Locomotion has always been a major criterion for human survival. Thus, it is no surprise that science supports the dependence of bone health on weight-bearing physical activities. The effect of physical activity on bone is site-specific. Determining how to perform osteogenic exercises, especially in individuals who have osteopenia or osteoporosis, without exceeding the biomechanical competence of bone always poses a dilemma and must occur under medical advice. This article presents the hypothesis that back exercises performed in a prone position, rather than a vertical position, may have a greater effect on decreasing the risk for vertebral fractures without resulting in compression fracture. The risk for vertebral fractures can be reduced through improvement in the horizontal trabecular connection of vertebral bodies.
Locomotion has always been a major criterion for human survival. Thus, it is no surprise that science supports the dependence of bone health on weight-bearing physical activities. “Bone, to be maintained, needs to be mechanically strained—within its biomechanical limits” .
Musculoskeletal challenges of aging
Bone loss and sarcopenia of aging cause an imbalance in the body’s musculoskeletal ability to withstand extensive mechanical strain. A mechanical strain to the skeletal structure can be as low as gravity alone and as high as the impact of a moving, energized body part as it contacts a hard floor. The point of no return for fracture is defined by the quality of the bone and supportive soft tissues of the musculoskeletal structure.
Bone loss related to aging is more challenging for the female skeleton than the male skeleton. In one study comparing the ash weight of vertebral bodies (L3) in the cadavers of men and women aged 18 to 96 years, women had significantly lower ash weight than men of the same age . Sarcopenia of aging affects women more than men because women start life with less muscle strength .
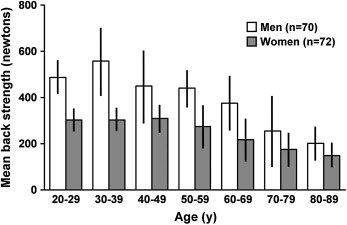
The process of bone remodeling affects bone loss more from metabolically hyperactive trabecular bone than cortical bone at menopause. The result is 47% bone loss from the spine during a woman’s life . The most significant bone loss occurs between ages 50 and 58 years, after sudden gonadal atrophy at menopause. In men, age-related axial bone loss is approximately 30% throughout life, and occurs more gradually because no sudden reduction in reproductive hormones occurs. The appendicular bone loss of aging is also less in men (15%) than in women (30%) . In boys and girls, axial and appendicular muscle strength is approximately the same until age 10 years, when a discrepancy begins to develop ( Fig. 1 ) .
Back extensor strength (BES) in women at different decades of life ranges from 54% to 76% of the strength in men ( Fig. 2 ) . This difference in BES between the genders decreases with age. By age 90, men have lost 64% of their maximal BES and women have lost 50% . Sarcopenia of aging affects type II (fast twitch) muscle fibers more than type I fibers. This process expands the ratio of type I motor neuron units at the expense of the type II fibers . The result of these changes is smaller, weaker muscles. Clinically, the consequence is a decrease in the protective role of muscles in locomotion and musculoskeletal health. The loss of muscle strength and bone mass creates more challenges for women than men, because women start life with less bone and muscle mass. In addition, other age-related spinal changes, such as facet arthropathies and reduction of resilience in intervertebral disks, decrease spinal flexibility and can subsequently increase risk for vertebral fracture.
A person who has a fear of falling tends to decrease locomotion and weight-bearing physical activities. In one study, healthy community-dwelling subjects who had osteoporosis had a significantly higher perceived risk for falls than control subjects . The fact that risk for falls increases with aging is well known . Participation in a moderate level of physical activity is a significant component of physical and mental health in older adults and can decrease death rate; however, loss of bone and muscle mass may limit their choice of physical activity. Limitation of locomotion is inevitable, whether it is caused by central nervous system disorders or the musculoskeletal changes of aging, which usually adds to premature frailty of aging. Risk for falls may increase because of extraskeletal or intraskeletal factors, which are listed in Box 1 .
Extrinsic
Environmental
Physical obstacles
Slippery floor
Uneven surfaces
Poor illumination
Ill-defined stairs
Pets
Icy sidewalks
Extraskeletal
Inappropriate footwear
Obstructive clothing
Intrinsic
Lower-extremity weakness (neurogenic or myopathic)
Balance disorder (eg, vestibular changes, peripheral neuropathy, hyperkyphosis)
Visual impairment, use of bifocals
Cognitive decline
Decreased coordination (eg, cerebellar degeneration)
Postural changes, imbalance, gait unsteadiness
Gait apraxia
Reduced muscle strength
Reduced flexibility
Respiratory difficulty (eg, orthopnea)
Postural hypotension
Cardiovascular deconditioning
Iatrogenically reduced alertness
Modified from Sinaki M. Prevention of hip fracture: physical activity. In: Senile osteoporosis. Ringe JD, Meunier JP, editors. Stuttgart: Georg Thieme Verlag Publications; 1996. p. 99–115; and Sinaki M. Falls, fractures, and hip pads. Curr Osteoporos Rep 2004;2(4):131–7; with permission.
Maintaining biomechanical competence of bone
Proper mechanical loading can increase osteoblastic activity and the rate of bone formation, but its mechanism is not fully understood . One study showed that job-related physical activity correlated significantly with bone mineral density of the spine ( Fig. 3 ) . This study showed that individuals working in a medical center who performed weight lifting at their jobs had greater bone mineral density than those engaged in a sedentary job. Some studies that used interventions to improve bone mass in humans did not show a significant increase in bone mass of the spine with weight-training exercises for the back extensor muscles . This unexpected result may be attributed to the low intensity of the exercise program, the method used to expose the bone to load, the subject’s compliance, or, perhaps, the genetic coding of the bone itself. However, the benefit of exercise on bone should not always be measured based on increased bone mineral density; the resulting changes in bone structure are important in increasing bone strength. One study in animals showed that mechanical loading improved bone strength by reshaping bone structure without increasing bone mineral density .
Preventing bone fracture, whether through increasing bone mineral density or reshaping the trabeculae, is the objective of clinical intervention. Most current medical literature focuses on the role of exercise in improving bone mass. In a recent long-term follow-up of a controlled trial, however, improved back muscle strength was shown to reduce the risk for vertebral fractures several years after the exercise program was discontinued . The results of this study prompted a new hypothesis that perhaps the exercises to decrease vertebral fracture should be different from loading exercises to increase bone mineral density in the upper and lower extremities.
Maintaining biomechanical competence of bone
Proper mechanical loading can increase osteoblastic activity and the rate of bone formation, but its mechanism is not fully understood . One study showed that job-related physical activity correlated significantly with bone mineral density of the spine ( Fig. 3 ) . This study showed that individuals working in a medical center who performed weight lifting at their jobs had greater bone mineral density than those engaged in a sedentary job. Some studies that used interventions to improve bone mass in humans did not show a significant increase in bone mass of the spine with weight-training exercises for the back extensor muscles . This unexpected result may be attributed to the low intensity of the exercise program, the method used to expose the bone to load, the subject’s compliance, or, perhaps, the genetic coding of the bone itself. However, the benefit of exercise on bone should not always be measured based on increased bone mineral density; the resulting changes in bone structure are important in increasing bone strength. One study in animals showed that mechanical loading improved bone strength by reshaping bone structure without increasing bone mineral density .
Preventing bone fracture, whether through increasing bone mineral density or reshaping the trabeculae, is the objective of clinical intervention. Most current medical literature focuses on the role of exercise in improving bone mass. In a recent long-term follow-up of a controlled trial, however, improved back muscle strength was shown to reduce the risk for vertebral fractures several years after the exercise program was discontinued . The results of this study prompted a new hypothesis that perhaps the exercises to decrease vertebral fracture should be different from loading exercises to increase bone mineral density in the upper and lower extremities.
Choosing a proper physical activity program
Determining how to perform osteogenic exercises, especially in individuals who have osteopenia or osteoporosis, without exceeding the bone’s biomechanical competence always poses a dilemma and must be done under medical supervision. Not all exercises are osteogenic. Several studies support the positive effect of physical activity on the maintenance of musculoskeletal health . However, the significance of the type of exercise and the exercise techniques on bone mass were investigated in recent decades, and the studies have added further information. Before 1980, spinal flexion exercises were popular for managing back pain related to vertebral fractures. The possible logic behind prescribing spinal flexion exercises was to stretch the paraspinal muscles that are in painful cocontraction while guarding the painful, fractured vertebral bodies . Flexing the spine might have made scientific sense initially, but considering that these exercises flexed and compressed the osteoporotic spine, which was already biomechanically compromised, made no common sense. The clinical study, which was conducted to clarify the investigators’ clinical impression, supported the fact that flexion of the osteoporotic spine would result in more vertebral compressions or fractures ( Fig. 4 ) . In this study, 59 women aged 49 to 60 years (mean age, 56 years) with postmenopausal spinal osteoporosis and back pain were divided into four groups. One group performed spinal extension exercises (not hyperextension), one group performed spinal flexion exercises, one group performed a combination of spinal extension and flexion exercises, and one group received only heat and massage with no prescribed exercise. All groups received instructions for proper posture principles. Follow-up time varied from 1 to 6 years (means for the groups, 1.4–2 years) dependent on the occurrence of increased back pain, which indicated a need for follow-up radiographic evaluation. The extension group had a longer period before follow-up. All subjects underwent spine radiographic studies before initiation of the treatment program and at follow-up, when any further wedging or compression fractures, or both, were recorded. Comparisons of the baseline and follow-up radiographs showed additional fractures in 16% of subjects in the extension group, 89% in the flexion group, 53% in the extension and flexion group, and 67% in the group that had no prescribed exercises for treatment and was provided only heat and massage (see Fig. 4 ).
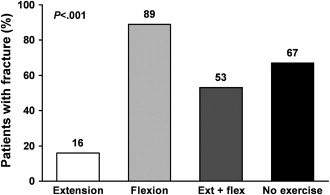
The difference between the spinal extension and spinal flexion groups was most significant ( P <.001). The P values were also significant for the extension group versus the extension and flexion group ( P <.01) and for the extension group versus the no-exercise group ( P <.01). The result of this study was so surprisingly supportive of the author’s clinical impression that exposing the osteoporotic spine to flexion exercises in a prospective study seemed unethical. Flexion of the spine has also been shown to increase intradiskal pressure , which can be transmitted to osteoporotic vertebral bodies anteriorly and result in vertebral wedging and fracture.
The conclusion that physical activity affects bone has been reported repeatedly; however, not all exercises affect bone and muscle in the same way. Osteogenicity depends on the type, intensity, and duration of the exercise performed. In addition, the type of exercise must differ according to the various spinal deformities or skeletal challenges.
Reducing the risk for vertebral fractures without increasing bone mass
In one study, the author and colleagues showed that bone mineral density of vertebral bodies and back strength were correlated . Later, however, they found that resistive exercises that did not load the spine vertically could not increase the vertebral bone mass, although back extensor strength increased significantly ( Fig. 5 ) . Initially, the lack of increase in bone mineral density was disappointing, but they later learned that the long-term effect of these exercises was very promising and effective in reducing the risk for vertebral fractures . Exercise can affect not only bone mass and muscle strength but also vertebral structure and the horizontal trabeculae, which may individually reduce the risk for vertebral fractures .







