Chapter 66 Quadriceps and Patellar Tendon Disruption*
Anatomy
The patellar tendon is primarily derived from the central fibers of the rectus femoris, which extend over the anterior surface of the patella and form a flat tendinous structure that inserts into the tibial tubercle. It continues past the tubercle and blends with the iliotibial band on the anterolateral surface of the tibia. The average length of the patellar tendon is 4.6 cm (range, 3.5 to 5.5).109
Causes of Extensor Mechanism Disruption
Experimental studies have shown that a normal tendon will not rupture when a longitudinal stress is applied but, instead, the disruption will occur at the musculotendinous junction, muscle belly, or tendinous insertion into the bone. It has been shown that the normal quadriceps tendon may be able to tolerate up to 30 kg/mm of longitudinal stress before failing. Patellar and quadriceps tendon ruptures therefore occur through a pathologic area of the tendon. The estimated force required to disrupt the extensor mechanism of the knee is 17.5 times body weight and usually occurs during a sudden eccentric contraction of the extensor mechanism with the foot planted and the knee flexed as the person falls. With this in mind, many pathologic conditions can affect the extensor mechanism, including renal disease, diabetes mellitus, hyperparathyroidism, rheumatoid arthritis, systemic lupus erythematosus, gout, osteomalacia, infection, obesity, steroid use,71,86 and other metabolic diseases. These metabolic diseases cause microscopic damage to the vascular supply to the tendons or alter the architecture of the tendon. Diabetes has been shown to cause arteriosclerotic changes in the tendon vessels, whereas chronic synovitis causes fibrinoid reactions within the tendon. Muscle fiber atrophy secondary to renal disease and uremia will also weaken the tendon. Pathologic changes from advancing age include fatty and cystic degeneration, myxoid degeneration, and calcification, all of which alter tendon architecture. Bone resorption and osteopenia can also occur at the osteotendinous junction with advancing age. A report of spontaneous patellar tendon rupture in identical twins has further supported the concept that predisposing factors for extensor mechanism rupture exist.41 Although quadriceps tendon rupture tends to occur in older patients or those with systemic disease or degenerative changes, patellar tendon rupture or avulsion is more common in patients younger than 40 years.62,120 Most spontaneous ruptures of the quadriceps tendon occur within 1 to 2 cm of the patella through the pathologic areas mentioned, leaving the periosteal attachment intact. This also correlates to the zone of the quadriceps tendon with the poorest vascularity.131 Numerous cases of bilateral extensor mechanism rupture have been reported. Although most ruptures occur in patients with predisposing conditions such as obesity, systemic illness,* and use of anabolic steroids, several reports have noted simultaneous bilateral extensor mechanism rupture in healthy patients without predisposing factors.† In a retrospective review of bilateral and unilateral quadriceps tendon rupture, Konrath and associates60 have noted a significant correlation between bilateral simultaneous rupture and systemic disease.
Iatrogenic conditions that may alter the local properties of the extensor mechanism include total knee arthroplasty (TKA),74 lateral retinacular release,9,29,118 and harvesting of the central third of the patellar tendon for ligament reconstruction.10,64,78 Local steroid injection has similarly been implicated as a cause of tendon rupture. Rupture of the quadriceps tendon has been reported after patellar dislocation.92 Partial patellar tendon rupture may occur with tibiofemoral dislocations.130
Disruption of the extensor mechanism is a significant disabling injury and should be diagnosed early.104,116 Patients usually have an acute onset of knee pain, swelling, and loss of function after a stumble or fall. Although rare, acute compartment syndrome of the thigh secondary to a quadriceps rupture has also been reported.63 The physical examination generally reveals a palpable defect in the quadriceps tendon with a low-lying patella. When asked to perform a straight-leg raise, the patient may be unable to do so or will demonstrate an extensor lag. A patellar tendon rupture has similar findings; however, the palpable gap is in the patellar tendon with a proximally retracted patella.
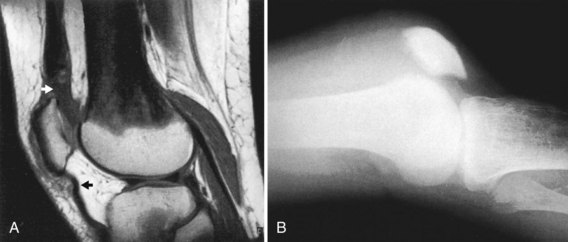
Although extensor mechanism disruptions are typically diagnosed from the history and physical examination, imaging studies often prove useful in confirming the diagnosis of quadriceps and patellar tendon tears or differentiating complete from incomplete tears.103 Radiographs provide supporting information, especially on the lateral view. A low position of the patella and disruption of the quadriceps tendon shadow are associated with quadriceps tendon rupture (Fig. 66-1), whereas a high patellar position and disruption of the patellar tendon shadow or the infrapatellar fat pad contour are associated with patellar tendon rupture.19,51,56,91 Despite relatively obvious findings on physical examination and standard radiographs, delay in diagnosis of extensor mechanism rupture still occurs.70,81,112,120 Several diagnostic imaging modalities may be used in addition to standard radiographs to confirm the diagnosis, including arthrography, ultrasound, and magnetic resonance imaging (MRI). Before the advent of MRI, arthrography was widely used. In the presence of an extensor mechanism tendon rupture, extravasation of radiopaque dye into the defect occurs.2 However, arthrography has been largely replaced by noninvasive methods such as ultrasound and, more commonly, MRI for evaluation of this problem. High-resolution ultrasonography* may reveal a hypoechogenicity across the entire thickness of the tendon with an acute rupture or tendon thickening and alteration of the normal echo signal with chronic tears. Advantages of ultrasonography include collection of images in real time without exposure to ionizing radiation and relatively limited expense. However, operation of the ultrasound equipment plus interpretation of the images require the skills of a highly trained and experienced technician and radiologist. Hence, the reliability is highly operator-dependent. MRI is the imaging study of choice if the diagnosis cannot be established from the clinical and radiographic examination alone.10,29,117,121,126 In addition, MRI may be useful to identify other problems within the knee.132
Quadriceps Tendon Rupture
Overview of Surgical Management
Numerous techniques have been described in the literature for repair of acute and chronic rupture of the quadriceps tendon.† Over the years, the repair techniques have progressed from simple suture with catgut or silk80 to wire-reinforced repairs, suture anchors,110 autografts,40 xenografts, allografts, and the use of synthetic material.37,87 McLaughlin82,83 and McLaughlin and Francis84 have even recommended a two-stage procedure with traction for better approximation of the tendon. With an acute intrasubstance rupture, direct repair may be performed. A straight midline incision will expose the quadriceps tendon rupture, which is then irrigated of hematoma. The tendon edges are débrided and cut fresh to normal-appearing tendon. If there is sufficient tendon proximally and distally, an end to end repair is performed with multiple interrupted no. 2 nonabsorbable sutures, and the retinaculum is repaired with multiple interrupted no. 0 absorbable sutures. Once the repair is complete, careful assessment of patellar rotation and tracking should be performed. The knee is then extended and the repair may be protected with a cerclage wire or nonabsorbable suture. The wound is closed in layers and the leg placed in a cylinder cast for 6 weeks. When the cast is removed, a control dial hinged-knee orthosis (Fig. 66-2) is used so that flexion can be gradually increased. The brace is discontinued when more than 90 degrees of flexion has been achieved and quadriceps strength is sufficient to support the limb.
Procedures
Acute Disruption
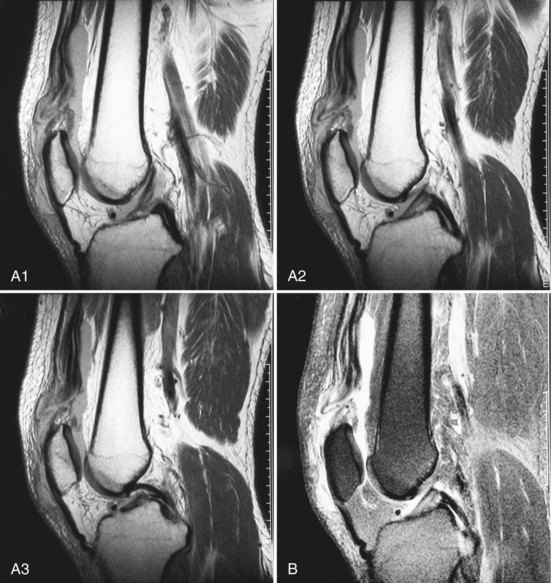
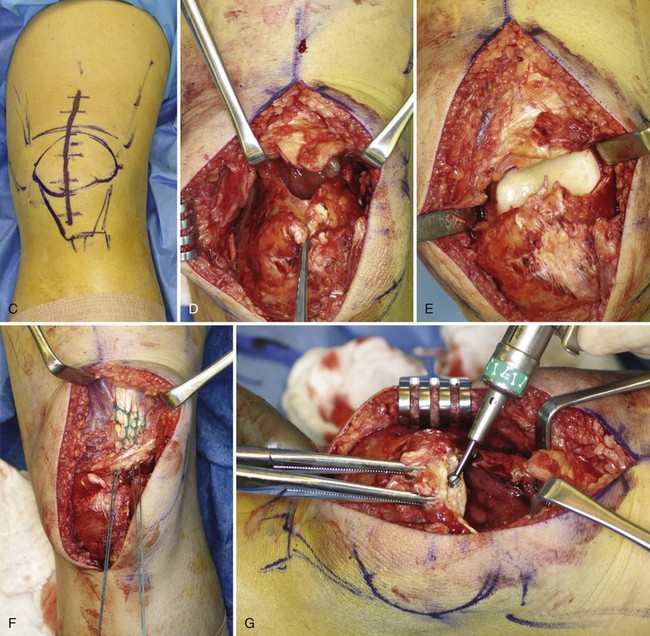
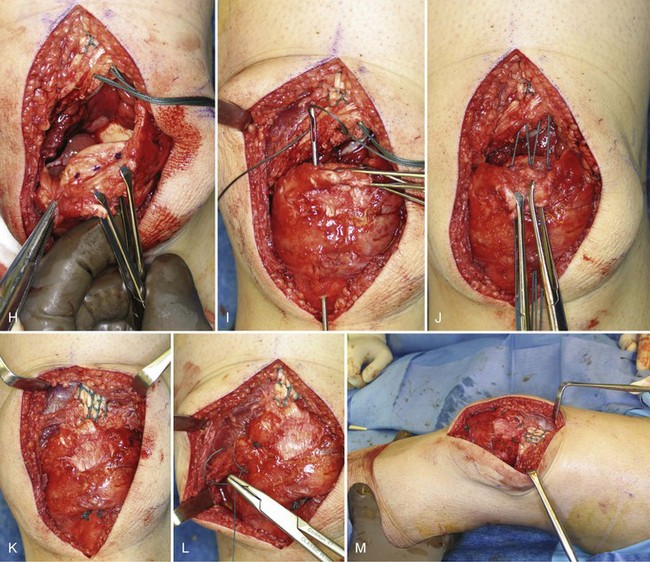
When the rupture occurs at the osteotendinous junction, we prefer to repair the tendon with transosseous sutures (Fig. 66-3). The MRI and repair technique are illustrated in Figure 66-4. A straight midline incision will expose the quadriceps tendon rupture (see Fig. 66-4C). The hematoma is evacuated (see Fig. 66-4D), the proximal end of the rectus femoris and vastus intermedius tendon is cut fresh to normal tendon, and the superior pole of the patella is débrided of residual tendon (see Fig. 66-4E). A no. 5 nonabsorbable suture is secured with an interlocking stitch along the lateral portion of the tendon.61 A second no. 5 nonabsorbable suture is placed in similar fashion along the medial portion of the tendon (see Fig. 66-4F). A transverse trough is then made in the superior pole of the patella with a high-speed bur (see Fig. 66-4G). To avoid patellar tilt, the trough should be placed as posterior as possible in the patella. Next, three marks are made with a methylene blue pen approximately 1.0 to 1.5 cm apart in the trough (see Fig. 66-4H). A Beath pin is used to drill through the medial mark, exiting at the inferior pole of the patella (see Fig. 66-4I). An anterior cruciate ligament (ACL) drill guide may be used to facilitate precise placement of the drill holes.95 The medial free end of suture is next placed through the eyelet of the Beath pin and the pin is pulled distally (see Fig. 66-4I). The Beath pin is then used to drill and pass the sutures in the central and lateral transosseous patellar tunnels (see Fig. 66-4J). The proximal end of the tendon is pulled into the trough and the sutures are held provisionally with a hemostat. The knee is then flexed so that patellar tracking and rotation can be assessed. The repair is completed by tying the no. 5 nonabsorbable suture distally with the knee in full extension (see Fig. 66-4K). Because the medial and lateral retinacula act as frontal plane stabilizers and play a complementary load-sharing role with respect to the patellar tendon, they are both repaired with multiple interrupted no. 0 absorbable sutures (see Fig. 66-4L).100 The repair is then checked to ensure that gapping at the repair site does not occur at 20 to 30 degrees of flexion (see Fig. 66-4M). Augmentation is typically not necessary.60,75,120 However, if the strength of the repair is in doubt, augmentation may be achieved with wire or Mersilene tape.83,87 Satisfactory results have also been obtained with suture anchors in lieu of transosseous sutures.110 After closure of the subcutaneous layer and skin, a cylinder cast is applied with the knee in full extension. Postoperatively, the cylinder cast is maintained for 6 weeks and the patient is allowed weight bearing as tolerated with a walker or crutches. Once the cast is removed, a control dial hinged-knee orthosis is used until 90 degrees of flexion is achieved and quadriceps strength returns. Although we prefer immobilization in the immediate postoperative period, some authors advocate early passive and active assisted range of motion of the knee after quadriceps tendon repair.69
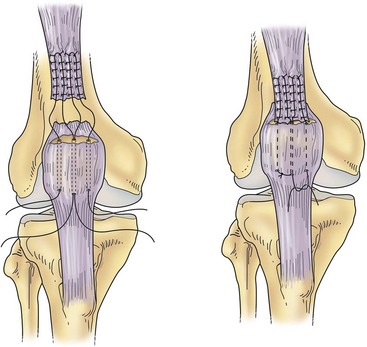
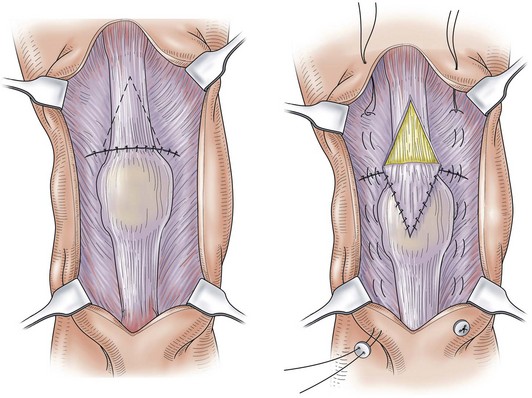
Figure 66-3 Acute repair of the quadriceps tendon into a bony trough.
(Redrawn from Scott WN [ed]: The knee, vol 1, St. Louis, 1994, Mosby–Year Book, p 472.)
Alternatively, the quadriceps tendon may be repaired using suture anchors rather than with this transosseous technique. The sutures may still be placed along the medial and lateral halves of the quadriceps tendon with an interlocking technique (modified Mason-Allen, Kessler, Krackow, or Bunnell technique).15
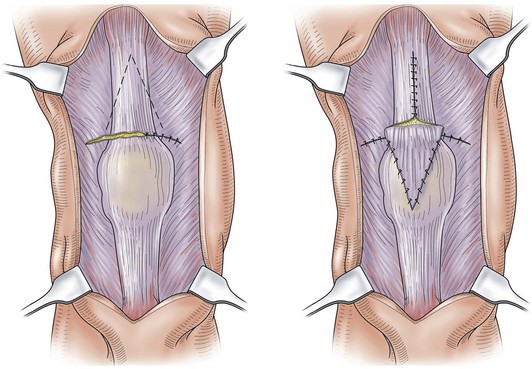
The Scuderi technique48,50,114,115 for repairing acute rupture of the quadriceps tendon has been widely used (Fig. 66-5). Using a midline longitudinal incision, the tendon rupture is exposed and the tendon edges are débrided until solid tendinous material is achieved. The knee is extended and the tendon edges are pulled with clamps, overlapped, and repaired with interrupted absorbable suture. A triangular flap 2.4 to 3.2 mm thick, 7.5 cm long on each side, and 5.0 cm at the base is fabricated from the anterior surface of the proximal part of the tendon. The base of the flap is left attached about 5.0 cm proximal to the rupture. The flap is folded distally over the rupture and sutured in place. A Bunnell pullout wire is placed along the medial and lateral side of the quadriceps tendon, patella, and patellar tendon. The wound is closed in layers and the leg placed in a cylinder cast, with the knee in the extended position. Postoperatively, the cylinder cast is maintained for 6 weeks and, at 3 weeks, the pullout wires are removed. When the cast is removed, a control dial hinged-knee orthosis is used so that flexion can be gradually increased. It is also recommended that the patient undergo physiotherapy, especially a quadriceps-strengthening program.
Chronic (Neglected) Disruption
Neglected or chronic rupture of the quadriceps tendon presents a difficult reconstruction, and the results after repair of such tears are less satisfactory than after treatment of acute tears.112 A longitudinal midline incision is the preferred approach and the exposure may reveal a large gap between the tendon edges. When the tendon edges can be apposed, the ends are débrided and repaired with the Scuderi technique, as described earlier. However, when there is contraction of the tendon and a large gap, a Codivilla tendon-lengthening and repair procedure is recommended (Fig. 66-6). An inverted V is cut through the full thickness of the proximal part of the quadriceps tendon, with the lower margin of the V ending approximately 1.3 cm proximal to the rupture. The tendon ends are apposed and repaired with multiple no. 0 nonabsorbable sutures. The medial and lateral retinacula are also repaired at this time with multiple interrupted no. 0 absorbable sutures. The flap is brought distally and sutured in place. The open upper portion of the V is closed with interrupted no. 0 absorbable sutures. The reconstruction should be protected with a pullout cerclage wire. Postoperative treatment is similar to that after the Scuderi procedure.
Results of Surgical Management of Quadriceps Tendon Rupture
Results of repair and/or reconstruction of acute quadriceps tendon disruptions are generally favorable, irrespective of the type of repair or location of the tear (avulsion from the patella versus midsubstance tendon disruption).60,69,104,106,112 Results are comparable between unilateral and simultaneous bilateral disruption. Although 15% to 53% of patients may have quadriceps tendon deficits based on isokinetic testing postoperatively,27 most are able to return to their preinjury occupations. However, fewer than half of patients reach their preinjury recreational activity level. Range of motion is typically recovered postoperatively and approaches the motion of the contralateral extremity. Although Konrath and coworkers60 found no detrimental effect of delay in repair, others have shown a delay in surgical repair to be the single most important factor predictive of a poor outcome. Rougraff and colleagues112 have suggested that a delay of 1 week compromises the outcome of quadriceps tendon repair, with significantly worse functional results and lower satisfaction scores. These findings are supported by Siwek and Rao120 and Scuderi,114 who observed worse results with a delay in surgical repair of 2 weeks and 3 days, respectively. In a study of 29 quadriceps tendon repairs, Wenzl and associates128 have demonstrated a significantly higher probability of a successful outcome with repairs performed within 2 weeks from the time of injury. Levy and coworkers69 have also noted the best results in patients managed acutely with a Dacron graft. Surgical débridement of scar tissue plus direct repair of the quadriceps tendon are effective in the management of partial quadriceps rupture. Complications include rerupture and wound compromise. In a series of 53 repairs, Rougraff and colleagues112 have observed two reruptures; in Konrath and associates’ series60 of 51 patients, one rerupture was noted. No large series of surgical repair of chronic or neglected quadriceps tendon rupture is available; however, a number of case reports have suggested favorable results with several different reconstruction methods.
Quadriceps Tendon Disruption Associated With Total Knee Arthroplasty
Tears of the quadriceps tendon after TKA are rare, with a reported incidence ranging from 0.1% to 1.1%.28,74 Although a traumatic event may result in a quadriceps tendon tear, the contribution of other factors such as systemic disease, local injury, and factors related to the TKA technique may predispose an individual. With only a few series in the literature, these factors may only be speculated on; they may include rheumatoid and other inflammatory arthritides, diabetes mellitus, chronic renal failure, hyperthyroidism, and systemic and local steroid use. Possible factors related to the arthroplasty include overresection of the patella with subsequent quadriceps tendon injury, vascular injury to the tendon resulting from lateral retinacular release, incomplete healing after extensile approaches, and manipulation.98
As in the case of the native knee, incomplete tears of the quadriceps tendon in patients with a TKA generally do well with nonoperative treatment. In a series from Dobbs and coworkers,28 seven partial quadriceps tendon ruptures were treated nonoperatively, all with a satisfactory outcome. One of these seven ruptures was diagnosed 1 year after partial rupture and had no further treatment. This patient had a persistent extensor lag of 10 degrees and a palpable defect in the quadriceps tendon. Sixteen patients with a partial quadriceps tendon rupture underwent primary repair. These patients had a high complication rate (5 of 16), and 4 ultimately had an unsatisfactory result. This suggests that early diagnosis is imperative and nonoperative management, consisting of immobilization of the knee in extension for 4 to 6 weeks with weight bearing as tolerated, can yield good results for partial quadriceps tendon tears.
In contrast to the native knee, the results of complete quadriceps tendon tears in patients with a TKA are less predictable. In the series of Dobbs and colleagues,28 11 patients were identified with a complete quadriceps tendon tear. Ten underwent primary repair and only four had a satisfactory result. Complications included four reruptures, two infections, and one patient with symptomatic recurvatum and instability. Similarly, Lynch and associates74 have reported unsatisfactory results with direct suture repair for three quadriceps tendon ruptures, with one sustaining a rerupture and the other two demonstrating limited knee flexion and significant extensor lag. Because of the discouraging results of operative treatment by direct suture repair, augmentation with autogenous graft material such as semitendinosus tendon or graft material such as Marlex mesh should be considered.
Patellar Tendon Rupture
Overview
Rupture of the patellar tendon is less common than rupture of the quadriceps tendon and generally occurs in patients younger than 40 years.55,120 Systemic inflammatory diseases, chronic metabolic disorders, anabolic steroid abuse, local steroid injections and, most commonly, progressive degenerative processes of the tendon have all been implicated as potential factors associated with an increased risk for tendon rupture.21,52,86,89,111 Rarely, patella tendon rupture occurs following anterior cruciate ligament reconstruction using bone-patellar tendon-bone (BPTB) autograft, predominantly in the early postoperative period.44 Most of these ruptures occur at the inferior pole of the patella, but may also take place in the midsubstance of the tendon or, rarely, at the insertion of the tubercle.22,76 The patella may be displaced 5 cm proximally as a result of associated retinacular and capsular disruption caused by the strong pull of the quadriceps mechanism. Disruptions through the substance of the patellar tendon can occur spontaneously but are more often caused by trauma or laceration. Early diagnosis and treatment provide the best results.
Historically, McLaughlin83 and McLaughlin and Francis84 recommended that repair of the patellar tendon be reinforced with the use of stainless steel wire anchored to a bolt placed in the tibial tubercle. Hsu and colleagues47 have reported a technique of primary repair reinforced with a neutralization wire. Siwek and Rao120 also recommended that all immediate repairs of the patellar tendon be reinforced by external devices. Several reports have described reinforcing the repair with various augmentation grafts, including autografts, allografts30,54 (fascia lata, semitendinosus, gracilis), and synthetic grafts (Mersilene,87 Dacron,35,36,69 carbon fiber,33 and a poly-p-dioxannone cord59). In a study by Ravalin and associates,107 12 fresh-frozen cadaveric specimens were used to compare standard repair with transosseous sutures without augmentation, with augmentation using a no. 5 Ethibond suture and with augmentation using 2.0-mm Dall-Miles cable. Gap formation at the repair site was assessed after cycling the knees in a custom knee jig; it was greatest in the repairs without augmentation and least in the group augmented with the cable. However, clinical reports have demonstrated satisfactory results of acute patellar tendon disruption repaired without augmentation. In a series of 15 consecutive patients, Marder and Timmerman76 published excellent results with primary repair of acute patellar tendon disruption treated by suture repair alone.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree