis for the young person’s later decision regarding whether to continue with prosthetic use. Fitting earlier to a rapidly growing infant makes the maintenance of socket fit difficult. In addition, a younger baby may find the prosthesis a hindrance during rolling maneuvers. Infants who are much older than 6 months may resist a prosthesis that deprives them of using the tactile sensation at the end of the residual limb. Initial fitting after 2 years tends to result in greater rejection of the prosthesis because by then the child has developed compensatory techniques.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree