CHAPTER 41 Recognition and management of combined instability and rotator cuff tears
 The incidence of a concomitant rotator cuff tear after shoulder dislocation increases with increasing age beyond the age of 40 years. In contrast, the incidence of the classic Bankart lesion decreases.
The incidence of a concomitant rotator cuff tear after shoulder dislocation increases with increasing age beyond the age of 40 years. In contrast, the incidence of the classic Bankart lesion decreases. In elderly patients affected by a concomitant rotator cuff tear, the risk of redislocation is estimated by the individual injury pattern more effectively than by the patient age.
In elderly patients affected by a concomitant rotator cuff tear, the risk of redislocation is estimated by the individual injury pattern more effectively than by the patient age. Nonoperative treatment should be limited to asymptomatic (partial) rotator cuff tears and nondisplaced avulsion fractures of the greater tuberosity.
Nonoperative treatment should be limited to asymptomatic (partial) rotator cuff tears and nondisplaced avulsion fractures of the greater tuberosity. A subjective instability in combination with a capsulolabral or glenoid lesion displays an indication for a surgical stabilization additive to the rotator cuff repair, especially in young patients with a high activity level.
A subjective instability in combination with a capsulolabral or glenoid lesion displays an indication for a surgical stabilization additive to the rotator cuff repair, especially in young patients with a high activity level. In patients between 40 and 70 years of age, the repair of a symptomatic rotator cuff tear should be performed as the essential procedure. The need for additional stabilization surgery is based on the intra-articular injury pattern and on the criterion of first-time dislocation versus chronic instability. Although first-time dislocations of an isolated reconstruction of the rotator can be effective, recurrences should be treated by an additional anterior capsulolabral or bony repair.
In patients between 40 and 70 years of age, the repair of a symptomatic rotator cuff tear should be performed as the essential procedure. The need for additional stabilization surgery is based on the intra-articular injury pattern and on the criterion of first-time dislocation versus chronic instability. Although first-time dislocations of an isolated reconstruction of the rotator can be effective, recurrences should be treated by an additional anterior capsulolabral or bony repair.Introduction
In general, two types of rotator cuff lesions can occur in the course of a traumatic shoulder dislocation: partial articular surface tears or full-thickness tears. In patients younger than 40 years of age and adolescents, a partial articular surface rotator cuff tear is more common than a full-thickness tear.1 Partial articular surface tears have been described by Itoi et al as a consequence of glenohumeral dislocation.2 Hintermann et al found these tears in 16% of the patients who sustained at least one traumatic shoulder dislocation (mean age: 35 years).1 A substantially higher incidence of 56% was verified in patients of various ages after first-time dislocation by Gleyze et al.3
In contrast, the incidence of full-thickness tears after first-time dislocation in young patients is described as low as 9% (mean age: 24 years).4 Even in the case of chronic instability, the incidence of a full-thickness tear in this age group only slightly increases up to 12%.4
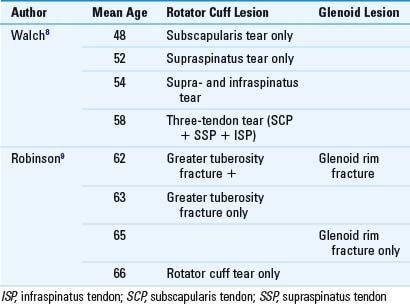
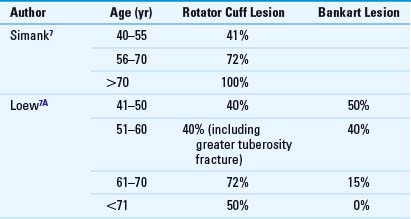
However, the risk of a full-thickness rotator cuff tear after shoulder dislocation is significantly higher in elderly patients (>40 years), with an incidence up to 85%.5,6 This may be explained by the reduced tendon elasticity of the rotator cuff due to age-related collagen degeneration. McLaughlin therefore arbitrarily categorized patients younger than 40 years as “low risk” and patients older than 40 years as “high risk” for instability-associated, full-thickness rotator cuff tears. As a rule, the incidence of full-thickness tears increases with increasing age beyond the age of 40 years, while the risk of a capsulolabral lesion decreases (Table 41-1). Thus, not only the incidence of rotator cuff tears but also their extent and localization have been supposed to be age-related (Table 41-2).
Table 41-1 Age-Related Incidence of a Rotator Cuff Lesion and a Bankart Lesion After Traumatic First-Time Dislocation
Pathomechanism
The question whether a rotator cuff lesion is the result of or the reason for a glenohumeral dislocation has not been answered definitively. McLaughlin stated, that an anterior dislocation of the humeral head from the glenoid requires a disruption of either the anterior (capsule, labrum, glenohumeral ligaments) or posterior (rotator cuff) stabilizing structures.10 Therefore, two different idealized mechanisms help explain the different injury pattern of young and elderly patients: The anterior mechanism of young patients and the posterior mechanism of elderly patients.
Anterior mechanism
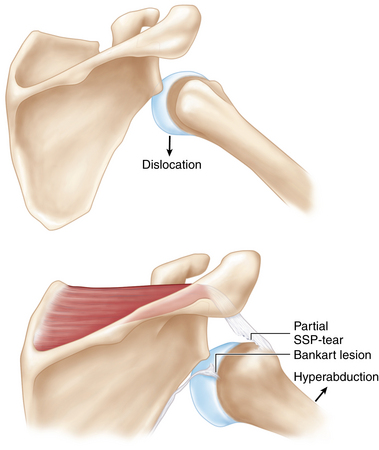
In the course of a traumatic anterior dislocation, young patients typically sustain an injury of the anterior labrum or the capsuloligamentous structures. Thereby the rotator cuff muscles react to the sudden eccentric load with a reflexive contraction that causes a distension of the rotator cuff tendons. The distension of the rotator cuff results in a shearing-off of the tendon insertion in the dislocation position (Fig. 41-1). This mechanism can result in a partial or complete tear of the rotator cuff.10
Posterior mechanism
The posterior mechanism of the elderly patient is based on a preexisting degeneration of the rotator cuff tendons. The posterosuperior rotator cuff (supraspinatus, infraspinatus) is known to be an essential dynamic stabilizer of the humeral head against excessive anterior translation. In the case of a traumatic anterior dislocation, the sudden tensile load results in a rupture of the weakened tendon insertion, whereas the anterior glenoid labrum typically remains intact.11 A possible redislocation that is rare in this patient group might be explained by the torn posterosuperior rotator cuff.
A predominance of the posterior mechanism in patients between 40 and 60 years is supported by Porcellini et al, who found a strong correlation between the increasing number of recurrences and the development of a posterosuperior rotator cuff tear.12 In contrast, a Bankart or capsular tear did not appear to be closely related to the number of dislocations in this age group.
Redislocation risk
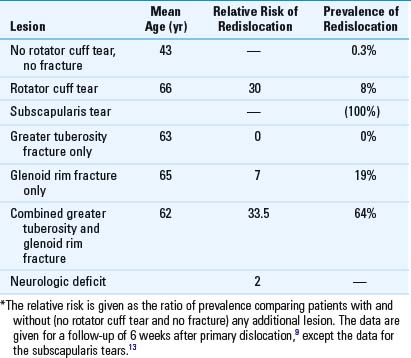
It is generally accepted that the risk of a redislocation after traumatic first-time dislocation decreases with increasing patient age. In contrast to this age-related correlation for younger patients (<40 years), the individual injury pattern seems to be more important in middle-aged and elderly patients. With regard to the prognostic recurrence risk, the following key lesions have been shown to be primarily relevant (Table 41-3):
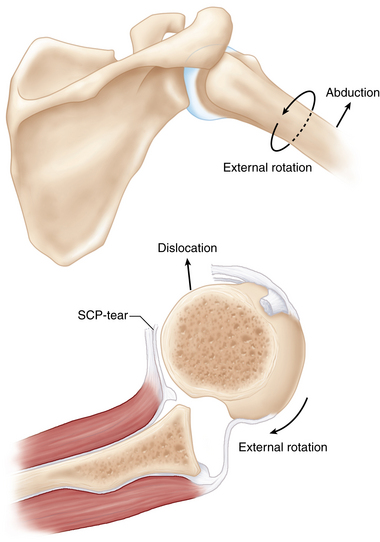
Thus, a full-thickness tear of the rotator cuff increases the risk of redislocation by a factor of 30. The prevalence of a redislocation in those patients is given by 8.3% compared with 0.3% if no rotator cuff tear is evident (see Table 41-3).9 Walch et al found 77% of the patients presenting with a recurrent dislocation after the age of 40 to have a rotator cuff tear.8 Furthermore, Porcellini et al revealed a strong correlation between the rising number of dislocations and associated full-thickness tears of the supraspinatus and infraspinatus tendon.12 In the category of full-thickness tears, a rupture of the subscapularis tendon by a combined abduction and external rotation mechanism seems to be particularly crucial. In these cases, the external rotation force results in a subscapularis tendon rupture, while the anterior shear force by the humeral head causes a Bankart lesion (Fig. 41-2). Neviaser et al reported all patients older than 60 years of age with an anterior redislocation to have a complete subscapularis tear and a rupture of the anterior capsule.13
In contrast to a full-thickness tear of the rotator cuff, an avulsion fracture of the greater tuberosity does not increase the prevalence of a redislocation but rather reduces it compared with the overall patient population.9 This relationship was initially described by Hovelius et al, who reported a redislocation rate of 0% after a fracture of the greater tuberosity compared with a risk of 32% in patients without this fracture.14 Therefore, this lesion seems to provide a “protective effect” against recurrent dislocation. However, this rule is strictly limited to isolated fractures of the greater tuberosity. If the greater tuberosity fracture is contrariwise accompanied by a glenoid rim fracture, such a bifocal lesion must be interpreted as a result of a high energy injury. Those lesions have been described with an excessively high prevalence of redislocation (64%).9
If the first-time dislocation is accompanied by an isolated glenoid rim fracture, the prevalence of a redislocation is increased up to 19%. While the standard Bankart lesion is rare in elderly patients, glenoid rim fractures have been detected with an incidence of between 8% and 23%.15 Jouve et al found an even higher incidence of bony Bankart lesions accompanied by a rotator cuff tear in 54% of the patients (mean age: 47 years).16 The authors stated that in those patients the recurrent instability was clearly influenced by the “anterior mechanism” resulting from the glenoid lesion.
In addition to the structural lesions of the dynamic and static stabilizers, the risk of recurrent dislocation is influenced by an axillary nerve or brachial plexus injury. In these patients, the relative risk of recurrent dislocation is reported to be two times higher compared with patients without any neurologic deficit.9
Axillary nerve injury: terrible triad
In the course of a traumatic rotator cuff lesion accompanied by shoulder dislocation, an additional axillary nerve injury can easily be missed if the resulting weakness is assumed to be caused by the rotator cuff tear alone. Therefore, a combined neurologic and structural injury pattern must be suspected if a global weakness is evident after reposition. A triple lesion that includes traumatic dislocation, rotator cuff tear, and an injury to the brachial plexus branches was defined by Groh and Rockwood as the terrible triad of the shoulder.17
In the course of glenohumeral dislocation, a lesion of the axillary nerve is supposed to be caused by either a direct compression mechanism of the humeral head or by a traction mechanism of the nerve in the posterior axillary gap. The incidence of axillary nerve injuries after anterior shoulder dislocation is given as 7% to 18%.5,18 Irreversible lesions are rare. Most of the nerve injuries are remittent after a posttraumatic interval between 3 to 24 months.19,20 Regarding the age-related incidence, Gumina et al found an axillary nerve palsy in 9.3% of the patients older than 60 years of age.19
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree