CHAPTER 28 Rehabilitation after posterior instability repair—open vs. arthroscopic
 Progression of rehabilitation exercises should follow soft tissue healing guidelines to avoid recurrence of shoulder pain and instability.
Progression of rehabilitation exercises should follow soft tissue healing guidelines to avoid recurrence of shoulder pain and instability. Range of motion progression and strengthening exercises following open reconstruction is delayed in comparison with the arthroscopic technique during the first 6 to 8 weeks of rehabilitation.
Range of motion progression and strengthening exercises following open reconstruction is delayed in comparison with the arthroscopic technique during the first 6 to 8 weeks of rehabilitation. Progression of strengthening exercises should begin with isometric exercises advancing to dynamic resistance and closed kinetic chain exercises.
Progression of strengthening exercises should begin with isometric exercises advancing to dynamic resistance and closed kinetic chain exercises. Optimization of shoulder function should incorporate a variety of dynamic and static exercises along with consideration of the patient specific demands required by their sport or occupation.
Optimization of shoulder function should incorporate a variety of dynamic and static exercises along with consideration of the patient specific demands required by their sport or occupation.Introduction
Posterior glenohumeral joint (GHJ) pathology is increasingly recognized as a source of activity related posterior GHJ pain and instability. While falls and motor vehicle accidents are common causes of traumatic posterior instability, participation in football, tennis, throwing sports, swimming, weight lifting, wrestling, and volleyball have been shown to contribute to the development of posterior instability.1,2 Conservative treatment focusing on scapular and rotator cuff musculature is widely advocated. Patients unable to return to their preinjury level of performance following 6 months of comprehensive rehabilitation will often require surgical intervention.
Early reports suggested a low incidence (<5%) of posterior GHJ instability but improved evaluation techniques (arthroscopic, clinical, and imaging) and awareness of this entity now suggests that incidence approaches 10% of GHJ instability cases.3 The etiology of posterior GHJ instability may include acute macrotraumatic injury (dislocation), recurrent microtraumatic injury (subluxation), or atraumatic (congenital or volitional) instability. Macrotraumatic instability is most commonly produced by a posteriorly directed force to the flexed and/or horizontally adducted arm. Microtraumatic injury is most commonly attributed to recurrent subluxation and clinicians must be aware of the high frequency of bidirectional or multidirectional patterns of GHJ laxity or instability.4 The soft tissue pathology responsible for posterior instability is not related to a single lesion but is most commonly the result of posterior capsular deficiency (due to tearing, stretching, or redundancy) and/or a posterior labral injury (reverse Bankart lesion). Thinning of the infraspinatus tendon also has been reported in cases of recurrent posterior instability. In some cases, bony alignment, glenoid retroversion, or posterior glenoid erosion may be causative factors and necessitate additional operative management.4,5 Reported rates for return to function following posterior GHJ reconstruction range from 50% to 96%.2,5–9 A comprehensive rehabilitation program following open or arthroscopic reconstruction is necessary to optimize upper extremity function.
Operative treatment
Surgical management of posterior GHJ instability focuses predominantly on restoration of posterior capsulolabral tissue integrity and restraint. The anterior capsuloligamentous tissue can also contribute to preventing posterior subluxation.10 Open reconstruction for posterior instability, first described in 1944,11 was the only technique described in the literature until the mid-1990s. Success rates following open reconstruction have been reported as high as 96%, although the number of patients that return to their preinjury sporting level has been reported as low as 30%.1
Arthroscopic repair of posterior GHJ pathology gained popularity in the 1990s and has been shown to produce equal if not better outcomes than open reconstruction in returning patients to maximal levels of functional ability.12 Arthroscopic techniques provide improved visualization of the entire GHJ with the advantage of less violation of musculotendinous tissue and therefore a more active early rehabilitation period. Isolated arthroscopic capsulorrhaphy consists of placating the capsule on itself to the posterior labrum. The posterior capsular repair consists of tightening the relatively thin posterior capsule and often includes the posterior band of the inferior glenohumeral ligament.3,13 When capsulolabral repair is conducted the capsulolabral complex is fixed to the posterior bony rim of the glenoid.10 In the case of arthroscopic reconstruction for isolated posterior instability, recurrence rates range from 0% to 12% with return to high level sports of 67% to 80%.2,7,8 While arthroscopic stabilization has gained favor, open techniques continue to be used primarily to address osseous defects and for some revision surgeries.
Rehabilitation guidelines
Management of pain and inflammation
Sling immobilization following surgery is universal and necessary to protect the surgically repaired tissue. Immobilization also will aid in resolution of pain and inflammation. Following an open posterior repair patients are usually immobilized for 6 weeks, whereas those who undergo the arthroscopic procedure may begin weaning from the sling at about 4 weeks.1,3,9,12 Recommended positions for sling immobilization vary from neutral abduction (ABD) and neutral rotation to 30 degrees ABD with neutral rotation.
Intermediate through return to activity phase (6 weeks to >6 months)
Range of motion progression
Acute phase (0 to 6 weeks)
Range of motion exercises following reconstruction should follow a gradual progression with extreme caution in the early postoperative phase to avoid posterior capsule stresses. Mobility exercises begin with Codman’s exercises supported by the uninvolved upper extremity. Unsupported Codman’s exercises during the first couple of weeks of the acute recovery phase are often performed incorrectly because of patient guarding. Supported Codman’s involve supporting the elbow of the involved arm and performing circular patterns of increasing size while maintaining the arm in neutral rotation (Figs. 28-1 and 28-2). It is recommended to perform range of motion (ROM) exercises sitting or standing rather than supine. Scapular mobility is restricted when supine because of the patient’s body weight, and unwarranted posterior capsular stress can be produced.
Passive range of motion (PROM) exercises are best performed initially by a physical therapist or certified athletic trainer to enable patient relaxation of the arm and avoidance of undesired muscular activity. Once the patient is able to relax the arm, various methods of PROM exercise can be introduced. Pulleys are a popular method to enable the patient to perform ROM exercises at home, but they can be detrimental and contribute to glenohumeral joint impingement if GHJ and scapulothoracic movement quality is not emphasized and monitored. The patient must be educated on ROM limits and awareness of quality of motion to ensure GHJ mobility without elevation of the shoulder complex. Use of towel slides (Fig. 28-3) or rolling of the arm over a physioball are additional methods to promote ROM in the acute postoperative phase. The change in shoulder position is produced by movement of the trunk, without recruitment of the shoulder musculature, during this acute phase. Active motion of the elbow, wrist, and hand should be performed throughout the acute phase following either surgical procedure. Loss of elbow extension resulting from prolonged sling wear and failure to perform AROM exercises during this phase is entirely avoidable.
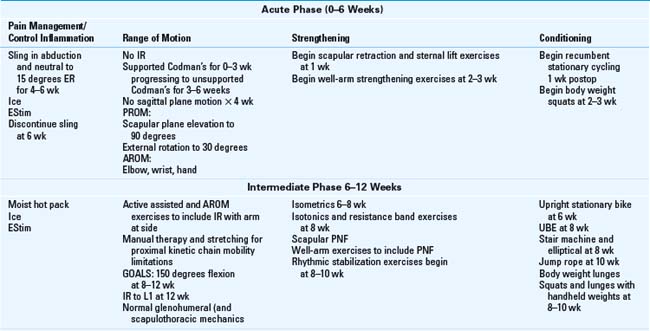
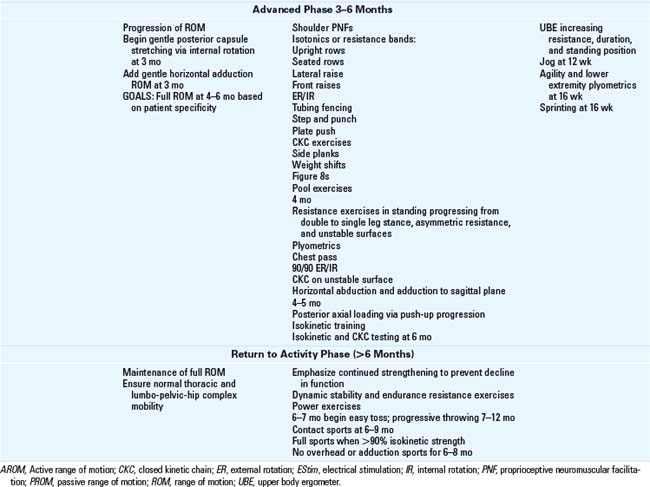
In the acute rehabilitation phase, ROM progression following open reconstruction is delayed in comparison with the arthroscopic reconstruction and limited to only passive motion (Tables 28-1 and 28-2). Shoulder elevation should be performed in the plane of the scapula to avoid undue posterior capsular stress imposed by shoulder elevation (flexion) performed in the sagittal plane. Internal rotation (IR) and horizontal adduction also are avoided throughout the acute phase in order to protect the posterior capsule and support healing of the surgically repaired tissues. At 6 weeks postoperatively, the open reconstruction patient can begin active-assisted ROM (AAROM). In contrast, the postarthroscopic patient can begin AAROM at 3 weeks. AAROM exercises should begin with short lever arm (elbow bent) scapular plane elevation to reduce muscular demands on the shoulder and promote gradual progression of soft tissue stress. Short lever arm exercises with limb support are recommended to gradually increase muscular demands while still protecting the GHJ.14 Methods of performing short lever arm AAROM include the use of a cane, pulleys, T-bar (Fig. 28-4), or physioball (Fig. 28-5).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree