Radial Head and Neck Fractures
CASE PRESENTATION
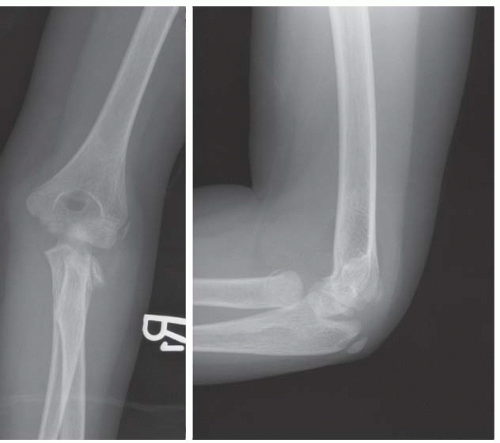
An 8-year-old female presents with right elbow pain after a fall from standing height. There is tenderness and swelling over the lateral elbow, and she is reluctant to flex-extend the elbow or rotate the forearm. Radiographs demonstrate a radial neck fracture (Figure 31-1).
CLINICAL QUESTIONS
How do children with radial neck and head fractures present?
How are radial neck and head fractures classified?
What are the treatment principles for radial neck and head fractures?
What are the indications for surgical reduction and fixation?
What surgical techniques are used?
What are the anticipated results and possible complications of surgical treatment?
THE FUNDAMENTALS
Radial neck fractures are relatively common injuries in the skeletally immature patient. While the diagnosis is often easily made, fractures of the proximal radius continue to present the pediatric hand and upper extremity surgeon with a host of clinical challenges due to (1) the controversies regarding what constitutes acceptable deformity; (2) the myriad of surgical treatment options; and (3) the propensity for these injuries to cause persistent elbow stiffness or late complications, despite seemingly acceptable radiographic alignment. In general, treatment is predicated on restoring anatomy and thus elbow/forearm motion using the least invasive means possible.
Etiology and Epidemiology
Proximal radius fractures represent approximately 1% of all childhood fractures and account for roughly 5% to 10% of all elbow injuries.1, 2, 3, 4, 5 and 6 Typically affecting children between 4 and 14 years of age, the peak age for radial neck and head fractures is between 8 and 10 years.1,3,7, 8, 9, 10 and 11 Unlike adult proximal radius fractures, which affect the radial head and are often intra-articular, pediatric fractures typically involve the neck and traverse the proximal radial physis or metaphysis. It is believed that the cartilaginous nature of the epiphysis is more resistant to fracture and confers a relative protective effect.
Radial head and neck fractures can occur in association with other elbow region injuries. Lateral compression (radial head/neck, lateral condyle), medial tension (medial epicondyle, medial collateral ligament), anterior tension (brachialis muscle, coronoid, anterior capsule), and posterior compression (olecranon) can all occur together. These more complex injuries require treatment for each injury as a part of the care package.
Clinical Evaluation
If size is all that matters, how come the whale is endangered and the ant continues to do just fine?
—Kelly Marshall
Patients will typically present with pain, swelling, and limited elbow and forearm range of motion. Physical examination will yield tenderness with palpation over the radial neck, with resistance to passive forearm rotation in displaced injuries.
Radiographic evaluation includes standard anteroposterior (AP) and lateral plain radiographs of the elbow. As the proximal radial epiphysis does not become radiographically apparent until approximately 3 to 4 years of age, radiographic evaluation of radial neck fractures may be challenging in the very young child. Furthermore, it is important to remember that normally the proximal radius has up to 15 degrees of valgus angulation on the AP view and between 10 degrees of anterior to 5 degrees posterior angulation as seen on the lateral projection.11 Careful inspection of the contour and alignment of the proximal radial metaphysis is needed to discern injuries in these young patients. The 45-degree oblique view may be helpful in separating the radial and ulnar structures on plain radiographs to better identify and
characterize the radial neck fracture.12, 13 and 14 Furthermore, as radial neck fractures are frequently associated with elbow dislocations and other fractures about the elbow, systematic inspection of all the bony structures is needed to rule out concomitant skeletal injuries.
characterize the radial neck fracture.12, 13 and 14 Furthermore, as radial neck fractures are frequently associated with elbow dislocations and other fractures about the elbow, systematic inspection of all the bony structures is needed to rule out concomitant skeletal injuries.
Radial neck fractures are primarily classified according to anatomic location, translation, and angulation. These fractures have been further classified according to mechanism of injury and degree of displacement.4,8,15 Group I injuries refer to those with primarily radial head displacement. Group IA fractures include Salter-Harris type I and II fractures, group IB fractures include Salter-Harris type IV fractures, and group IC fractures involve the proximal radial metaphysis. Group ID and IE injuries refer to radial head displacement that occurs during reduction or dislocation of ulnohumeral dislocations, respectively. Group II injuries denote displacement of the radial neck, either with angular (IIA) or torsional (IIB) deformity. Finally, Group III injuries denote stress injuries of the radial head articular surface, epiphysis, or physis (see Coach’s Corner).
Surgical Indications
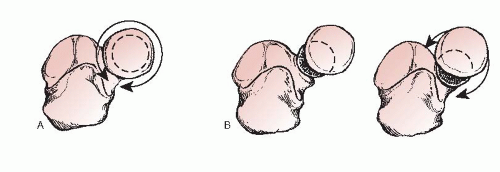
While radial neck fractures have tremendous healing potential, excessive angulation or translation will result in loss of forearm rotation and/or elbow flexion-extension. Much of this is due to the constrained articulation of the proximal radioulnar joint (PRUJ) (Figure 31-2). With angulation or translation of the radial head on the radial shaft, cam impingement may occur, resulting in a bony block to forearm rotation.16 Surgical procedures are therefore intended to restore more normal anatomy in hopes of preserving motion and ultimately upper limb function.
Given these considerations, intervention is recommended for excessive fracture displacement. How much angulation and/or translation constitute “too much” is difficult to answer and has not been rigorously studied. Multiple authorities and retrospective studies have suggested that <30 to 45 degrees of angulation and <3 to 4 mm of translation will allow for acceptable functional results.5, 6, 7 and 8,10,11,17,18 While these radiographic guidelines are helpful, they can be misleading, as often the maximal
deformity is not appreciated on static AP and lateral radiographs of the elbow. Furthermore, radiographic remodeling of proximal radial injuries is poor, and multiple studies have demonstrated that radiographic alignment and elbow/forearm motion plateau after 6 months postinjury.9
deformity is not appreciated on static AP and lateral radiographs of the elbow. Furthermore, radiographic remodeling of proximal radial injuries is poor, and multiple studies have demonstrated that radiographic alignment and elbow/forearm motion plateau after 6 months postinjury.9
We favor observation and nonoperative treatment of most of the radial neck fractures with <30-degree angulation, <4-mm translation, congruent radiocapitellar reduction, and at least 80 degrees of forearm pronation-supination. For all other injuries, the simplest and least invasive method of fracture realignment is attempted to achieve the above-stated criteria. In essence, the question is not which injuries require intervention, but rather, which fractures do not require further reduction.
SURGICAL PROCEDURES
Ain’t no chance if you don’t take it.
—Guy Clark
While a host of surgical procedures can be performed, multiple published studies highlight some common, unifying principles. First, earlier intervention is better.19,20 Fracture reduction becomes much more difficult beyond 7 days postinjury, potentially compromising results. Second, open reduction and fracture stabilization should be deemed a last resort.7,9,21,22 While likely due to selection bias, the literature clearly supports the notion that the need for open reduction portends a worse prognosis. Third, an imperfect but acceptable closed reduction is preferred over an anatomic reduction achieved via open means. Finally, despite surgical skill and radiographic realignment, stiffness does occur, and patients/families should be counseled about the risk of post-traumatic loss of forearm rotation.
In cases where unacceptable alignment and loss of forearm pronation-supination exist, we advocate a stepwise progression of reduction maneuvers, from simple to complex, until a satisfactory clinical and radiographic result is achieved (Table 31.1).
Table 31.1 Progression of treatment options for displaced radial neck fractures | |||||
|---|---|---|---|---|---|
|