Proximal Interphalangeal and Metacarpophalangeal Joint Silicone Implant Arthroplasty
Charles A. Goldfarb
DEFINITION
Arthritis of the metacarpophalangeal (MCP) or proximal interphalangeal (PIP) joints may cause pain, deformity, and decreased motion. Rheumatoid arthritis (RA), osteoarthritis, and posttraumatic arthritis are common causes.
Silicone implant arthroplasty may be considered as a surgical option after failure of nonoperative treatment in the patient with pain, functional disability, or both secondary to arthritis at the MCP or PIP joint.
The primary function of the silicone implant is to serve as a dynamic spacer until the joint is encapsulated; thereafter, the joint can be expected to maintain alignment and provide a satisfactory range of motion.
ANATOMY
Metacarpophalangeal Joint
The MCP joint is condyloid with motion in three planes: flexion-extension, abduction-adduction, and rotation.
The head of the metacarpal is wider on its volar aspect, providing greater stability in flexion. The radial condyle is larger as well, contributing to the ulnar deviation posture most commonly seen in RA patients.
Collateral ligaments arise dorsal to the center of rotation; this, together with the shape of the metacarpal head, contributes to the cam effect that is manifest by collateral ligament laxity in extension and tightness in flexion.
Hyperextension of the MCP joints is common; however, the volar plate limits excessive motion.
Proximal Interphalangeal Joint
The PIP joint is a hinge joint with an average arc of motion of 0 to 100 degrees of flexion.
The bony anatomy is crucial to PIP joint stability in all positions; the base of the middle phalanx is wider volarly, thus helping to prevent dorsal dislocation. The PIP joint is more stable in all positions compared to the MCP joint.
The proper collateral ligaments originate from the center of rotation of the proximal phalanx head and insert onto the volar base of the middle phalanx; they provide stability in all positions. The accessory collateral ligaments insert onto the volar plate and provide more stability in extension. There is no significant cam effect with the PIP joint.
The volar plate resists hyperextension and is a key supporting structure of the joint.
PATHOGENESIS
Arthritis of the MCP or PIP joints may be idiopathic, posttraumatic, or inflammatory (RA).
Idiopathic osteoarthritis involves the distal interphalangeal joint most commonly, but the PIP joint is also affected; the MCP joint is less commonly involved.
The PIP joint is the most frequently traumatized finger joint and, thus, has the highest incidence of posttraumatic arthritis. Given the shortcomings of the salvage procedures for PIP joint arthritis, an anatomic joint reduction and aggressive restoration of the normal anatomy after trauma is critical to reduce the risk of arthritis.
The bony congruity of the PIP joint makes it poorly tolerant of any loss of cartilage; deformity and loss of motion may progress quickly.
Inflammatory arthritis (RA) most commonly affects the MCP joint but may also involve the PIP joint. In RA, a proliferative synovitis compromises the soft tissue support of the affected joint and may lead to the characteristic deformities at the MCP joint, including volar subluxation (and a flexed posture) and ulnar deviation. The PIP joint is less predictable because attenuation of the volar supporting structures may lead to joint hyperextension, whereas compromise of the central slip insertion will lead to a joint flexion deformity.
The efficacy of the disease-modifying antirheumatic drugs has dramatically decreased the need for joint arthroplasty in these patients.
NATURAL HISTORY
The natural history of osteoarthritis or posttraumatic arthritis of the PIP joint is progression with loss of motion, pain, and, in some patients, deformity. The MCP joint is less commonly affected and is also more tolerant of arthritis, given its increased mobility in all planes.
In the patient with severe RA not controllable by disease-modifying antirheumatic drugs, joint inflammation will lead to progression of the arthritis.
The functional effect of the arthritis depends on the degree of involvement, the specific joint, and the involvement of the adjacent joints.
PATIENT HISTORY AND PHYSICAL FINDINGS
It is vital that the surgeon understand how the arthritis specifically affects the function of a particular patient. This depends on many factors, including adjacent joint involvement, specific patient activities, and the degree of pain experienced.
Physical Examination
Key components in the physical examination are as follows:
Palpate along the joint line to confirm the site of pain and presence of synovitis.
Measure active and passive range of motion of the joint with a goniometer. Joint motion is lost with arthritis. Pain with motion is noted.
Measure coronal plane deformity (angulation) of the joint with a goniometer. Progressive arthritis leads to joint deformity.
Stress the joint in a radial-ulnar directions to evaluate the collateral ligaments. The MCP should be tested in flexion; the PIP joint may be tested in any position but is most commonly tested in extension. Attenuation of collateral ligaments may occur in RA or after trauma.
Assess the integrity of intrinsic and extrinsic tendon function and strength: most commonly abnormal in RA or after prior trauma
Assess for tendon shortening or lengthening (eg, after repair of an open injury) and the presence of tendon adhesions, which is most important in posttraumatic conditions.
Perform the Elsen test: Integrity of the central slip is important when contemplating PIP joint arthroplasty.
Evaluate alignment and function of the adjacent joints (including the wrist), as there is an intimate relationship between the joints.
In inflammatory conditions, the more proximal joints, most importantly the wrist, are also examined. If wrist deformity is not corrected before surgical correction of distal disease, surgical correction (such as MCP arthroplasty) will have a higher incidence of failure due to the uncorrected deforming forces.
Assess for intrinsic or extrinsic contractures after hand trauma.
Perform the intrinsic tightness (Bunnell) test: If the intrinsics are tight, therapy or surgical intervention may be needed.
IMAGING AND OTHER DIAGNOSTIC STUDIES
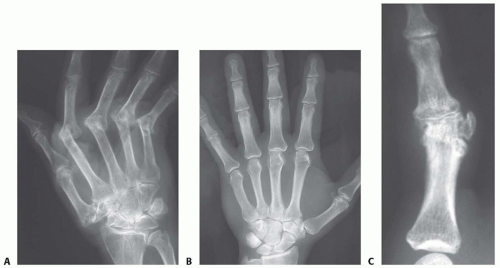
Posteroanterior and lateral plain radiographs provide sufficient diagnostic information. Occasionally, oblique radiographs are helpful (FIG 1).
Magnetic resonance imaging (MRI) and computed tomography (CT) are of limited use in the evaluation of the MCP and PIP joints.
DIFFERENTIAL DIAGNOSIS
Acute fracture with or without joint subluxation
Collateral ligament injury
Joint infection
Flexor or extensor mechanism injury
NONOPERATIVE MANAGEMENT
Anti-inflammatory medications
Steroid injections
Hand therapy to address contractures, including splinting
SURGICAL MANAGEMENT
Surgery is considered if nonoperative management fails. Given the limitations of silicone implant arthroplasty as noted in the following text, the decision for surgical intervention should be patient driven.
The best outcome is expected in patients with joint-based pain and a well-preserved arc of motion and minimal deformity. Patients without pain and presenting with deformity or a lack of motion are not ideal candidates for arthroplasty, especially if the adjacent joints are functioning well. Joint arthroplasty, of any variety, does not reliably increase motion at long-term follow-up.
In RA, an ulnar drift and volar subluxation of the MCP joints with a flexion posture of the joints may lead to weakness and a loss of the ability to grasp larger objects. These deformities are also unsightly. Surgical intervention in these patients can be expected to improve the appearance and function of the hand.
Preoperative Planning
All imaging studies are reviewed.
Involvement of adjacent joints is assessed.
Multiple MCP or PIP joints can be treated with silicone arthroplasty at the same surgical setting, but we do not typically recommend MCP and PIP joint silicone arthroplasty in the same finger.
In patients with symptomatic disease at both the MCP joint and the PIP joint, the MCP is typically treated with silicone implant arthroplasty and the PIP joint is fused.
An assessment of the ligamentous stability of the MCP and PIP joints is performed under anesthesia.
MCP and PIP arthroplasty is performed cautiously in the index (or long) finger, as pinch forces may be problematic for joint stability if the collateral ligaments are elongated or compromised with surgery.
Templating is performed to ensure that appropriate-sized implants are available.
Positioning
The patient is supine with the extremity on an arm table.
A nonsterile arm tourniquet is used.
General or axillary block anesthesia is used.
Approach
The MCP joint is approached from dorsally with a midline incision.
The PIP joint may be approached from either the dorsal or volar approach.
TECHNIQUE
▪ Metacarpophalangeal Joint Silicone Arthroplasty
Incision and Dissection
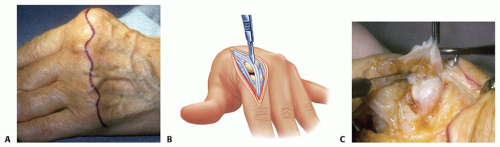
If a single joint is being addressed (osteoarthritis or posttraumatic arthritis), make a longitudinal incision over the MCP joint. If multiple joints are being addressed, make a transverse incision over the metacarpal necks2 (TECH FIG 1A).
Protect the superficial veins (most important in RA patients).
Identify and protect the extensor tendons.
In RA, the tendons may be translocated in an ulnar direction. If so, divide the sagittal bands on the ulnar side to allow later centralization of the tendons.
If the tendons are centralized, the interval between tendons (index and small finger between extensor indicis proprius or extensor digit minimi and extensor digitorum communis) can be used to approach the joint (TECH FIG 1B).
In RA, the ulnar intrinsic tendon is often a deforming force. In fingers with marked ulnar deviation, bring the tendon into the surgical field with a blunt hook and divide it.
Divide the joint capsule longitudinally for later repair.
Débride the joint (TECH FIG 1C).
It may be necessary to recess the collateral ligaments off their origin from the metacarpal head. Carefully protect their insertion onto the base of the proximal phalanx.
In osteoarthritis or posttraumatic arthritis, the collateral ligaments need not be released if adequate exposure can be obtained.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree