CHAPTER 8 Radiographic studies and findings
 The treatment of instability requires precise identification of the underlying lesion through clinical examination and diagnostic imaging.
The treatment of instability requires precise identification of the underlying lesion through clinical examination and diagnostic imaging. Visualization and treatment of any associated lesions are essential because the lesions are often associated with pain and poor outcomes.
Visualization and treatment of any associated lesions are essential because the lesions are often associated with pain and poor outcomes. The diagnosis of shoulder instability involves a workup that begins with plain x-rays and is completed with magnetic resonance imaging or magnetic resonance arthrography.
The diagnosis of shoulder instability involves a workup that begins with plain x-rays and is completed with magnetic resonance imaging or magnetic resonance arthrography.Imaging evaluation
Plain x-rays
Standard anteroposterior view
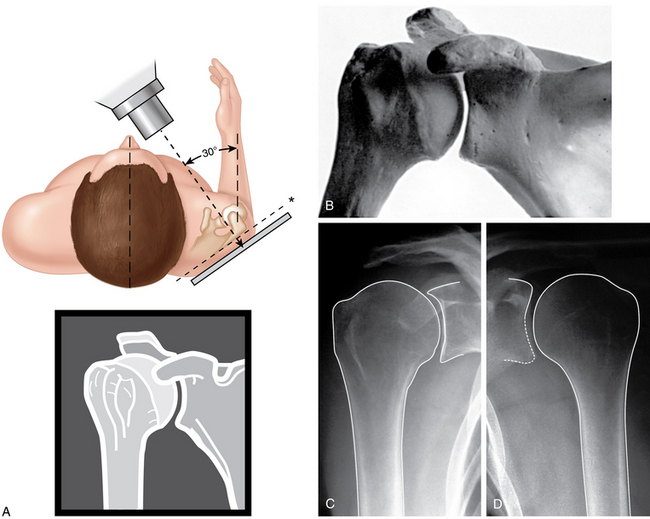
The standard AP view is an oblique view in which the humeral head and the glenoid partially overlap because of the anterior tilt (approximately 40 degrees) of the beam directed toward the humeral head. This view can be obtained in internal and external rotation to demonstrate a Hill-Sachs lesion (Fig. 8-1).
True anteroposterior (grashey) view
The beam directed lateral to the scapula (45 degrees) affords optimal visualization of the glenohumeral (GH) joint, with the overlying anterior and posterior glenoid rim highlighting the joint line. This view clearly demonstrates any erosion of the anterior glenoid rim that fails to be depicted (Fig. 8-2).
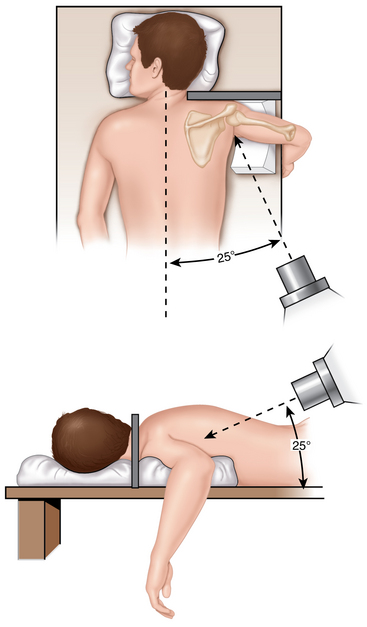
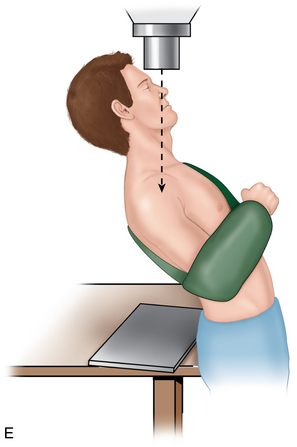
Stryker notch view (fig. 8-4)
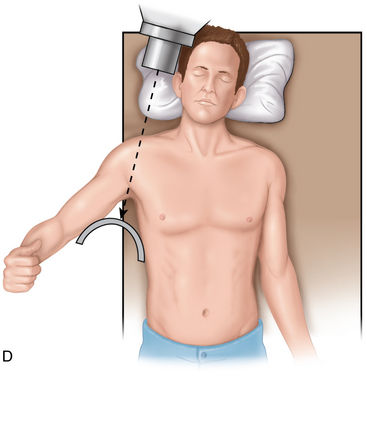
This variant of the AP view is obtained with the patient lying supine, the arm abducted and externally rotated and the palm behind the head. The beam has approximately 10 degrees of cephalic inclination to display the posterolateral humeral head and document Hill-Sachs fractures. The Stryker notch view is important to help with evaluation of humeral head Hill-Sachs lesions. In addition, an internal rotation view also may be helpful to visualize Hill-Sachs injuries (Fig. 8-4, D).
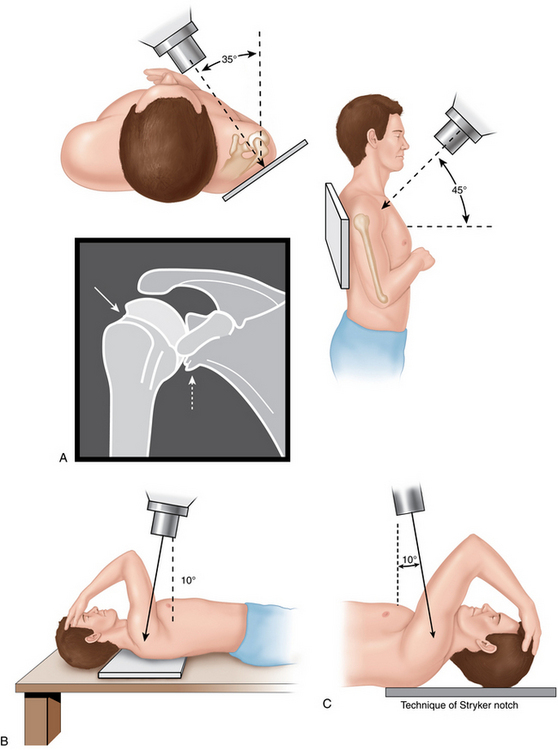
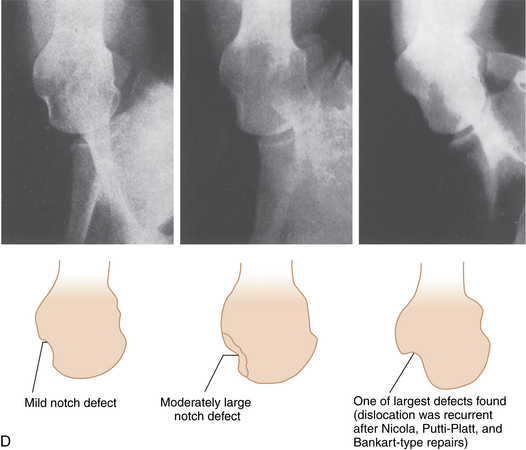
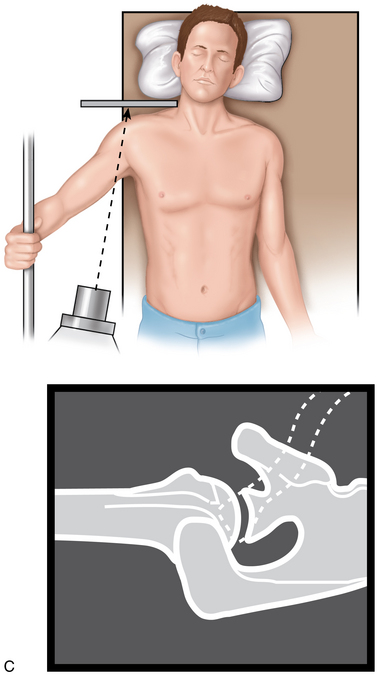
FIGURE 8-4 A, Apical oblique view. The shoulder is positioned as for an anteroposterior view in the plane of the scapula except that the x-ray beam is angled inferiorly at an angle of 45 degrees. This reveals the contour of the posterolateral humeral head and the anteroinferior glenoid. Solid arrow indicates Hill-Sachs defect. Dashed arrow indicates anteroinferior glenoid defect. B, Stryker notch view. C, Position of the patient for the Stryker notch view. The Stryker notch view is helpful for identification of humeral head bony injuries. The patient is supine with the cassette posterior to the shoulder. The humerus is flexed approximately 120 degrees so that the hand can be placed on top of the patient’s head. Note that the angle of the x-ray tube is 10 degrees superior. D, Defects in the posterolateral aspect of the humeral head are seen in three different patients with recurring anterior dislocations of the shoulder.
(A redrawn from Matsen FA, III, et al: Shoulder surgery: Principles and procedures, Philadelphia, 2004, WB Saunders, p 12. B redrawn from Hall RH, et al: Dislocations of the shoulder with special reference to accompanying small fractures. J Bone Joint Surg Am 41:489–494, 1959. C and D modified from the work of Hall RH, et al: Dislocation of the shoulder with special reference to accompanying small fractures. J Bone Joint Surg Am 41:489–494, 1959; appearing in Rockwood CA, et al: The shoulder, ed 4, Philadelphia, 2009, Saunders Elsevier, p 187.)
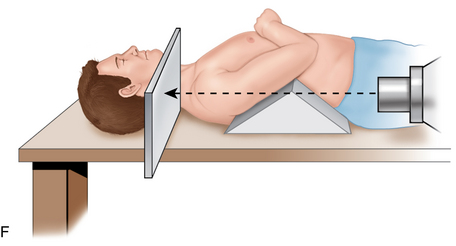
Axillary view (fig. 8-5)
The beam is directed toward the axillary cavity, with a medial tilt of approximately 15 degrees, and the arm is abducted. It depicts any anterior glenoid rim bone fragments, which may be related to a bony Bankart lesion, and erosion of the anteroinferior portion of the glenoid rim (see Fig. 8-5, C).
Considerations
The true AP view affords diagnosis of superior subluxation and of other lesions of the acromioclavicular joint, collarbone, and ribs, as well as of glenoid hypoplasia, a rare congenital condition involving absence or marked reduction of the glenoid neck. Glenoid hypoplasia is often associated with recurrent dislocation; hence, there is x-ray evidence of GH arthritis, bone spurs, and intra-articular loose bodies. When excessive glenoid retroversion with respect to the humerus is the suspected cause of instability, a CT scan is the most informative examination. Finally, a ganglion cyst at the level of the lower glenoid region may be associated with pain and GH joint dislocation. In such cases, the frequent clinical finding of supraspinatus and infraspinatus hypotrophy is well documented on MRI. In overhead and thrower athletes, such as baseball pitchers, plain films can demonstrate specific lesions such as Bennett lesion, which involves a bony spur on the posterior-inferior surface of the glenoid. When Bennett first described it, in 1941, he attributed spur formation to traction of the brachial triceps on the infraglenoid tubercle and suggested a dedicated view with the beam tilted 5 degrees cephalad and the arm in 90 degrees of abduction and 90 degrees of external rotation. In fact, this lesion is due to ossification of the posterior band of the inferior glenohumeral ligament (IGHL), and the bone spur is due to the impact of the humeral head on the posterior glenoid with each throwing movement.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree