Chapter 13 Rehabilitation and Prosthetic Restoration in Lower Limb Amputation
Despite advances in medicine, industry, and technology, amputation remains a leading source of disability. Approximately 159,000 lower limb amputations are performed each year,68 with peripheral vascular disease accounting for the vast majority of lower limb amputations. Amputations secondary to vascular conditions accounted for 82% of limb loss discharges, with the incidence increasing by 27% from 1988 to 1996.23 Trauma-related amputations accounted for 16% of amputations, whereas those resulting from malignancy and congenital deformity were responsible for 0.9% and 0.8% of amputations, respectively. Interestingly, the incidence of amputation secondary to a traumatic etiology has not gone up significantly within the United States Armed Services personnel despite recent conflicts.90 The incidence of amputations is not expected to subside anytime soon for a number of reasons, including the aging of the population and the increased incidence of diabetes in the United States. As the population ages, the number of amputations in persons older than 65 years is expected to double.36 Amputation prevalence is also expected to more than double from 2005 to 2050.106 Diabetes creates the greatest risk for amputation, surpassing the risks created by both smoking and hypertension. Diabetes is related to 67% of all amputations.81 The age-adjusted amputation rate for persons with diabetes is as high as 18 to 28 times more than that of persons without diabetes.94
In terms of level of amputation, Dillingham et al.23 reported that lower limb amputation accounted for 97% of all amputations between 1988 and 1996 with the following distributions: 31.5% toes, 10.5% midfoot, 0.8% ankle disarticulation, 27.6% transtibial, 0.4% knee disarticulation, 25.8% transfemoral, and 0.4% hip disarticulation. Other sources report that 64% to 73% of amputations were transtibial; 26% to 31%, transfemoral level; and 4.5%, knee disarticulation.4,35 Patients with diabetes are at greater risk for a second amputation, with rates as high as 18% at 2 years and 45% at 4 years.26 A second amputation is shown by more recent studies to be a conversion to a more proximal amputation level in 9%, with amputation of the contralateral limb in 11% to 21% of patients with amputation.4,35,49,91 In patients with vascular disease, 34% required more than one amputation procedure.80
Survival rates after amputation vary based on a variety of factors. Those who have amputations from trauma tend to have good long-term survival, but those who have amputations because of a vascular etiology face sobering survival statistics. After a vascular amputation, the 30-day mortality rate ranges from 9% to 21%,1,4,28,49,80 and long-term survival has recently been found to be 48% to 69% at 1 year, 42% at 3 years, and 35% to 45% at 5 years.4,15,28,79,80 More proximal levels of amputation have also been associated with decreased survival rates.4,15,36,79 Diabetes and end-stage renal disease have been shown to negatively affect survival, with 5-year survival rates as low as 30.9% and 14.4%, respectively.4
The chances of prosthetic fitting vary depending on the etiology of amputation, the level of amputation, and the age. In a survey of individuals registered with the Amputee Coalition of America, 95% of respondents had a prosthesis and used it extensively.70 MacKenzie et al.58 found that 97% of all traumatic amputees were ambulating with a prosthesis at 3 months. Success rates are lower for people with amputations resulting from vascular disease and diabetes. Overall success rates for prosthetic fitting in dysvascular patients have been reported to be greater than 80%.40,72 Fletcher et al.36 reported a 78% success rate in transtibial patients and a 57% success rate in transfemoral patients for functional prosthetic use among people older than 65 years who were referred to an amputee clinic. He noted that success of fitting diminished with age and level of amputation. Patients with transtibial amputation older than 85 years had less than a 2% chance of successful prosthetic fitting. Johannesson et al.49 reported that 43% of all patients received a prosthesis after primary amputation. Multiple limb amputees can be successful ambulators. Two studies have reported that 70% of bilateral transtibial amputees were able to use their prosthesis for ambulation.13,93
Regardless of its etiology, amputation remains a source of significant physical and psychological trauma in individuals facing limb loss. Although many patients and physicians alike might consider it to be a failure of medical and surgical management, amputation is a reconstructive surgery that maximizes the patient’s function and quality of life. Most patients have the potential for a successful outcome after amputation. Although elderly patients who have undergone vascular amputation might never run or participate in competitive sports, they can still have the potential for improved function with a prosthesis. For the young person with amputation, an active lifestyle with a prosthesis is expected. To illustrate the functional potential of a patient with amputation, the men’s record for the 100-m sprint for an athlete with an amputation is 10.91 seconds. This was set in April 2007 by Oscar Pistorious, a man with bilateral transtibial amputations, who later petitioned to qualify for the 2008 Olympics.57 Although he did not compete, that is not far behind the able-bodied record of 9.69 seconds set by Usain Bolt at the 2008 Olympics.107
Presurgical Management
Selection of Amputation Level
The earliest attempts to judge the appropriate level of amputation focused on the presence of palpable pulses, angiographic findings, skin color and temperature, character and location of pain, and most notably, the presence of incisional skin bleeding at the time of surgery. Various diagnostic methods exist to help determine the level at which healing will occur. These include Doppler pressure measurements, pulse volume recordings, photoplethysmographic pressures, laser Doppler blood flow studies, xenon-133 skin blood flow studies, arterial angiography, and transcutaneous oxygen determinations (see Chapter 57). However, these tests have not been more consistently reliable than clinical judgment in predicting wound healing at a given level.5,25 Most surgeons use a combination of objective data and assessment of the appearance of the tissues at the time of surgery, particularly bleeding, to decide on the site of amputation.
Pain Control
Good perioperative pain control is essential for the patient facing limb loss. Beyond patient comfort, adequate pain control minimizes the patient’s stress, and allows the patient to participate more fully in a rehabilitation program. Uncontrolled pain can result in the development of central nervous system–mediated pain and chronic pain,60 as well as impair postoperative healing and immune functions.8,22
The mainstay of perioperative pain control treatment is opioid therapy. Oral opiates are usually sufficient, but there should be no hesitation to use more aggressive pain control measures including transdermal, subcutaneous, intramuscular, or intravenous routes. A scheduled dose of a long-acting agent in conjunction with an immediate-release analgesic is recommended so that the patient has consistent pain relief. A sufficient dose of analgesia just before therapies often helps the patient fully participate. Caution, however, should be used in the geriatric population given the risk of delirium in these individuals, and opiate use should be streamlined in these instances.
Patient-controlled analgesia systems are useful for patients having severe pain in the perioperative period. They provide a continuous infusion of analgesic, with the ability of the patient to use a supplemental dose as needed. Patient-controlled analgesia provides excellent analgesia and can reduce some of the patient’s stress or fear related to pain. Continuous regional nerve blocks and epidural anesthesia can also be used for perioperative pain control,58 although typically these cannot be continued in the post–acute care setting.
Psychological Support
Psychological assessment and support for the patient facing limb loss should be a high priority. Assessment of the patient’s expectations and goals is important. Frequently, patients fear that they will never be able to walk again after amputation and might not expect to be able to accomplish more demanding occupational or recreational tasks. These perceptions are often unfounded because most amputees can do very well functionally. As noted above, several studies indicate that greater than 80% of amputees at all levels will be able to successfully walk with a prosthesis,40,63,72 and this is consistent with our experience. Each patient’s specific long-term goals should be identified before surgery, and a comprehensive rehabilitation program should be outlined to achieve these goals. Patients feel empowered and reassured when higher functions (such as sports) are recognized as legitimate goals, and the rehabilitation team helps them achieve these goals.
Describing the rehabilitation process in detail to patients and educating them about prostheses can help to allay their fear of the unknown. Providing educational literature and website addresses can be a valuable and calming service to patients and their families (Box 13-1). Some programs use a peer counseling program in which patients who are successful prosthesis users visit patients with new amputees on request. Finally, it is important to discuss phantom limb sensation and phantom limb pain with patients before surgery. Phantom limb sensation is the temporary nonpainful feeling that the amputated limb is still present. This feeling typically fades away over a period of weeks. Phantom pain is the usually temporary pain that can occur in a limb after its amputation, especially in a patient with a long history of preamputation limb pain. All patients need to be told to expect these sensations in the missing limb after surgery and to realize that they are normal.
BOX 13-1 Educational Resources Available for Amputees
Booklets
Books
Websites
Postsurgical Management
Wound Care
In patients with vascular compromise, wound margin necrosis can develop. The limb should be monitored closely in these cases, kept clean, and protected from any trauma that could cause a dehiscence in such a fragile wound. Once the nonviable tissue is clearly demarcated, debridement can be considered. Adjuvant therapies such as negative pressure wound therapy and hyperbaric oxygen treatment are available options that have possible benefit but warrant further investigation to determine their efficacy with this population.43,91,98
Good nutrition must be encouraged and supported with supplements when necessary. Eneroth30 found that when supplementary nutrition was given to malnourished patients, twice as many adequately nourished patients healed their residual limb wound when compared with controls.
Edema Control
Several different edema control systems are available. The most commonly used treatment is elastic wraps on the residual limb (e.g., Ace bandages). Although elastic wraps can provide effective compression, they are high-maintenance items that must be properly applied and changed about every 4 to 6 hours to maintain consistent compression.61 This can be difficult and time-consuming for a patient, or even the health care team, to accomplish. Elastic wraps that are improperly applied or displaced in the normal course of regular movement can turn into tourniquets, causing pressure wounds and even limb ischemia. Consequently the use of elastic wrapping is not recommended.
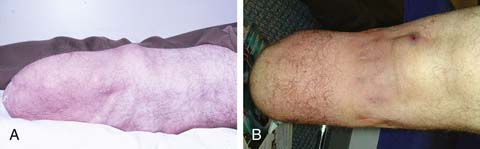
The use of elastic socks or elastic stockinette provides a better alternative than elastic wraps. Elastic stockinette (e.g., Compressigrip and Tubigrip) can be applied in multiple layers to give graded and increasing compression toward the end of the residual limb (Figure 13-1). It is inexpensive and easily applied. Premanufactured residual limb shrinkers can also be used. For transfemoral amputees, a residual limb shrinker with a waist belt must be used, because otherwise the dressing tends to slide off the conical-shaped residual limb. The waist belt should be attached to the elastic dressing at the side of the limb. If the attachment is worn in front, the shrinker will slide off during sitting.
Prosthetic elastomeric liners can also be used as compression socks for edema reduction in amputees.49,51 They can provide compression and also lend some degree of protection to the residual limb. Because of their suction fit, they can be used on the transfemoral amputee without a waist belt. When using any elastic dressing, bony prominences should be closely monitored because pressure can concentrate at protruding bony areas and lead to skin breakdown.
Rigid dressings provide additional benefits over soft dressings alone for transtibial amputees (Figure 13-2). Rigid dressings help protect the residual limb from any inadvertent trauma, such as a fall.31 They provide good compression to minimize edema, and the cast can be conformed to minimize pressure over bony prominences. Partial weight-bearing can also be started through the rigid dressing to help desensitize the limb and build tolerance to pressure.

FIGURE 13-2 Rigid dressings for transtibial amputee. (A) Rigid dressing. (B) Rigid removable dressing.
A nonremovable rigid dressing is a cast that is applied over the fully extended residual limb up to the midthigh (see Figure 13-2, A). This type of cast is helpful in preventing knee flexion contractures and can be used as an immediate postoperative prostheses (as discussed below). A nonremovable cast does not allow for wound inspection except at cast changes. It also does not allow patients to massage their residual limbs, an important part of the desensitization program.
A removable rigid dressing (RRD)104,105 is a custom-made cast that covers the residual limb up to the knee (see Figure 13-2, B). It is held in place with either elastic stockinette or a thigh cuff. As the limb shrinks, socks, shrinker socks, and elastic stockinette are added underneath the RRD to keep it snug. The RRD allows for frequent wound inspection and massage of the residual limb. It also helps to teach patients how to adjust sock ply, a necessary skill for using most types of prostheses. A suggested protocol is to start with a rigid nonremovable dressing applied immediately after surgery. After the first 3 to 6 days, the cast should be changed to an RRD, which should be used until most of the edema is resolved and the wound is well healed. If more than 12 to 18 ply of sock is required to keep the RRD snug, a new RRD is recommended.
Functional Rehabilitation
Patients should be educated in proper positioning. Prevention of hip and knee contractures is critical in this period. Patients should not have pillows placed under the knee because this can lead to knee flexion contracture. To prevent hip abduction contractures, pillows should not be placed between the legs. Dangling the residual limb over the side of the bed or wheelchair should be avoided. A knee extension board (Figure 13-3) can be fitted underneath the wheelchair or chair to promote knee extension and help prevent dependent edema. Wheelchair-elevating leg rests are generally less effective and more expensive than these boards. If knee flexion contractures are of great concern, a knee immobilizer while the patient is in bed can be used to maintain knee extension. Patients should be instructed to lie prone several times a day for 10 to 15 minutes at a time to prevent hip flexion contractures. Individuals who cannot tolerate prone positioning can lie supine on a mat while performing hip extension exercises of their affected limb.
ROM and strengthening exercises of the affected limb are important adjuncts to positioning. Muscles that oppose the common sites of contracture must be strengthened, especially knee and hip extensors. Other important muscles groups that should be strengthened include the hip adductors and abductors. Because patients are increasingly reliant on their arms to assist with mobility, arm strengthening and conditioning are needed. Specific exercises include strengthening of the wrist, elbow extensors, and scapular stabilizers. This training prepares patients to properly execute transfers and to correctly use crutches or a walker. Initiation of aerobic exercise is needed to increase endurance and cardiovascular fitness, but given the high incidence of concomitant cardiovascular disease in individuals with a vascular etiology of amputation, adherence to cardiac precautions is important.
Early partial weight-bearing can begin in the first few days if there are no wound complications. For transtibial amputees with rigid dressings, limited weight-bearing can be performed through their cast using a strap across their wheelchair (Figure 13-4). When the patient is up in the parallel bars, weight-bearing can be done via a tire jack or adjustable footstool. Immediate postoperative prostheses can also be used for early weight-bearing as described below. Inspection after weight-bearing is important in monitoring wound tolerance of pressure. This is especially important in individuals with amputation from vascular disease or patients with impaired sensation.
Pain Management
Identifying the etiology of postoperative limb pain is important for successful control of the pain. Because of nerve fiber damage and ongoing stimulation of the nerves in the residual limb, a generalized residual limb pain is initially expected secondary to the surgical incision and postoperative edema. Ectopic activity at the cut end of nerves is expected and can be due to unstable sodium channels or the uncovering of new pathologic receptors.6,7 Ephaptic transmission, which is the stimulation of afferent fibers (nociceptors) by efferent neurons (motor or sympathetic), can also contribute to limb pain.48,77 This acute pain responds well to intravenous or intramuscular opiates. It subsides fairly rapidly, and the parenteral opiates can usually be discontinued within 2 to 3 days. Scheduled doses of oral opiates with rescue medications as needed should be continued beyond this period and weaned slowly so that the patient continues to receive adequate pain control.
Desensitization techniques should be added to the treatment plan within a few days of surgery. Patients should be instructed to start massaging and tapping their residual limb, which can be performed through any soft dressing. This gentle stimulation can help to reduce residual limb pain by closing the pain gate,60 and gives patients a technique for controlling their pain independently. Self-massage also forces patients to attend to their amputation; this can help with their new body image and psychological adjustment to limb loss.
Even after the immediate postoperative period and residual limb healing, the incidence of pain is high in patients with amputation, with 68% reporting residual limb pain and 80% reporting phantom pain.32 The most common types of sensory problems reported include phantom pain, phantom sensation, and residual limb pain. The differential diagnoses for pain in an amputated lower limb are diverse, and treatment options differ significantly based on the etiology of pain. Consequently the source and mechanism of the pain must be investigated and identified so that an optimal treatment plan can be implemented.
Prosthesis use is a common cause of residual limb pain in individuals with amputation. In these instances, pain tends to be worse with prosthetic use and during ambulation. Usually there is skin irritation that correlates with the area of the prosthesis causing the pain. Multiple factors can contribute to prosthetic pain including socket fit, suspension, alignment, and gait pathology. Consideration must be given to all of these areas when there are complaints of pain in the residual limb during prosthetic use. As an example, Table 13-1 lists some of the common causes of distal tibial pain, a very common site for prosthesis-related pain in transtibial amputees. Addressing the prosthetic etiology typically results in pain reduction.
Table 13-1 Prosthetic Adjustments for Distal Tibial Pain in the Transtibial Amputee
| Contributing factors | Treatment |
|---|---|
| Excessive socket pressure | Socket relief. Remove sock ply. |
| Pistoning in the socket | Add socks to tighten fit. Build up the liner. Tighten socket. Tighten suspension system. |
| Excessive pressure from liner | Change suspension system. |
| Excessive early knee flexion | Move foot forward. Plantar flex foot. Decrease socket flexion. Soften heel of foot or shoe. Add anteroposterior ankle motion. Round heel of shoe or change shoe. Strengthen quadriceps/hamstring muscles. |
Phantom limb sensation and pain are likely maintained by afferent, central, and efferent (sympathetic) dysfunction.54 Phantom limb sensation and pain are neuropathic perceptions in a portion of the limb that was amputated. Most amputees experience some degree of phantom limb sensation and pain, but the natural history is for these feelings to diminish both in frequency and intensity over the first few weeks to months after the amputation.29 These sensations are highly variable in character. Phantom limb sensations are frequently described as numbness, tingling, pins and needles, or itching. Some amputees report the sensation of the phantom limb becoming shorter, known as telescoping. Patients can also complain that the missing limb feels like it is moving or is in a cramped or awkward position. It is important to explain that these are normal sensations that will likely diminish with time. Sometimes patients do not consider the sensation to be painful, but uncomfortable or “bothersome.” These sensations can be severe enough to interfere with sleep, impair patients’ functioning, or significantly reduce their quality of life. At this point the phantom limb sensation should be treated as neuropathic pain. The character of phantom limb pain is often described as sharp, burning, stabbing, tingling, shooting, electric, or cramping. Patients frequently perceive the same type of pain that they had before the amputation. For example, they might feel like they still have a painful foot ulcer.
Residual limb pain, previously referred to as stump pain, is another manifestation of central sensitization. Preliminary work in the area suggests that it is a form of allodynia (i.e., pain evoked by previously innocuous stimuli) or a spontaneous pain of peripheral neuropathic origin, central neuropathic origin, or both. Spontaneous residual limb pain is usually described as aching, burning, or throbbing, whereas evoked pain can be electrical or shooting (which can easily be confused with a clinically significant neuroma).95 The pain is localized in the residual limb and can be associated with phantom limb pain. Edhe et al.29 reported residual limb pain to be as common as phantom limb pain in lower limb amputees, and often more distressing.
The first line of treatment for bothersome phantom limb sensation, phantom limb pain, and residual limb pain is desensitization techniques. Massaging, tapping, slapping, wrapping, and friction rubbing of the residual limb often diminish such sensations. Patients frequently find that their phantom limb pain diminishes with the stimulation of using a prosthesis. Anecdotally, many patients find that for a phantom itch, scratching the remaining leg in the same spot is helpful. For cramped or malpositioned limb sensations, hypnosis can be helpful.27,65,88 Under hypnosis, the patient might be able to alleviate a cramped phantom hand or move an awkwardly phantom positioned limb to a more comfortable position.
If desensitization techniques are insufficient and these pains are significantly interfering with quality of life, pharmacologic treatment should be considered. Unfortunately, the literature is not robust with regards to demonstrating efficacy of any particular agent in treating phantom pain.69 However, the two primary categories of medicines generally used in clinical practice to treat chronic phantom limb phenomenon are antidepressants and anticonvulsants. Antidepressants have several advantages in addition to pain control. They can also treat depression, which is a common problem in new amputees. They generally have anxiolytic effects and, some being sedative, can improve sleep. They are convenient because they are usually taken just once per day, and they are generally less expensive than the newer antiseizure medications. Analgesic antidepressants apparently need to have both noradrenergic and serotonergic receptor activity to effectively treat neuropathic pain,33 which explains why the selective serotonin reuptake inhibitors do not help with the treatment of phantom limb pain. Tricyclic antidepressants have the most anecdotal and empirical support for treating pain, but they also have undesirable anticholinergic side effects.52,82 Some antidepressants have both serotonergic and noradrenergic activity without the anticholinergic activity (serotonin and norepinephrine reuptake inhibitors [SNRIs]), and might help in treating neuropathic pain. Mirtazapine is an SNRI that can be useful for the treatment of phantom limb pain because it has no anticholinergic side effects, and it enhances sleep (night is often when phantom limb pain is most problematic). It is an effective antidepressant and an anxiolytic, although weight gain can be a significant side effect.85 Venlafaxine and the newer agent duloxetine are also SNRI-type agents that might have some value for the treatment of neuropathic pain.
A number of anticonvulsants have been used to treat neuropathic pain syndromes.6 At present, gabapentin is probably the most widely prescribed neuropathic pain medicine in the United States. Despite its name, gabapentin’s mechanism of action is unknown. Nevertheless, gabapentin has demonstrated efficacy with neuropathic pain, has minimal side effects, and has been shown in a small study to have efficacy in phantom pain.10,45 However, it usually requires frequent dosing (generally three to four times a day). Traditional anticonvulsants such as carbamazepine and phenytoin are membrane stabilizing agents (sodium channel blockers) that have the widest historical use for the treatment of neuropathic pain syndromes.21,69 However, they have a high incidence of significant side effects. Other anticonvulsants that are being used to treat neuropathic pain include oxcarbazepine, topiramate, levetiracetam, and pregabalin, but few or no data exist yet concerning their efficacy. Anticonvulsants can also be used in combination with antidepressants or with each other to maximize relief from phantom limb pain. This must be done in a thoughtful fashion that uses complementary mechanisms.
Some success has been reported with topical anesthetic agents such as various analgesic balms, sprays, and patches. Capsaicin, a substance P inhibitor, has been anecdotally reported to be effective for phantom limb pain and residual limb pain.51 Lidocaine cream, ointment, and patches have also been used with some success.
Other nonpharmacologic modalities exist for the treatment of phantom limb pain such as stress-relaxation techniques and biofeedback.37,50,87,88 Transcutaneous electrical nerve stimulation has also been shown to give temporary pain relief.35,56 Mirror therapy, while primarily used with upper limb amputations, has been attempted in patients with lower limb loss,16,19 with some success.
Neuromas are bundles of nerve endings that form after a nerve is cut, as is done during an amputation. They can produce sharp, focal pain under pressure or upon palpation (i.e., Tinel’s sign).22 If a neuroma is superficial, then a small, tender mass can be palpated. It can cause significant pain and can preclude use of a prosthesis. Initially, prosthetic socket adjustments are used to relieve pressure over a neuroma. If this is unsuccessful, neuropathic pain medication, intralesional steroid and anesthetic injection, or neuroma ablation with phenol, alcohol or cryoablation can provide pain relief. However, literature demonstrating efficacy in patients with amputation remains severely limited. Ultrasound-guided phenol instillation has been shown in a small case series to provide some benefit in the treatment of neuroma pain.44 Radiofrequency ablation has also had some success in case reports for both neuroma and phantom limb–related pain.76,103
If these interventions are all ineffective, the neuroma can be surgically excised and the nerve endings buried deep in the soft tissue to protect them from mechanical pressures. Surgical resection has been found to be up to 80% successful.12,42
While the causal relationship between amputation and phantom limb pain or residual limb pain is obvious, other conditions can also cause pain in a phantom limb. In trauma, referred pain can be generated down the leg by a proximal nerve injury, plexopathy, radiculopathy, or occult fractures, even if the leg has been amputated. Referred leg pain from spinal stenosis or arthritis at the knee or hip can also be mistaken for phantom limb pain. These alternative diagnoses must be considered and clearly require different treatment plans.
Psychological Adjustment
The emotional impact of limb loss is devastating and is frequently underestimated by the rehabilitation team. Grieving over the loss of one’s limb is necessary, and a brief exogenous (reactive) depression is expected. Amputees are at high risk of developing more severe psychological problems. The incidence of persistent clinical depression is estimated to be 21% to 35% for people with limb loss.20,83 Risk factors for depression include low income, comorbid conditions, and the presence of phantom and back pain.20 Posttraumatic stress disorder is a recognized complication after traumatic amputation, but frequently goes untreated. Nontraumatic amputees can also develop anxiety disorders from the stress related to limb loss.
Peer counseling and amputee support groups are another important emotional support mechanism. The opportunity to talk to persons who have been through a similar amputation, and to see how well they are doing, can be very valuable to the patient. The Amputee Coalition of America (see Box 13-1) has a national peer network that provides peer counselor training sessions and lists amputee support groups by region.
The physician should regularly monitor the patient’s emotional adjustment to amputation by assessing mood, appetite, weight changes, quality of sleep, and the occurrence of nightmares. Any correlation between the patient’s perceived stress level and pain should be explored. Sometimes adjustment issues will not become problematic until shock and denial wear off and time passes. Because studies have shown that the incidence of depression in younger amputees increases with time,38 continued monitoring by the rehabilitation team is necessary. The whole team must be involved in monitoring the patient’s emotional state, and not just the physician. In most cases the therapists and prosthetists will spend much more time with the patient and might have better insight regarding a patient’s emotional status.
Skin Problems
Problems with skin are frequent in patients with amputation. It has been reported that 63% of patients experienced a skin problem in the past month in one questionnaire.61 Adequate treatment requires proper identification of etiology and type of skin issue.
Verrucose Hyperplasia
Verrucose hyperplasia (also termed verrucous hyperplasia) is the development of a wart-like lesion on the end of the residual limb (Figure 13-5). Cracks in the skin and even infection can occur in severe cases. Verrucose hyperplasia is most common in the transtibial amputee, but can occur with other levels of amputation. This dysplastic skin condition is thought to be due to choking effect on the residual limb. It is hypothesized that if the prosthesis fits tightly around the limb (circumferentially) and there is a lack of distal pressure, then vascular congestion can occur that somehow leads to verrucose hyperplasia. The pathophysiology of the condition remains unknown. Adjusting the prosthesis to create adequate distal pressure usually resolves the verrucose hyperplasia within a few weeks or months. Adjustments such as simply adding an end pad to the socket can be sufficient; otherwise a new total contact socket is recommended.
Contact Dermatitis
Contact dermatitis is inflammation of the skin manifested by erythema and sometimes mild edema. It can be caused by an irritant that causes scaling, or an allergic reaction that induces vesiculation. Contact dermatitis is a common problem with prostheses, especially with the increased use of elastomeric liners. It is treated by locating the causative agent and preventing it from contacting the residual limb. Hygiene of the residual limb and its prosthetic components must be considered first, because poor hygiene can allow the accumulation of allergens on the residual limb. Soaps can also be the causative agent, and the patient should wash the residual limb each night with a mild or hypoallergenic soap and then rinse the limb well. Similarly the skin interface system (e.g., socks, liners, or the socket itself) should be washed daily per the manufacturer’s recommendations, rinsed well, and allowed to dry before donning. If these simple measures fail, then a change in the skin interface system is needed. Wool socks can be changed to cotton or acrylic. Elastomeric liners made of different materials can be tried. If the contact dermatitis persists, then a change to a different interface system must be considered. For acute contact dermatitis, a short course of topical steroids can decrease inflammation and discomfort. Because the use of topical steroids cannot be considered a long-term plan, the causative agent must be identified and eliminated.
Hyperhidrosis
Hyperhidrosis has been reported to be one of the most common skin issues in patients with amputation, with 32% to 50% of patients reporting this as a symptom in one large study.59 It is usually associated with prosthetic use and can be seen with all types of suspension and liner materials, because heat dissipation is impaired with the use of a prosthetic device or material over the residual limb. Hyperhidrosis can be alleviated by using nylon sheaths as an interface with the liner material, and by using topical or spray antiperspirants. One case series showed promise with the use of botulinum toxin for alleviating this symptom.17
Infections
Once the residual limb is healed, other infections can arise. Aeration of the residual limb, good limb hygiene, good prosthetic hygiene, and proper prosthetic fitting can all prevent and treat such infections. Residual limbs tend to harbor more abundant bacterial flora than unaffected limbs.3 Folliculitis is a hair root infection that can occur in limbs with excessive perspiration and oily skin. This is aggravated by sweating and is worse in warmer, humid months. Skin maceration and moisture can allow bacterial invasion of the hair follicles. This can eventually lead to cellulitis.51 Treatment consists of warm compresses and topical antimicrobials. More severe cases warrant the use of oral or parenteral antibiotics, and incision and drainage of boils.
Epidermoid Cysts
Epidermoid cysts occur when sebaceous glands are plugged. These cysts are firm, round, mobile, subcutaneous nodules of variable size that are most commonly found in the popliteal fossa of transtibial amputees and the upper thigh of transfemoral amputees (Figure 13-6). They can be quite tender and can become inflamed by the pressure of the prosthesis. Sometimes bleeding into the cyst makes them appear dark. Ruptured epidermoid cysts have a purulent or serosanguineous discharge. Treatment with topical or oral antifungal and/or antibacterial agents has been recommended.52 Treatment should also include minimizing pressure over the cysts by adjusting the prosthesis and ensuring an optimal fit. Sometimes larger inflamed cysts require incision and drainage. However, recurrences are frequent because incision and draining does not remove the keratin-producing lining of the cyst. A more definitive treatment consists of surgical excision, but even this intervention cannot completely eliminate the possibility of recurrence.
Other Complications
Joint contractures are frequent complications during the rehabilitation of people with limb loss. Initial treatment consists of a stretching program both in therapy and at home. For knee contractures, extension devices like knee immobilizers can provide relief. For hip flexion contractures, prone lying on a daily basis is helpful. Ultrasound heating can also be an effective therapy when combined with aggressive stretching, provided the patient’s vasculature is adequate for vigorous heating. For transtibial patients who are expected to ambulate, the knee flexion contracture is initially accommodated in the prosthetic alignment. Once the patient is ambulating adequately, flexion is gradually taken out of the socket. This causes an extension stretch when the patient walks, and progressively reduces the contracture. In severe cases that do not respond to the above treatment, surgical release can be considered.
Bony growths at the end of the amputated bone are called bone spurs. They occur frequently and are usually asymptomatic. Similarly, heterotopic ossification (HO) is a spontaneous development of bone in soft tissue, usually occurring after traumatic amputations. The incidence of HO with traumatic amputation has been reported to be as high as 63% in recent armed conflicts.73 If a bone spur or HO protrudes distally and is not covered by adequate soft tissue, it can become painful and cause skin breakdown. Accommodating the spur or HO with a relief and/or padding in the socket might solve the problem. If this fails, surgical excision might be required.
Prostheses
Timing of Prosthetic Fitting
Determining when to fit the lower limb amputee with a prosthesis and what kind of prosthesis to use are issues open to considerable debate. One option for transtibial amputees is to use an immediate postoperative prosthesis (IPOP). IPOPs traditionally have been thigh-high casts with a pylon and foot attached (Figure 13-7, A). Prefabricated devices are also now available (Figure 13-7, B and C). These devices allow for earlier bipedal ambulation. Although many claims have been made for the advantages of IPOPs over soft dressing management (including improved psychological acceptance, reduction in pain, accelerated rehabilitation times, reduced revision rates, and time to healing), these claims have rarely been evaluated with controlled studies.89 A review of 10 controlled studies yielded only two proven claims for the IPOP: (1) that rigid plaster casts result in accelerated rehabilitation times and significantly less edema compared with soft dressings; and (2) that prefabricated pneumatic prostheses were found to have significantly fewer postsurgical complications and fewer higher level revisions compared with soft gauze dressings. Only limited weight-bearing can take place with an IPOP, and patient compliance is important for such success.89 Although weight-bearing is limited through IPOPs, patients clearly have greater stability in standing and walking with the bipedal support. Some studies have shown an increase in wound dehiscence and infection with these devices.18 Frequently the residual limb is too tender and painful to allow early weight-bearing to take full advantage of these devices. With the nonremovable IPOPs, patients are unable to inspect or massage their residual limbs, which can interfere with desensitization and emotional adjustment to their amputation.
The most conservative option is to wait until the wound on the residual limb is completely healed and surgical edema has resolved before the patient is fitted with a custom prosthesis. This generally takes 3 to 6 months with dysvascular amputees. Although this approach can minimize wound problems related to early weight-bearing, there is a higher risk of complications such as joint contracture, deconditioning, pressure ulcers, and an unnecessarily long delay in returning to functional ambulation.
Factors Affecting Prosthetic Prescription
In 1994 the federal government attempted to clarify which knee, ankle, and foot components should be used for patients with particular functional abilities or functional levels. The functional level is a measurement of the capacity and potential of the patient to accomplish his/her expected postrehabilitation, daily function. This functional classification was designed to assist the Durable Medical Equipment Regional Committees in determining appropriate reimbursement for prosthetic components.24 It limits patients with lower functional abilities to simpler prosthetic components, while allowing more active people to use more advanced (and expensive) devices. The determination of these levels is for individuals with unilateral lower limb amputations and is at the discretion of the prescribing physician. Items to take into consideration are the patient’s medical history, present medical condition, and functional status, as well as future ambulation goals and expectations. The prescribing physician should keep an open mind regarding the potential or expected functional level, focusing on the patient’s current condition and how it may affect the goals. Documentation of function should be maintained in the patient’s records.
The functional levels (often referred to as the K-modifiers) are listed in Box 13-2. These levels are based on the patient’s potential, not on the current level of function; even deconditioned patients can reach a higher level of function than anticipated with appropriate rehabilitation. Also, the K1 level includes the use of a prosthesis for assisting with transfers. Many low-functioning people with amputations below the knee or lower benefit from the use of a prosthesis. For higher levels of amputation, a prosthesis does not generally assist with transferring; instead, it often gets in the way.
BOX 13-2 Description of the K-Level Modifiers
| K0 | Does not have the ability or potential to ambulate or transfer safely with or without assistance, and a prosthesis does not enhance quality of life or mobility. |
| K1 | Has the ability or potential to use a prosthesis for transfers or ambulation on level surfaces at fixed cadence. Typical of the limited and unlimited household ambulator. |
| K2 | Has the ability or potential for ambulation with low-level environmental barriers such as curbs, stairs, and uneven surfaces. Typical of the limited community ambulator. |
| K3 | Has the ability or potential for ambulation with variable cadence. Typical of the community ambulator who can traverse most environmental barriers and has vocational, therapeutic, or exercise activity that demands prosthetic utilization beyond simple locomotion. |
| K4 | Has the ability or potential for prosthetic ambulation that exceeds basic ambulation skills, exhibiting high impact, stress, or energy levels. Typical of the prosthetic demands of the child, active adult, or athlete. |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree