Proximal Row Carpectomy
Ann E. Van Heest
James H. House
Indications
Most candidates for a proximal row carpectomy have a severely disabled, painful wrist with a limited arc of motion and decreased grip strength. Removal of the diseased proximal carpal bones (scaphoid, lunate, and triquetrum) with careful capsular repair provides an articulation of the capitate in the lunate fossa of the distal radius, as a motion-sparing procedure (1,2,3,4,5,6). By comparison, with fusion procedures, early mobilization is possible with proximal row carpectomy. Proximal row carpectomy is indicated for a variety of specific conditions, including scapholunate advanced collapse, Kienböck disease, carpal injuries, Preiser disease, and wrist contractures caused by neurologic disorders. Each of these conditions is described below in detail.
Scapholunate Advanced Collapse
Degenerative arthritis secondary to scapholunate instability develops in a progressive pattern, as Watson and Ballet have documented (7). Degenerative changes most commonly originate between the tip of the radial styloid and the scaphoid, progressing along the scaphoradial joint. The capitolunate articulation is next affected, and the radiolunate joint is spared. Even in advanced cases, the articular cartilage of the lunate fossa remains unaffected, so that proximal row carpectomy is an ideal option.
The articular cartilage of the capitate can be affected to varying degrees in advanced cases. In our experience, even if the capitate has some fissuring or thinning, proximal row carpectomy results are not compromised. When severe midcarpal arthritis with significant degenerative changes are seen in the head of the capitate, proximal row carpectomy is contraindicated.
In our opinion, proximal row carpectomy is a more attractive option for this type of degenerative arthritis than intercarpal fusion because the period of postoperative immobilization is shortened and the possibility of re-operation for nonunion is not a concern.
Kienböck Disease
Alexander and Lichtman (8) consider proximal row carpectomy a salvage procedure suitable only for stage IV Kienböck disease (carpal collapse with associated degenerative changes). In our experience, however, stage II (lunate fracturing) and stage III (carpal collapse without degenerative changes) disease are equally suitable for proximal row carpectomy treatment in patients who are not candidates for joint leveling by osteotomy (see Chapter 32). If the disease process is treated in its earlier stages, the articular cartilage of the lunate fossa and capitate head are intact, a condition that theoretically allows greater longevity for the proximal row carpectomy. Recent studies have shown that results are improved for patients with Lichtman stage IIIa and IIIb disease, and that proximal row carpectomy commonly results in early failure for Lichtman stage IV disease (9).
Scaphoid Nonunions
Persistent scaphoid nonunion following surgical intervention is amenable to effective treatment with a proximal row carpectomy. Nonunions with small proximal pole fragments, unrecognized
nonunions presenting with dorsal intercalated segmental instability, and secondary radioscaphoid degenerative changes are also treatable in this way.
nonunions presenting with dorsal intercalated segmental instability, and secondary radioscaphoid degenerative changes are also treatable in this way.
Carpal Injuries
Acute injuries to the proximal carpal row can be severe, on occasion. In open (10) or closed injuries, especially with devascularized scaphoid or lunate fragments or multiple proximal carpal fractures, proximal row carpectomy provides simple and effective definitive management. Additionally, dislocations and ligamentous disruptions, especially those initially unrecognized and unreduced, can be effectively treated subacutely with proximal row carpectomy. In our experience, this patient group achieves the best postoperative results, manifested by near-normal grip strength, improved range of motion, and excellent pain relief.
Preiser Disease (Avascular Necrosis of the Scaphoid)
Patients with idiopathic or posttraumatic avascular necrosis of the scaphoid are excellent candidates for proximal carpectomy, because the degenerative process is primarily confined to the radioscaphoid articulation. The capitate and lunate fossa are usually spared of degenerative changes.
Severe Flexion Contractures
When a patient has severe functional deficits owing to a flexion posture that is rigid or not amenable to tendon transfer alone, proximal row carpectomy shortens the carpal segment, allowing more functional positioning (11,12). Such wrist contractures occur with arthrogryposis, cerebral palsy, or other spastic neurologic conditions. This procedure is also a useful adjunct to wrist arthrodesis for patients with chronic wrist flexion contractures who have sufficient digital control to function with an immobile wrist.
Contraindications
Three relative contraindications to proximal row carpectomy exist. First, Ferlic et al. (13) reported unsatisfactory results in 75% of patients with rheumatoid arthritis. Second, in our experience, patients with failed lunate silicone implants have had variable clinical results with proximal row carpectomy. Although some patients, after having a Silastic lunate, have done well with proximal row carpectomy as a salvage procedure; in general, clinical results are unpredictable due to the silicone synovitis, which can persist despite removal of the diseased bones. Finally, significant capitate articular damage is a contraindication to proximal row carpectomy. In a patient with SLAC wrist, we often opt before surgery for either four-bone intercarpal fusion or proximal row carpectomy; we make an intraoperative decision depending on the condition of the head of the capitate. Additionally, Tang and Imbriglia (14) have described the use of osteochondral grafting of the head of the capitate, in association with proximal row carpectomy, if the head of the capitate demonstrates focal degenerative changes.
Preoperative Preparation
Candidates for proximal row carpectomy present with a variety of different carpal disorders, as discussed above. Consistent physical findings include limited and painful range of motion in the wrist and decreased grip strength.
It is important for the physician to record accurately preoperative motion and strength values for postoperative comparison. Obtain routine radiographs as well as appropriate secondary imaging studies to diagnose and stage accurately the patient’s condition.
Technique
After administering regional or general anesthesia, position the patient supine and place a tourniquet on the proximal arm.
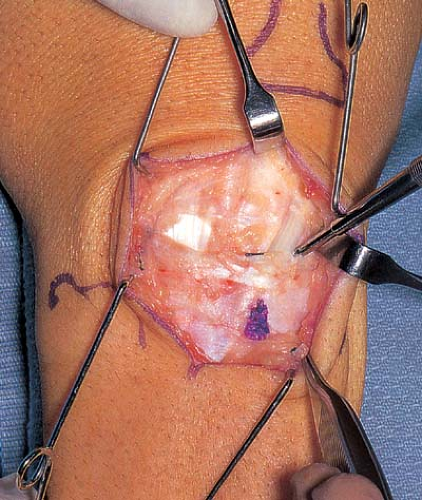
Figure 26-2 Identify the proximal and distal extents of the extensor retinaculum. The dental probe distally is under the extensor pollicis longus tendon.
After routine surgical scrubbing and limb draping, elevate and exsanguinate the limb, and inflate the tourniquet to a pressure of 250 mm Hg.
Make an oblique longitudinal incision, centered over the radiocarpal joint, from the ulnar side of the radius proximally to the base of the second metacarpal distally (Fig. 26-1).
Dissect the subcutaneous tissue to the extensor retinaculum, taking special care to preserve subcutaneous nerves and vessels (Fig. 26-2).
Identify the proximal and distal extents of the extensor retinaculum (Fig. 26-3).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree









