1.6 Reflex Incontinence Caused by Underlying Functional Disorders
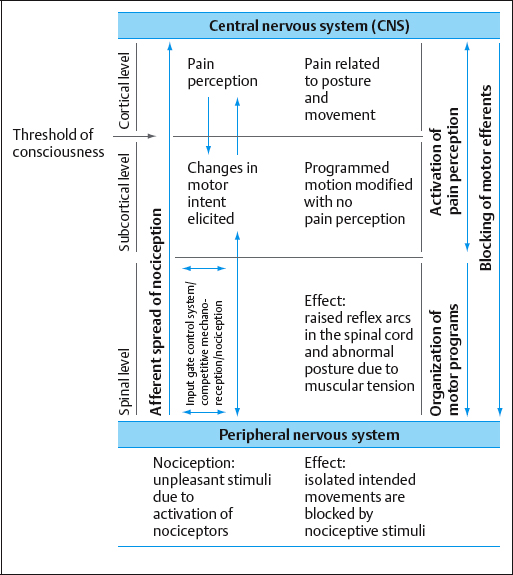
This type of incontinence is a symptom of an underlying disorder that needs be identified. According to Brügger [1977, 2000] the primary cause of most disorders of the motor system is not structural in nature, but rather an expression of certain protective mechanisms in the brain mediated by the central nervous system. These protective mechanisms are initiated by nociceptive afferent messages arising from faulty or excessive strain. The result is a changed sequence of movements and corresponding pathophysiological alteration of the infrastructural performance and functioning of the inner organs. If the nociceptive input is not excessive, these sequences take place at a corticosubcortical level. Consequently, the symptoms can only be diagnosed through their functional expression, since they cannot be experienced consciously. The protective mechanism of the neuromusculoskeletal system responds by reflex changes in muscular tone, leading to hypotonic or hypertonic changes in the tendons and muscles. Since a change in tone of this type is controlled by the central nervous system, it will persist until the underlying disorder is resolved (Fig. 1.56).
If the nociceptive input is excessive, the nociceptive messages are conducted to the cortex, where they are interpreted as warning signs— e. g., pain, fatigue, weakness, or stiffness.
If the faulty stresses become chronic, these initially functional reflex changes result in the development of morphological disorders in the specific structures affected by the generating stimuli.
 Reflex Incontinence
Reflex Incontinence
Reflex incontinence is a type of incontinence that does not originate primarily in the muscles of the pelvic floor. Instead, it is the expression of a protective mechanism mediated by the central nervous system in response to a functional disorder of the motor system. The musculature of the pelvic floor first affects this protective mechanism by increasing or decreasing muscular tone [Rock 1999]. The result of either of these responses is reduction in both elasticity and strength, due to diminished eccentric or concentric contractility respectively. These symptoms are expressed as reflex incontinence.
If the causes of functional disorders of the motor system are not eliminated, chronic malfunctioning of the pelvic floor muscles of this type can lead to structural changes such as fibrous infiltration into the connective tissue [Rock 1999].
 Upright Posture
Upright Posture
According to Brügger [1977, 1996, 2000] the upright posture, with thoracolumbar lordosis, is the result of a complex interplay of the muscles of the trunk and extremities. These are coordinated under neurophysiological guidance and dependent on their underlying infrastructural activities. An understanding of this neurophysiological interplay is basic to the diagnosis and treatment of functional disturbances of the motor system.
 Structure of the Upright Posture
Structure of the Upright Posture
The trunk and the extremities form an interdependent stochastic system. That is, every position and movement of the trunk influences the position and movement of the extremities, and vice versa.
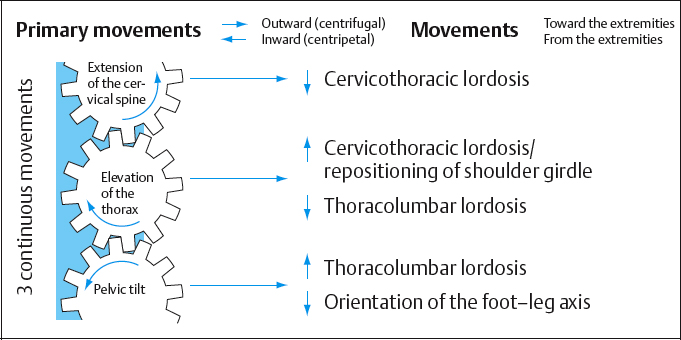
The Cogwheel Model
To illustrate these complex relationships, Brügger [1986] devised the cogwheel model (Fig. 1.57). The cogwheels represent the movements of the trunk: pelvic tilt, elevation of the thorax and extension of the neck. Forward and downward tilt of the pelvis induces lumbar lordosis above and distally influences the position of the axis of the foot on the lower leg. Translation of the thorax upward and forward creates posterior displacement of the shoulder girdle and induces both thoracolumbar and cervicothoracic lordosis. Movement of the occiput backward and upward leads to cervicothoracic lordosis, resulting in elevation of the thorax. The synergistic actions of the extremities, such as external rotation of the arms in the shoulder joints and abduction/external rotation of the legs in the hip joints, facilitate raising the trunk into the erect posture (Fig. 1.57). The model demonstrates the way in which malfunctions in the system have an effect on the whole motor system.
Anterior Pelvic Tilt and Flexion at the Hip Joint from the Proximal Lever (the Pelvis)
Tilting the pelvis anteriorly and flexing the hip joints from the proximal lever (pelvis) are two separate movements in which the axis of rotation depends on the position of the pelvis at the starting position. The axis of rotation (fulcrum) is the point at which the least displacement occurs in the course of a movement. In the sitting position, the axis of rotation of the pelvis is the ischial tuberosity [Brügger 1977, Rock 1997]. The axis of rotation cannot be located in the hip joint, since this moves through a longer path when the pelvis is tilted. A pelvic tilt—i. e., anterior rotation of the pelvis—can only occur while the ischial tuberosities remain in contact with the seat. Once the ischial tuberosities are no longer in contact with the seat, the proximal lever (pelvis) effects flexion at the hip. Flexion of the hip at the proximal lever instead of the intended pelvic tilt indicates that the course of the movement is pathophysiological. Similar considerations apply to pelvic movements while standing. The axis of rotation of the pelvis in this case lies in the acetabulum [Brügger 1977, Rock 1997]. The result is that a pelvic tilt can only be determined by functional criteria. The essential functional criterion here is optimal activation of the transversus abdominis muscle (see section 2.6, pp. 252–266), because it requires thoracolumbar extension that entails anterior tilting of the pelvis and elevation of the thorax.
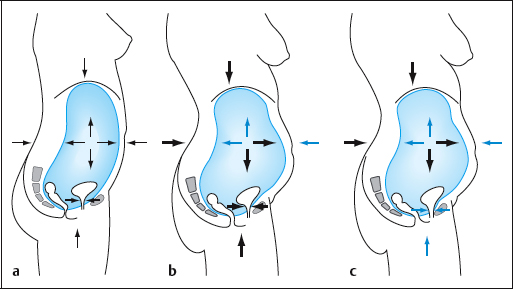
The Pressure System in the Body Cavities
The trunk can be divided into two visceral cavities—the thorax and abdomen. The greater omentum subdivides the abdominal cavity into abdomen and true pelvis. Hence, the structures and organs of the trunk form a tripartite system of cavities. Within this system, external pressure has to balance internal pressures, and pressure has to balance counterpressure. On the one hand, this resists the constant effect of gravity, which strives to force the body into a flexed posture; on the other hand, physiological pressure relationships provide good prophylaxis against ptosis (descent of the inner organs) (Fig. 1.58) [Stone 1996].
The dynamic upright posture (see section 1.4) provides the foundation for this type of balance. It makes possible the functional synergistic coordination of the trunk with the extremities and the system of bodily cavities. Among other consequences, it ensures the coordination of the work of the thoracic diaphragm, the abdominal muscles (transversus abdominis), and the pelvic floor muscles (see sections 1.5 and 2.6).
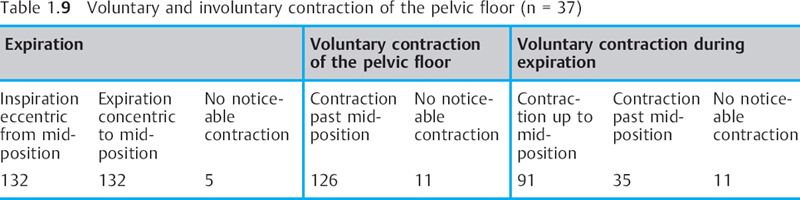
Brief increases in intraabdominal pressure such as those that occur during coughing and sneezing can be compensated for by additional bladder closing mechanisms [Bücheli et al. 1994, Fischer and Kölbl 1995]. One of these closure mechanisms occurs at the proximal urethra, assuming that this is attached physiologically to the pelvic floor muscles and the pubourethral ligaments. Other mechanisms are the periurethral muscles of the urogenital diaphragm and parts of the pubococcygeus, which undergo what is regarded as a reflex contraction. Voluntary activation of the pelvic floor muscles leads to elevation of the bladder neck. In contrast, the bladder neck remains in mid-position during coughing in women without symptomatic incontinence [Wijma et al. 1991, Deindl et al. 1994]. This is part of the physiological closing mechanism. Often, voluntary activation of the pelvic floor muscles is used to support the closing mechanisms during increases in intraabdominal pressure such as those that occur during coughing and sneezing. There is a difference between voluntary activation of the pelvic floor muscles, resulting in elevation of the bladder neck, and physiological activation resulting in a mid-position of the pelvic floor musculature. This means that different functional results are obtained if one compares voluntary activation and physiological (reactive) activation. This has to be borne in mind, and the question is what kind of activation is desired with any given patient. With voluntary activation, the mid-position will not be reached unless the patient has a descent, prolapse, etc.
In view of this, DeLancey [DeLancey 1996, DeLancey and Ashton-Miller 2004] raises the question of whether occlusion of the urethra under stress is really due to its elevation. In his opinion, timing plays a cardinal role in the recruitment of the physiologically powerful musculature of the pelvic floor that maintains the mid-position of the urethra.
DeLancey’s theory is supported by the fact that the muscles of the pelvic floor are activated before intraabdominal pressure rises during coughing and sneezing [Richardson et al. 1999, Sapsford 2000]; this fact indicates that in neurophysiological conditions, coughing and sneezing are programs that have a corresponding forward-feeding mechanism, organized by the central nervous system. In this process, the pelvic floor muscles and the transversus abdominis muscle function eccentrically during the initial phase (pressure build-up by deeper inspiration) and concentrically during coughing and sneezing.
Intra-abdominal pressure also rises during defecation. In this case, the special need is for the puborectalis to act in concert with the muscles of the anal sphincter. The eccentric activity of the puborectalis allows the muscles to support the rectum without impeding defecation.
 Action of the Transversus Abdominis Muscle when Posture is Physiological
Action of the Transversus Abdominis Muscle when Posture is Physiological
Anatomically, the transversus abdominis muscle connects the pelvis with the thoracic cage (ribs) and via the lumbar fascia to the spinal column. Accordingly, it can be expected that the position of the pelvis, the spinal column, and the thorax will influence the actions of the transversus abdominis muscle, which will influence their position in turn.
Brügger [1977] long ago drew attention to the role of the transversus abdominis muscle in raising the body from a flexed to an upright posture.
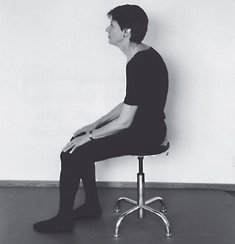
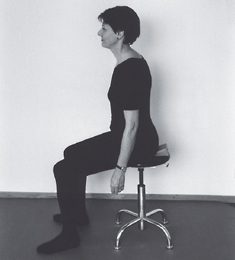
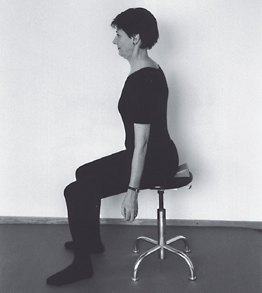
With the correct anteroinferior movement of the pelvis and simultaneous anterosuperior elevation of the thorax, the concentric action of the transversus abdominis muscle can easily be verified both by inspection and palpation, as the waist narrows and the abdominal wall tightens (Figs. 1.59, 1.60).
On the other hand, if the anterior pelvic tilt is replaced by hip flexion at the proximal lever arm, the abdomen remains protruded and the width of the waist does not change. Hence, the key movement for inducing the transversus abdominis muscle to straighten the body physiologically is to learn to move the pelvis correctly forward and downward while maintaining contact with the tuberosity, and at the same time elevating the thorax forward and upward.
It would appear that the neutral anatomical position of the pelvis should form the observational criterion for the correct upright posture (see section 1.4). However, the functionally normal position of the pelvis [Rock 1997] features a slight forward pelvic tilt, in which the anterior superior iliac spines move very slightly in front of the symphysis. This is the only way in which the shear forces in the sacroiliac joint can be offset. If the pelvis remained in the anatomically normal position, shear forces would continue, since the anterior weighting of the thorax and the inner organs in front of the spinal column would create a rotational strain at L5-S1.
In various studies on loading in the spinal column, Richardson et al. [1999] were able to demonstrate that the transversus abdominis muscle is activated before the erector spinae. This finding confirms the role of the transversus abdominis muscle in stabilizing the spinal column. It also confirms Brügger’s concept that the primary function of the erector spinae musculature is not to raise the trunk into the erect posture, but rather to fine-tune the segments [Brügger 2000, Vele 1998].
The Role of Posture for Generating Strength in the Transversus Abdominis Muscle
Sapsford et al. [2001] demonstrated that the position of the lumbar vertebrae in extension or flexion, together with the degree of pelvic tilt during voluntary contraction of the pelvic floor muscles, changes the electromyography (EMG) tracing from the various abdominal muscles.
In flexion, the action of the external oblique was the strongest. The rise in the amplitude of the EMG of the transversus abdominis muscle exceeded that of the rectus and the internal oblique when the spinal column was in extension.
Sapsford et al. [2001] point out that exercise with the spinal column in flexion will impede the recruitment of the transversus abdominis muscle and rather favor the flexing action of the remaining abdominal muscles. At present, there is general agreement that activation of the transversus abdominis muscle is greater with the spinal column in extension than in flexion [Sapsford et al. 2001]. See p. 87, Fig 1.51.
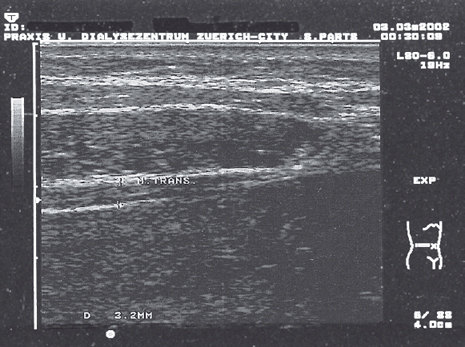
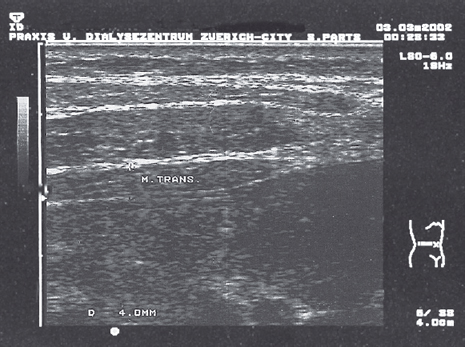
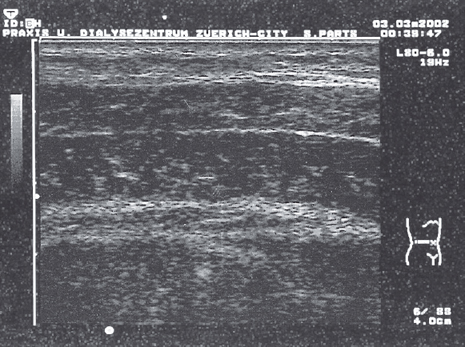
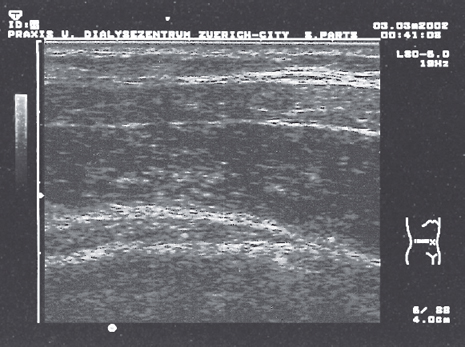
To resolve the question of the extent to which contraction of the transversus abdominis muscle is affected by posture or position, its activity was displayed in various postures in expiration using ultrasound. The least activity in the transversus abdominis muscle was found in a flexed posture (strained posture) and protruding abdomen. When the position of the pelvis was normal, the activity of the transversus abdominis muscle was more powerful than in the strain posture (Figs. 1.61–1.64).
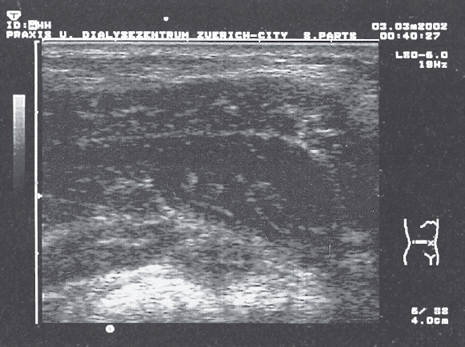
The upright posture, with the correct pelvic tilt and elevation of the thorax advocated by Brügger, showed increased activity of the transversus abdominis muscle (Figs. 1.65–1.67). By comparison, the hollowing [Sapsford 2000] that results from voluntary activation of the transversus abdominis muscle when the lower abdomen is pulled in gently while extension of the spinal column is maintained, created more activity in the transversus abdominis muscle with the pelvis tilted forward than in the neutral pelvic position (Figs. 1.68, 1.69).
This finding confirms previous clinical experience in which the transversus abdominis muscle was felt by palpation to be activated more strongly when the pelvis was tilted.
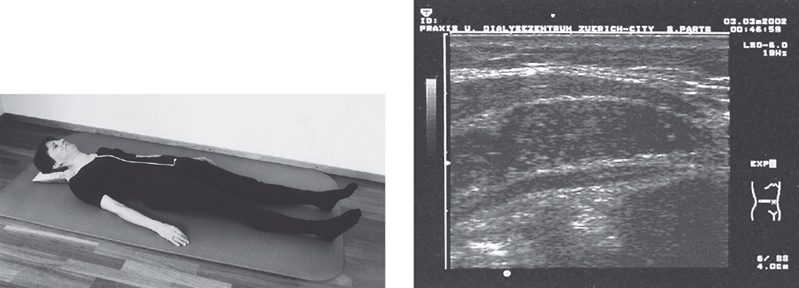
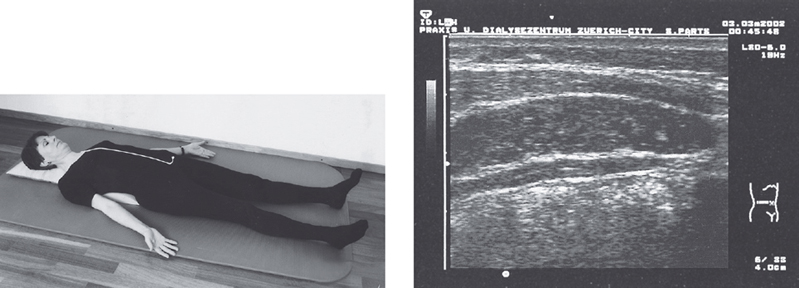
Brügger [1977,1986, 2000] pointed out that in most subjects, the supine position combines a dorsal tilt of the pelvis with simultaneous flexion of the lumbar spine. For this reason, he advocates thoracolumbar support of the spinal column in the supine position [Brügger 1986]. Previously, the transversus abdominis muscle was shown clinically to be palpably active with thoracolumbar support. This has now been demonstrated by ultrasound (Figs. 1.70, 1.71).
Synergistic Action of the Transversus Abdominis Muscle and the Pelvic Floor Muscles
Sapsford et al. [1997a, 1997b, 2001] and Richardson et al. [1999] have demonstrated that voluntary concentric contraction of the transversus abdominis muscle and contractions of the pelvic floor muscles activate each other. Critchley [2002], using ultrasound, was able to show that when the transversus abdominis muscle acted in concert with the muscles of the pelvic floor, its thickness increased by 15% more than when it acted alone. Neumann and Gill [2002], in the course of their EMG studies, demonstrated that during pelvic floor muscle contraction in both the supine and standing positions, the transversus abdominis muscle and the internal oblique muscles were also active. The same studies showed that none of the subjects was able to contract the pelvic floor muscles effectively when the deep abdominal muscles were relaxed. It is possible to show using ultrasound that the Brügger upright posture facilitates optimal activation of the transversus abdominis muscle (Figs. 1.65–1.67). It follows that Brtigger’s upright posture must automatically also activate the pelvic floor muscles. B⊘ et al. [2003] compared the effect of elevating the levator plate (levator ani) during contraction of the pelvic floor muscles, contraction of the transversus abdominis muscle, and combined contraction of transversus abdominis and pelvic floor muscles. As a control, correct contraction of the transversus abdominis and of the pelvic floor muscles was first determined in the supine position. The actual study was then carried out with the subjects in a bent supine posture, with two pillows placed under the head for comfort. Consequently, the spinal column was flexed during the study, so that the transversus abdominis muscle could no longer be activated optimally, since that would require extension of the spine. Most likely the external oblique would be recruited during contraction, since this is the muscle most easily activated in the flexed position [Sapsford et al. 2001]. B⊘ et al. [2003] concluded from their investigations that contraction of the pelvic floor muscles is more effective than that of the transversus abdominis muscle in 61.6% of cases, and more effective than the combined contraction of transversus abdominis muscle and the pelvic floor muscles in 24.1 % of cases. In six subjects, the pelvic floor muscles descended during contraction of the transversus abdominis muscle. However, in four of these subjects, the pelvic floor muscles could be raised again by combined contraction of the pelvic muscles. Even when the pelvic floor muscles contracted, one subject experienced descent of the pelvic diaphragm. However, because of the initial flexed position, no conclusions could be drawn concerning the effect of the contraction of the transversus abdominis muscle on the descent of the pelvic floor muscles. It is of interest, however, that the subject who induced a descent both with contraction of the pelvic floor muscles and with contraction of the transverse was able to raise the pelvic floor when both muscles contracted at the same time. The authors do not mention this fact.
Incontinence is often induced by coughing and sneezing, which require synergistic contractions of the abdominal and pelvic muscles (Tables 1.8–1.10). These contractions are involuntary muscle actions that are part of a corresponding reflex (see pp. 106–108 below). Moreover, since it seems likely that the pelvic floor musculature moves differently from its mid-position depending on whether a contraction is voluntary or involuntary, the studies by B⊘ et al. [2003] are unable to show which contraction causes physiological shifting of the pelvic floor muscles. This topic would require further studies. Based on their studies, the authors advise against indirect activation of the pelvic musculature through the transverse muscle. This treatment recommendation is not tenable, however, since the problems mentioned above mean that the study’s validity is uncertain.
| Muscle group | Contraction type during inspiration | Contraction type during expiration |
|---|---|---|
| Diaphragm Transversus abdominis (abdominal muscles) Pelvic floor | Concentric Eccentric Eccentric | Eccentric Concentric Concentric |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree