The reported prevalence rates of pain within the pelvis range from 3.8% to 24% in women aged 15 to 73 years. Despite the significant number of women affected, pelvic floor pain and dysfunction are commonly overlooked in women seeking medical care. Physiatrists are uniquely qualified to manage these patients because of their knowledge of the musculoskeletal and nervous systems and their awareness of the relationships among pain, physiology, and function. When evaluating women who have pelvic pain, practitioners must ask questions about history of urinary or fecal incontinence, dyspareunia, or pelvic pain with certain activities or associated with menses, surgery, or trauma. If left unidentified, pelvic floor dysfunction can deter individuals from normal bowel and bladder function, intimacy, and even engagement in work and social functions. This article introduces pelvic floor anatomy, neurophysiology, and function and provides an overview of pelvic pain and pelvic floor dysfunctions and their recognition and treatment.
Reported prevalence rates of pain within the pelvis range from 3.8% to 24% in women aged 15 to 73 years . Despite the significant number of women affected, pelvic floor pain and dysfunction are commonly overlooked in women seeking medical care. This oversight may be attributed to changes in medical practice that restrict time spent with patients, the often embarrassing and personal nature of the subject, the social stigmas for some cultures, or the perceived notion that no effective treatment exists. Overlap exists among medical specialists who treat patients who have pelvic pain, including gynecologists, urologists, gastroenterologists, and colorectal surgeons. Physiatrists are uniquely qualified to manage patients who have pelvic pain because of their knowledge of the musculoskeletal and nervous systems and their awareness of the relationships among pain, physiology, and function. Their approach is also nonsurgical. As with many other conditions, a procedure does not always exist that fits the disorder, and the physiatrist can offer that missing link for some patients.
Early recognition or prevention of pelvic floor dysfunction may literally change the trajectory of individual’s life, especially late in life. The top three reasons for nursing home admission (reduced mobility, urinary incontinence, and fecal incontinence) have pelvic floor dysfunction as a common theme . This article introduces pelvic floor anatomy, neurophysiology, and function and provides an overview of pelvic floor dysfunctions and their recognition and treatment.
Anatomy of the pelvic floor
The pelvic floor is a dome-shaped striated muscular sheet or sling that, together with the endopelvic fascia, supports the bladder, uterus, and rectum ( Fig. 1 ). Specialized smooth muscular urinary and anal sphincters allow for storage and evacuation of urine and stool. Pelvic floor muscles attach to local pelvic bony structures along the inner surface of the lesser pelvis. However, global muscles from the lumbar spine and lower extremities and their fascia play a large supportive role in lumbopelvic stability and mobility. The pelvic floor muscles include the levator ani (iliococcygeus, pubococcygeus, and puborectalis) muscles and the coccygeus. The paired levator ani and coccygeus muscles, together with the fascia above and below, are sometimes referred to collectively as the diaphragm of pelvis . The levator ani arises from the posterior surface of the superior ramus of the pubis, lateral to the symphysis, and attaches to the inner surface of the spine of the ischium along with the obturator fascia and tendinous arch of the pelvic fascia. The fibers of the levator ani pass downward and backward toward the middle of the pelvis with attachments to the coccyx and anococcygeal raphe. The latter extends between the coccyx and anus. Midline fibers insert into the rectum and blend with fibers of the sphincter muscles, whereas anterior fibers can invest in the sides of the prostate in men and the vagina in women. At the central tendinous portion of the perineum, the levator ani joins the fibers of the more superficial pelvic floor muscles, the transversus perinea (transversus perinea superficialis and profundus).

Structure of the pelvic walls
The pelvic walls are formed by bones and ligaments partly lined with muscles and covered with fascia. The anterior pelvic wall is a shallow wall formed by the posterior surfaces of the pubic bones and symphysis pubis. This landmark is easily identified with palpation on most patients. The posterior pelvic wall is a more extensive wall, consisting of the sacrum, coccyx, and piriformis muscle.
The lateral pelvic wall is a component of the pelvis formed by part of the innominate bone, the obturator foramen, the sacrotuberous and sacrospinous ligaments, and the obturator internus muscle and fascia. The inferior pelvic wall or pelvic floor consists of the levator ani muscles, coccygeus, and pelvic fascia and is accessible to palpation only through internal pelvic or rectal examination.
Joints of the pelvis
The pelvis is a ring and the base of support for the upper and lower torso and extremities. Forces are ultimately distributed through the pelvis directly and indirectly. Located in the posterior pelvic ring are the sacroiliac joints. These are synovial joints inferiorly, have anterior and posterior capsules, and are surrounded by ligaments. The anterior sacroiliac ligament acts as a sling. The dorsal longitudinal sacroiliac joint (SIJ) ligament crosses the joint and attaches to the dorsal surface of the sacrum and ilium in three layers lying in oblique planes to one another. In isolation, this ligament is believed to contribute to posterior pelvic pain because it contains both pain receptors and proprioceptors and absorbs forces directly from the SIJ and indirectly from the hip The interosseous sacroiliac ligaments are short ligaments within the SIJ and connect the sacrum to the ilium. They are believed to be among the strongest ligaments in the body. Ligaments extrinsic to the SIJ but that contribute to posterior pelvic pain include the iliolumbar and sacrotuberous ligaments. The iliolumbar ligament absorbs and distributes forces from the lumbar spine and ilium. The sacrotuberous ligament absorbs and distributes forces from the lower extremity through direct and fascial attachments to the hamstrings and thoracodorsal fascia . All of these ligaments are important for joint stability .
The symphysis pubis is a cartilaginous joint between the two pubic bones. It is surrounded by ligaments that allow subtle motion in frontal (inferior and superior sheer motion) and rotational planes. This joint is subjected to substantial mechanical stresses during pregnancy.
The sacrococcygeal joint is a cartilaginous joint that is joined by ligaments. Much movement is possible at this joint, although this varies among individuals. Women who have a previous history of direct trauma to the coccyx region may have healed in an asymmetric alignment or may continue to have increased mobility of the segment that may be symptomatic with routines activities of daily living, direct pressure at the site, gluteal contraction, defecation, or intercourse. These should all be investigated in women whose presentation of pelvic pain includes coccyx pain.
Nerves of the pelvis and perineum
The lumbosacral trunk passes into the pelvis and joins the sacral nerves as they emerge from the anterior sacral foramina. From a clinical perspective, the important nerve branches associated with clinical syndromes at or near the pelvic floor include sciatic, obturator, femoral, lateral femoral cutaneous, and pudendal. The clinical anatomy of the pudendal nerve and its branches make it prone to damage during complicated vaginal childbirth and surgical interventions. The pudendal nerve arises from the sacral plexus from the ventral branches S2, S3, and S4. It passes between the piriformis and coccyges muscles as it travels from the pelvis through the greater sciatic foramen and then passes over the spine of the ischium to reenter the pelvis through the lesser sciatic foramen. This nerve supplies sensation to the external genitalia and motor function to the urinary and external anal sphincters and muscles responsible for ejaculation in men and orgasm in both genders ( Fig. 2 ).
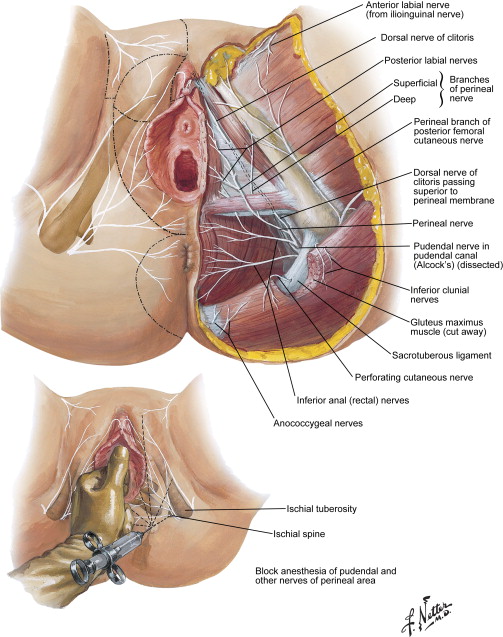
Because of its complex and comprehensive function, the pudendal nerve is implicated in pelvic floor dysfunction related to pain, incontinence, and sexual dysfunction. In one study , a pudendal nerve block decreased vaginal pressures, increased the length of the urogenital hiatus, and decreased electromyography activity of the puborectalis muscle, suggesting that the pudendal nerve innervates the levator ani muscle . Other studies show that the motor branch to the levator ani, the levator ani nerve, approaches the pelvic floor muscles on their visceral side. Near the ischial spine, the levator ani nerve and the pudendal nerve lie above and below the levator ani muscle, respectively. The median distance between the levator ani nerve and the point of entry for a pudendal block into the levator ani muscle is 5 mm. Therefore, a transvaginal pudendal nerve blockade will probably block both nerves simultaneously . Other authors disagree that the pudendal nerve sends a branch to the levator ani. Gross dissections of cadavers suggest that innervation of the female levator ani muscle ias not provided by the pudendal nerve but rather originates directly from the sacral nerve roots (S3–S5) that travel on the superior surface of the pelvic floor. Because definitive studies involving nerve transection and neural tracer studies cannot be performed in living humans, further investigations using appropriate animal models may delineate the neuroanatomy .
Hip and pelvis injuries
Pelvic and hip injuries can be divided into bony and soft tissue causes. Bony causes include but are not limited to osteoarthritis, stress fractures, avulsion injuries, acetabular labral tears, femoral acetabular impingement, osteitis pubis, and avascular necrosis of the head of the femur. Soft tissue conditions include muscle strains, tendonitis, bursitis, and nerve entrapment. As in other areas of the body, local splinting of the pelvic floor diaphragm may result from painful hip and pelvis injuries. Conversely, prolonged maladaptive hypertonic or hypotonic pelvic floor dysfunction may change joint loading, leading to musculoskeletal sequela such as degenerative joint disease of the hip. This article briefly mentions these disorders, because each may refer pain to the pelvic floor. Pelvic floor pain may develop secondary to spine or pelvic trauma and should be incorporated into the treatment plan.
Hip and pelvis injuries
Pelvic and hip injuries can be divided into bony and soft tissue causes. Bony causes include but are not limited to osteoarthritis, stress fractures, avulsion injuries, acetabular labral tears, femoral acetabular impingement, osteitis pubis, and avascular necrosis of the head of the femur. Soft tissue conditions include muscle strains, tendonitis, bursitis, and nerve entrapment. As in other areas of the body, local splinting of the pelvic floor diaphragm may result from painful hip and pelvis injuries. Conversely, prolonged maladaptive hypertonic or hypotonic pelvic floor dysfunction may change joint loading, leading to musculoskeletal sequela such as degenerative joint disease of the hip. This article briefly mentions these disorders, because each may refer pain to the pelvic floor. Pelvic floor pain may develop secondary to spine or pelvic trauma and should be incorporated into the treatment plan.
Urinary continence
Urinary continence depends on central and local neurologic and musculoskeletal control along with an adequate level of cognition and physical functioning. A full review of continence is beyond the scope of this article, although continence issues related to the pelvic floor are briefly discussed . Increases in abdominal pressure during activities of daily living challenge continence. Supportive and sphincteric structures must be functional to prevent incontinence and prolapse of genital organs . Urethral closure pressure is maintained higher than bladder pressure through the combined action of the urethral sphincter and a supportive hammock under the urethral and vesical neck. This supporting layer consists of (1) the anterior vaginal wall and the connective tissue that attaches it to the pelvic bones, (2) the pubovaginal portion of the levator ani muscle, and (3) the uterosacral and cardinal ligaments constituting the tendinous arch of the pelvic fascia. The number of striated muscle fibers of the sphincter decreases with age and parity. Computer models indicate that vaginal birth places the levator ani under tissue stretch ratios of up to 3.3 and the pudendal nerve under strains of up to 33%.
Anorectal continence
The internal and external anal sphincters are primarily responsible for maintaining fecal continence . Defecation is a somatovisceral reflex regulated by dual nerve supply, including somatic and autonomic to the anorectum. The net effects of sympathetic and cholinergic stimulation are to increase and reduce anal resting pressure, respectively, and to allow for storage or voiding as appropriate. Fecal incontinence and functional defecatory disorders may result from structural changes or functional disturbances in the mechanisms of fecal continence and defecation.
Viscerosomatic reflex
Viscerosomatic reflexes result from afferent stimuli from viscera affecting somatic tissues. Visceral receptors send afferent impulses through the dorsal horn of the spinal cord to synapse on interconnecting neurons. These neurons convey impulses to the sympathetic and peripheral motor efferents, resulting in sensory and motor changes in muscle, skin, and fascia of the trunk, including the pelvic floor. Persistent muscle contraction of the pelvic floor related to noxious visceral stimulation, such as that associated with endometriosis or irritable bowel syndrome, can cause splinting and pain with reduction of normal pelvic floor muscle function. The body adapts by recruiting nearby muscles, such as the psoas and iliacus, which can cause related symptoms such as posterior pelvic and lower back pain. Manual treatment may be advocated to address the restrictions in the somatic structures that may be secondary to a primary visceral disorder. Treatment of local muscle and joint dysfunction will also treat the viscerosomatic reflexes that may cause the symptoms , resulting in reduced pain, increased mobility and muscle excursion, and enhanced lymphatic and venous drainage. The ultimate goal is to restore normal pelvic floor neuromuscular control to allow for normal voiding.
Pelvic floor dysfunction overview
Pelvic floor dysfunction describes pain or abnormal function of the muscular sling within the bony pelvis. Box 1 provides examples of additional dysfunctions associated with pelvic pain. The pelvic floor supports viscera, sphincter function, hip and trunk movement, and sexual function. Dysfunctions are commonly divided into hypertonic and hypotonic. Hypertonic , or high-tone, dysfunctions include pain and excessive muscle tension and can present with associated constipation and dyspareunia (pain with intercourse). Hypotonic , or low-tone, dysfunctions can present with incontinence and may be related to collagen changes, previous childbirth or gynecological surgery, or peripheral nerve injury. Women who exercise may describe their pelvic floor pain as acute or insidious at onset. These women often seek medical advice when their athletic performance declines or they are no longer able to exercise. In these circumstances, health care providers must acknowledge the woman’s desire to return to or continue with sports or exercise and should offer an alternative form or intensity of exercise during evaluation and treatment of the pelvic floor dysfunction.
Dyspareunia
Dysmenorrhea
Vulvodynia
- •
Hyperpathia
- •
Burning
- •
Itching
Involuntary spasms of muscles
- •
Vaginismus
- •
Pelvic floor tension myalgia
- •
Levator ani syndrome
Defecation dysfunction
- •
Constipation
- •
Diarrhea
- •
Fecal incontinence
- •
Rectal itching and burning
Voiding dysfunction
- •
Urinary urgency
- •
Urinary frequency
- •
Painful urination
Sexual dysfunction
- •
Anorgasmia
Coccygodynia
Lower back pain and upper leg pain
Mood disturbances
- •
Anxiety
- •
Depression
Fatigue (mental and physical)
As in other regions of the body, gender differences exist in the anatomy of the hips and pelvis, such as those listed in Box 2 . Women have broader pelvises than men, and those who have even broader and shallower pelvises may have greater hip range of motion. Women are more likely to have mild to severe developmental dysplasia of the hip, which may also contribute to greater degrees of hip motion and thereby increased need for balanced muscle strength and length to provide joint stability . The combination of greater femoral neck anteversion and shorter limb length leads to a lower center of gravity for women compared with men . Neuromuscular differences in firing patterns of motor units may arise from these anatomic differences, but have not been proven to increase injury risk . The ligaments, fascia, and muscles of the pelvic girdle support the force closure (muscles and ligaments that surround the joint to provide stability) of the SIJ working in concert with form closure (bony congruency of joint surfaces) . Alterations in force closure occur during pregnancy because of increasing abdominal girth, changes in load transfer, and deconditioning, in addition to ligamentous laxity caused by the shift in levels of hormones, including relaxin and estrogen. Inadequate closure may cause increased SIJ pain in pregnant women .






