CHAPTER 14 Radiographic and arthroscopic evaluation of glenoid and humeral head bone loss
 Glenoid bone loss is likely the number one factor responsible for failure and recurrence after a shoulder instability repair.
Glenoid bone loss is likely the number one factor responsible for failure and recurrence after a shoulder instability repair. Nearly all patients with traumatic, recurrent anterior instability have some level of glenoid bone loss. It is paramount to recognize the amount of bone loss preoperatively in order to clearly delineate successful management strategies.
Nearly all patients with traumatic, recurrent anterior instability have some level of glenoid bone loss. It is paramount to recognize the amount of bone loss preoperatively in order to clearly delineate successful management strategies. Standard radiographs may be inadequate for detecting the extent of glenoid and humeral head bone loss.
Standard radiographs may be inadequate for detecting the extent of glenoid and humeral head bone loss. Initial plain film radiographic evaluation of the shoulder should include an anteroposterior (AP) view, a Grashey (true AP) projection view, an axillary view, and a scapulolateral Y view.
Initial plain film radiographic evaluation of the shoulder should include an anteroposterior (AP) view, a Grashey (true AP) projection view, an axillary view, and a scapulolateral Y view. Glenoid fractures and fragments should be distinguished from attritional glenoid bone loss in which the injured portion of glenoid bone has resorbed.
Glenoid fractures and fragments should be distinguished from attritional glenoid bone loss in which the injured portion of glenoid bone has resorbed. The AP view with internal rotation and Stryker notch view can be used to assess the posterolateral aspect of the humeral head, a typical location for Hill-Sachs lesions.
The AP view with internal rotation and Stryker notch view can be used to assess the posterolateral aspect of the humeral head, a typical location for Hill-Sachs lesions. Three-dimensional computed tomography (CT) and magnetic resonance imaging (MRI) are useful methods for quantitative assessment of glenoid bone loss. Estimating bone loss can be done using a variety of methods, including the true circle method, the linear method, or variations on these techniques.
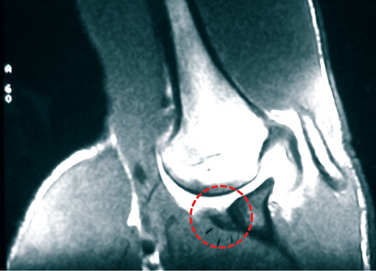
Three-dimensional computed tomography (CT) and magnetic resonance imaging (MRI) are useful methods for quantitative assessment of glenoid bone loss. Estimating bone loss can be done using a variety of methods, including the true circle method, the linear method, or variations on these techniques. MRI is an accurate method for identifying subtle lesions of the humeral head and can be used for grading Hill-Sachs lesions with methods described by various authors.
MRI is an accurate method for identifying subtle lesions of the humeral head and can be used for grading Hill-Sachs lesions with methods described by various authors. Diagnostic arthroscopy may be helpful for confirmation of pathology, quantification of osseous defects, and assessment of associated structures. Using a calibrated arthroscopic measurement probe and various geometric techniques, quantification of glenoid bone loss can be achieved using simple mathematics.
Diagnostic arthroscopy may be helpful for confirmation of pathology, quantification of osseous defects, and assessment of associated structures. Using a calibrated arthroscopic measurement probe and various geometric techniques, quantification of glenoid bone loss can be achieved using simple mathematics.Introduction
Stability in the glenohumeral joint is dependent on numerous restraint mechanisms, including the constraining bony articulation and a complex array of dynamic and static mechanisms that center the humeral head on the glenoid fossa. Shoulder instability, often instigated by trauma, frequently results in bony injury to the glenoid and/or humeral head. As described by Howell et al,1 the glenoid articular surface combines with the labrum to create a socket that is approximately 9 mm deep in the superoinferior direction and only 5 mm deep in the anteroposterior (AP) direction. After initial traumatic dislocation, articular constraints in the AP direction may be compromised, effectively reducing the socket depth. With decreased constraints, the shoulder is subject to recurrent instability, thereby perpetuating the cycle.
The most common defect seen after traumatic anterior dislocation of the shoulder is an anteroinferior capsulolabral avulsion, also termed a Bankart lesion.2 When accompanied by a comparable fracture in the glenoid rim, the term bony Bankart lesion is frequently used. It should be noted that a bony Bankart injury is much different than a Bankart tear alone, a soft tissue injury in which there is no bone injury to the glenoid. Although true incidence of bony Bankart lesions is often debated, reports in the literature suggest that glenoid bone injuries occur in up to 22% of first-time anterior shoulder dislocations and up to 90% of patients with recurrent instability.3,4 In the acute (<3 months) setting, individuals with traumatic anterior shoulder dislocation may have identifiable glenoid rim fracture fragments identifiable with diagnostic arthroscopy.5,6 As shoulder instability begins to take on a more chronic course (>6 months), fracture fragments may begin to show signs of partial resorption7 and glenoid osseous lesions may develop, progress, or remodel secondary to recurrent dislocation.
Like the glenoid, the humeral head also may demonstrate osseous pathology after traumatic anterior dislocation. Osteochondral defects in the humeral head, often referred to as Hill-Sachs lesions, are commonly found on the posterolateral region where the soft base of the humeral head impacts against a relatively hard anterior glenoid. They are caused by a compression fracture that forms when the humeral head is displaced anteriorly, inferiorly, and medially during traumatic dislocation. Hill-Sachs lesions can be formed during the initial anterior shoulder dislocation or any subsequent episode thereafter. It has been reported that almost half of all initial anterior shoulder dislocations are accompanied by some level of Hill-Sachs lesion.8 Such osteochondral lesions often play a fundamental role in recurrent shoulder instability by decreasing the humeral head’s contribution to passive stability. As described by Burkhart,9 the phenomenon of articular arc length mismatch occurs with a unique subset of large Hill-Sachs lesions when patients abduct and externally rotate the arm. This position brings the flattened Hill-Sachs lesion in contact with the anterior glenoid rim, thereby causing the rim to “drop into” and “engage” the Hill-Sachs lesion.
To better assess glenoid bone loss, the apical oblique view of Garth,10 the West Point view,11 and the Didiée view12 are often used; all three involve shooting the radiographic beam at an angle relative to the glenoid face. For humeral head osseous pathology, an anteroposterior (AP) view with internal rotation and a Stryker notch view12 also may be beneficial.
Additional imaging modalities such as computed tomography (CT), magnetic resonance imaging (MRI), and magnetic resonance arthrography (MRA) also can be used to obtain 3-dimensional (3-D) representations of the glenoid; these often are valuable for preoperative planning. Humeral head defects can be measured using MRI, which is useful for evaluation of nearby structures that may contribute to instability. Grading of Hill-Sachs lesions has been described in articles published by Rowe et al,13 Franceschi et al,14 Flatow et al,15 Hall et al,16 and Richards et al.17
Plain radiographic evaluation
Initial plain film radiographic evaluation of the shoulder should include an AP view, a “true” AP view in the plane of the scapula (also termed the Grashey projection), an axillary view, and a scapulolateral Y view. A standard AP view of the shoulder is useful for visualizing the glenohumeral joint with respect to the clavicle, acromion, scapular body, upper ribs, and adjacent soft tissues. This view also is useful for demonstrating unexpected pathology, including dislocation, arthritis, abnormal calcifications, or tumors. To perform the “true” AP view of the shoulder, a cassette is placed on a flat surface directly behind the affected shoulder. The patient then turns the affected shoulder out 35 to 40 degrees, thereby placing the posterior aspect of the shoulder directly on the cassette; this places the cassette parallel to the scapular plane. An x-ray beam is then shot perpendicularly to the cassette, directly tangential to the glenohumeral joint, allowing visualization of joint space abnormalities and humeral head positioning. An AP view is often differentiated from a “true” AP shoulder view by assessing the glenohumeral joint. The Grashey projection, because it is shot in the plane of the scapula, does not demonstrate any overlap of the humerus and glenoid; a standard AP view, in contrast, will show a convex lens shaped overlap between the humeral head and the posterior rim of the glenoid. The Grashey view frequently is adept at detecting subtle subluxation in the superoinferior direction: simply compare the center of the humeral head with the center of the glenoid fossa. Subluxation also may be suggested with the presence of asymmetric joint space widening in the glenohumeral joint; this finding, however, also can be caused by a cartilage defect. Stress views are frequently employed to accentuate subtle subluxation patterns.
Glenoid bone loss
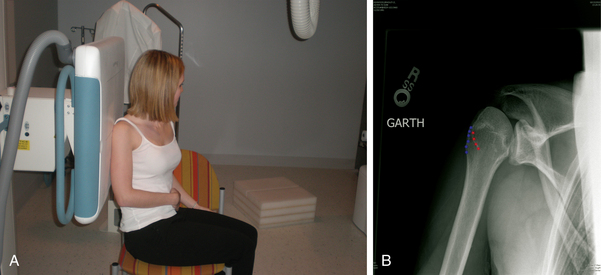
The apical oblique view or Garth view is most useful for optimizing visualization of Bankart fractures on the anteroinferior glenoid rim, calcifications, and impression fractures on the posterior margin of the superolateral humeral head following dislocation (Fig. 14-1). Additionally, since the arm does not have to be manipulated more than slightly, it is extremely useful in the setting of acute trauma. The view is performed by having the patient sit with their arm in their lap. An x-ray cassette is positioned flat against the scapula on the affected side, similarly to the Grashey projection. The x-ray beam is centered on the coracoid process, perpendicular to the cassette, except that it is angled 45 degrees caudally off the AP glenohumeral view, such that the beam becomes tangential to the anteroinferior aspect of the glenoid rim.
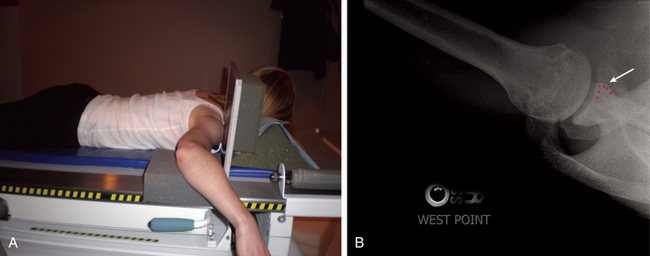
The West Point view, in contrast, is a variation of the standard axillary view. Like the apical view, it creates a tangential view of the anteroinferior rim of the glenoid, thereby improving detection of bony Bankart lesions. The West Point view is often felt to be the best evaluation for osseous pathology of the anterior glenoid. Accurate patient positioning, however, may be tough for patients recently experiencing shoulder injury. To perform the West Point view, the patient is placed in a prone position on the x-ray table while the injured shoulder is abducted 90 degrees and placed on a pad raised 7.5 cm from the top of the table. The head and neck are turned away from the involved side while a cassette is placed on the superior aspect of the involved shoulder (Fig. 14-2). The x-ray beam is centered at the axilla and directed from distal to proximal while being angulated 25 degrees medially and 25 degrees anteriorly.
The Didiée view, like the West Point view, is obtained with the patient prone on the x-ray table (Fig. 14-3). It is used to enhance visualization of fractures, degenerative changes, calcifications, loose bodies and malalignment in and around the glenohumeral joint. To perform, the arm is abducted and the forearm is positioned posterior to the trunk while the dorsum of the hand rests on the iliac crest, thumb pointing upward. A 3-inch pad can be placed under the elbow. In this position, the humeral shaft is parallel to the table and perpendicular to the vertical transcondylar axis. The beam is directed from a position centered on the humeral head directly lateral to the glenohumeral joint and angled 45 degrees to the floor.
Humeral head bone loss
In addition to the Garth and West Point views, humeral head bone loss also can be assessed using an AP view with internal rotation and the Stryker notch view. The AP with internal rotation view is shot with the patient either standing (Fig. 14-4) or in the supine position with a pad positioned under the elbow. The arm is abducted and internally rotated 45 degrees with the forearm lying across the patient’s abdomen so that the humerus is parallel to the table. The beam is rotated 15 degrees caudally and positioned over the humeral head, allowing improved visualization of the posterolateral aspect of the humeral head.
Perhaps the best radiographic view for identifying humeral head bone loss after traumatic anterior dislocation—namely Hill-Sachs lesions—is the Stryker notch view. In a prospective study of 27 shoulders with recurrent anterior dislocation, Rozing et al found the Stryker-notch view to adequately demonstrate Hill-Sachs lesions in 92.6% of shoulders.18 Additionally, the authors also found it to be of high diagnostic yield in detecting Bankart lesions. To perform the Stryker notch view, the patient is positioned supine, and the elbow of the affected shoulder is placed above the head, pointing forward; the hand should be palm down on the top of the head with fingers oriented posteriorly. An x-ray plate is placed directly under the shoulder, and the beam is shot cephalad at a 45-degree angle directly on the coracoid process (Fig. 14-5). This view also can be obtained with the patient erect by using a swivel arm x-ray system. The hand is placed on top of their head with their fingers pointed toward the back of the head. The beam is directed anteroposteriorly with 10 degrees of cephalic angulation. In this position, evaluation of subluxation and glenoid rim fractures is limited to the oblique orientation of the glenohumeral joint. However, the resulting image exposes the posterolateral aspect of the humeral head, thereby improving detection of Hill-Sachs lesions.
Radiographic measurement
Glenoid bone loss
Determination of the amount of bone loss on the glenoid is imperative to preoperative discussions and planning in patients with recurrent instability. This is due to the finding that in those patients with anterior instability and glenoid bone loss, around 20% to 25% have diminished results and a higher chance of recurrent instability after repair.19 Also, those with attritional glenoid bone loss (resorption of the glenoid bone fragment) may be at an even higher risk of failure after instability repair19 (Fig. 14-6). It should be kept in mind that the bony glenoid does not tolerate loss too well, and that a 20% to 25% loss may only be a 6- to 8-mm osseous defect in the anteroinferior glenoid. Thus, it is imperative to determine precisely the amount of glenoid bone loss in order to fully educate your patient on expected outcomes and determine the optimal treatment plan (i.e., arthroscopic versus open repair or bone augmentation procedures).
Plain radiographs, two-dimensional (2-D) MRI, and 2-D CT have proven to be effective for detecting the presence of glenoid bone loss and newly formed glenoid rim fracture fragments20 (Fig. 14-7). However, as a result of the natural three-dimensional (3-D) structure of the glenoid in combination with the variance in glenoid version, these methods may be inadequate for quantifying glenoid bone loss. In standard 2-D CT, the amount of glenoid version affects the gantry angle needed to gain an accurate representation of the glenoid. The beam must be precisely perpendicular to the long axis of the glenoid, and the glenoid must be in a fixed position. Two-dimensional scanning methods also make it difficult to precisely identify the superior tip of the glenoid, especially when viewed in the sagittal plane.
MRA is also useful in cases of glenohumeral instability because of its capacity to distend the joint, outline capsular and labral structures, and show cartilage lesions on both the humeral head and the glenoid. MRA is more costly, time intensive, and invasive than standard MRI, but it is frequently used in situations with suspected shoulder instability, ligamentous lesions, or anterior labrum periosteal sleeve avulsion (ALPSA). An ALPSA lesion—tear of the anteroinferior labrum without rupture of the anterior scapular periosteum—is important to identify preoperatively because surgical treatment is different from Bankart repair. Additionally, patients with anterior shoulder instability and concomitant ALPSA type lesion have two times greater bone loss at time of surgery as compared with those with anterior instability alone.21 Shoulder stabilizing procedures may have a higher predisposition to failure in this population. ALPSA lesions are best identified on axial MRA and appear as a small cleft or margin between the anterior labrum and the glenoid.
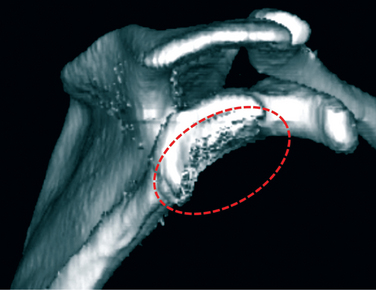
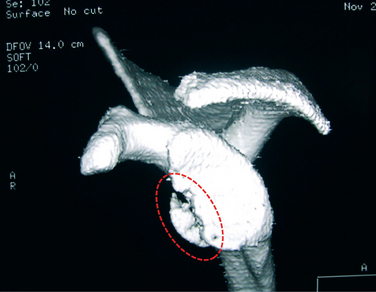
Quantitative evaluation of bone loss is best performed preoperatively using 3-D CT, 3-D MRI, or MRA. Three-dimensional CT allows for the digital subtraction of the humeral head from images of the glenohumeral complex, thereby facilitating analysis of the scapula as a free body (Fig. 14-8). The net result is an accurate anatomic depiction of the glenoid, glenoid surface, and vault.22 Indications for obtaining a 3-D CT scan in patients with shoulder instability are described in Table 14-1.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree