Proximal Humerus and Humeral Diaphyseal Fractures
CASE PRESENTATION
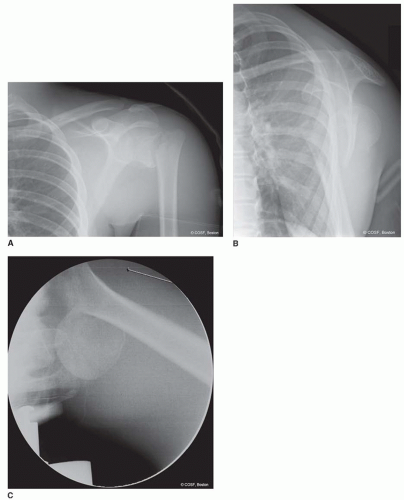
A 14-year-old male presents for evaluation of left shoulder pain after a fall. On clinical examination, there is swelling, tenderness, mild ecchymosis, and limited range of motion of the shoulder. The affected hand is pink and well perfused with a palpable radial pulse. Median, ulnar, and radial nerve function is intact, though he does complain of decreased sensation to light touch over the lateral deltoid. Radiographs demonstrate a displaced proximal humeral physeal fracture (Figure 26-1).
CLINICAL QUESTIONS
How do fractures of the proximal humerus and humeral shaft present in skeletally immature patients?
What are the radiographic views used to assess proximal humerus and humeral shaft fractures?
How are proximal humerus and humeral shaft fractures classified?
What is the remodeling potential of proximal humerus fractures?
How much deformity may be accepted in the nonoperative care of humeral shaft fractures?
What are the indications for surgical treatment of proximal humerus fractures? Of humeral shaft fractures?
What are the surgical approaches and methods of fixation for proximal humerus and humeral shaft fractures?
What are the treatment principles for humeral shaft fractures associated with radial nerve palsy?
What are the anticipated results of treatment?
What are the potential complications of surgical care?
THE FUNDAMENTALS
Fractures of the proximal humerus and humeral diaphysis are common injuries in children and adolescents.1 Due to the compensatory motion of the glenohumeral joint and tremendous remodeling potential imparted by the proximal humeral physis, the majority of these injuries can be treated nonoperatively with good clinical outcomes.2, 3, 4, 5 and 6 However, in older children with less growth remaining, severely displaced fractures may require operative treatment to restore anatomic alignment and maximize shoulder motion.7, 8 and 9 In these situations, a number of surgical techniques may be employed to achieve bony healing, improve skeletal alignment, and minimize potential complications.
Etiology and Epidemiology
Proximal humerus fractures are relatively common in children and adolescents, with an estimated incidence of 1 to 4:1,000 fractures per year.10,11 The pattern of injury is associated with age, with Salter-Harris type I fractures predominating in children <5 years old, metaphyseal fractures in children 5 to 11 years old, and Salter-Harris type II fractures in patients >11 years of age. The primary mechanisms of injury are direct blows to the shoulder or indirect forces resulting from a fall onto an outstretched hand. In addition to these traumatic causes, proximal humerus fractures may be seen in the setting of traumatic birth injuries or pathologic lesions of the humerus (see Chapters 20 and 50).
Humeral diaphyseal fractures are less common, accounting for 2% to 5% of childhood fractures.12 The estimated incidence is approximately 1 to 3:10,000 per year.11,13 A bimodal distribution has been observed, with the majority of humeral shaft fractures seen in children younger than 3 and older than 12 years of age.14 Humeral diaphyseal fractures may occur during birth, particularly in cases of macrosomia and breech presentation. In older patients, shaft fractures are due to direct trauma, indirect forces sustained during falls, penetrating injuries, or motor vehicle collisions.
Nonaccidental trauma should be considered as a part of the differential diagnosis for very young patients pre-senting with proximal humeral or diaphyseal fractures. Indeed, humerus fractures are thought to represent over 60% of newly diagnosed injuries and 12% of all fractures in cases of child abuse.15,16
Clinical Evaluation
Take off the blinders. You have to see opportunity before you can seize it.
—Greg Hickman
Patients typically present with pain, swelling, ecchymosis, and limited shoulder and elbow motion. The affected extremity is usually held in adduction and internal rotation, with fullness or deformity about the injury site. A comprehensive physical examination should rule out concomitant neurovascular injury. Deltoid function and sensibility along the lateral aspect of the shoulder should be checked in cases of proximal humerus fractures to rule out concomitant axillary nerve injury. Careful assessment of radial nerve function (first dorsal web sensation, wrist extensor, and thumb and digital extensor motor function)
is imperative in cases of humeral shaft fractures to assess for radial nerve palsy.
is imperative in cases of humeral shaft fractures to assess for radial nerve palsy.
Plain radiographs will confirm the diagnosis. Recommended for evaluation are anteroposterior (AP) lateral (scapular Y view), and axillary views of the proximal humerus. While axillary views are sometimes difficult to obtain, they are necessary to quantify displacement and angulation, which is often apex anterior (Figure 26-1C). In situations where an axillary view cannot be obtained, an apical oblique view of the shoulder (AP radiograph with 45 degrees of caudal tilt) may be useful. Pathologic fractures in the setting of unicameral bone cysts, aneurysmal bone cysts, or other benign and malignant conditions commonly occur in the proximal humerus. Radiographs should be carefully evaluated for underlying bony abnormalities, and further diagnostic workup should be considered prior to any surgical intervention in cases of diagnostic unknowns.
Understanding of the normal appearance of the secondary centers of ossification in the proximal humerus is imperative for accurate diagnosis. The proximal humeral epiphysis becomes radiographically apparent at 6 months of age; for this reason, infantile proximal humerus fractures require other imaging modalities (e.g., ultrasound, magnetic resonance imaging (MRI)) for adequate visualization. The greater and lesser tuberosities appear by 3 and 5 years of age, respectively. The tuberosities coalesce between 5 and 7 years and fuse with the humeral epiphysis at 7 to 13 years of age. Unlike adults, pediatric proximal humerus fractures rarely require computed tomography (CT) scans to identify fracture pattern and guide treatment.
Proximal humerus fractures are characterized according to their anatomic location and displacement. Physeal fractures are typically classified according to the Salter-Harris classification.17 In addition, Neer and Horwitz18 have proposed a classification based on the amount of radiographic displacement (Table 26-1).
Radiographic evaluation of humeral diaphyseal injuries is straightforward and based upon AP and lateral views of the entire humerus. The shoulder and elbow joints should be visualized to confirm appropriate joint alignment and rule out the rare associated floating elbow or fracture dislocation. Humeral shaft fractures are similarly classified according to their anatomic location, displacement, and angulation.
Table 26.1 Classification of pediatric proximal humerus fractures | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||
Surgical Indications
The time is always right to do what is right.
—Martin Luther King, Jr.
As the proximal physis contributes approximately 80% of the longitudinal growth of the humerus, there is great remodeling potential of displaced proximal humerus fractures in skeletally immature patients. For this reason, the majority of proximal humerus fractures may be successfully treated nonoperatively. Surgical treatment is typically considered in older patients with fracture displacement or angulation beyond what might be expected to spontaneously correct with continued skeletal growth (Neer and Horwitz grade 3 and 4 injuries) or in those patients with concomitant musculoskeletal or neurovascular injury.
Traditional guidelines have been proposed regarding what constitutes “acceptable” proximal humeral deformity amenable to nonoperative care6,14,18 (Table 26-2). In cases of unacceptable displacement in an older child or adolescent, closed reduction (CR) and/or surgical stabilization of the proximal humerus fracture may provide the best long-term outcome. Current indications for surgical treatment with internal or percutaneous skeletal fixation include open fractures, fractures associated with vascular compromise, fractures in the multiple-trauma patient, displaced intra-articular fractures, and unstable or unacceptable fracture displacement in an older child or adolescent.7 In the older child, if the proximal aspect of the greater tuberosity impinges on the acromion with attempted elevation, and the child is too skeletally mature to remodel, then closed reduction percutaneous pinning (CRPP) or intramedullary fixation is performed. It is our preference to use percutaneous pins for displaced physeal fractures and intramedullary fixation for metaphyseal injuries.
Table 26.2 Guidelines for “acceptable” alignment of proximal humerus fractures in children and adolescents | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||
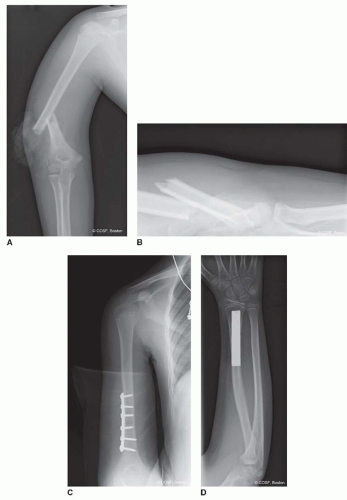
Similar considerations dictate humeral shaft fracture care. Due to the remodeling potential as well as the compensatory motion of the glenohumeral and scapulothoracic joints, considerable deformity is functionally and aesthetically acceptable. Indeed, up to 30 degrees of angulation, 2 cm of bayonet apposition, and 20 degrees of internal rotation are deemed acceptable. Surgical treatment is indicated in cases of excessive deformity, open fractures, fractures with associated vascular injury, floating elbow injuries, and the multiple-trauma patient (Figure 26-2).
SURGICAL PROCEDURES
A host of surgical techniques are available for reduction and stabilization of proximal humerus and shaft fractures. All are effective, and all should be in the quiver of the pediatric hand and upper extremity surgeon. The decision regarding which method of exposure, reduction, and fixation is dependent upon an array of individual patient factors, including skeletal maturity, injury pattern, and associated bony or soft tissue injuries. In general, the simplest and least invasive technique that can achieve the desired result should be selected.
Fracture reduction with percutaneous or internal fixation offers a number of theoretical advantages. First, bony fixation maintains fracture reduction, decreasing the risk of late displacement that may occur with immobilization alone. In addition, anatomic fracture reduction lessens the risk of shoulder impingement and loss of function. Furthermore, the fracture stability provided by skeletal fixation lessens pain and allows for a more expedient return to activities of daily living. Finally, in cases of severely displaced physeal fractures, anatomic reduction theoretically reduces the risk of post-traumatic growth disturbance.
Disadvantages include all the attendant risks of surgical intervention. In particular, there is a risk of a pin tract infection and/or iatrogenic axillary nerve injury with percutaneous pinning techniques. Finally, in cases where intramedullary fixation is utilized or where pins are cut beneath the skin, a second anesthetic is required for implant removal.
• Nonoperative Care
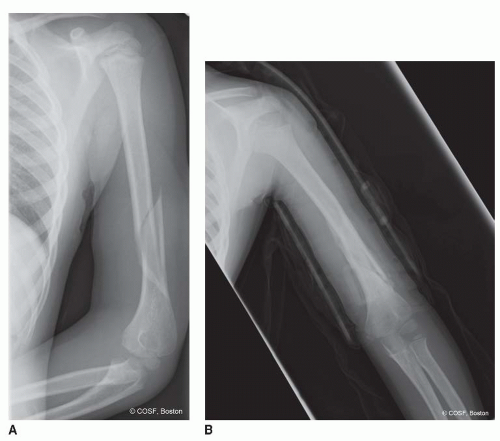
Nonoperative care is appropriate and effective for the majority of proximal humerus and humeral diaphyseal fractures. For proximal humerus fractures, simple sling immobilization is sufficient, with the expectation for bony healing in 4 to 6 weeks. In cases of diaphyseal humerus fractures with acceptable alignment, initial sling or coaptation splint immobilization followed by Sarmiento fracture bracing is effective19 (Figure 26-3).
▪ Closed Reduction and Pinning of Proximal Humerus Fracture
You must not only aim right, but draw the bow with all your might.
—Henry David Thoreau
CRPP is commonly utilized in the treatment of displaced proximal humerus fractures in older children and adolescents. CR maneuvers must counteract the typical deforming forces imparted on the fracture fragments to be successful. In proximal fractures, the humeral head fragment typically abducts, flexes, and externally rotates, due to the action of the rotator cuff muscles. Conversely, the diaphyseal fracture fragment is displaced proximally by the deltoid and adducted and internally rotated by the pectoralis major. While successful CR may be achieved in many cases, up to 50% of patients will demonstrate a loss of reduction with immobilization alone.8,18 For this reason, percutaneous pinning is added to maintain alignment during the healing process.
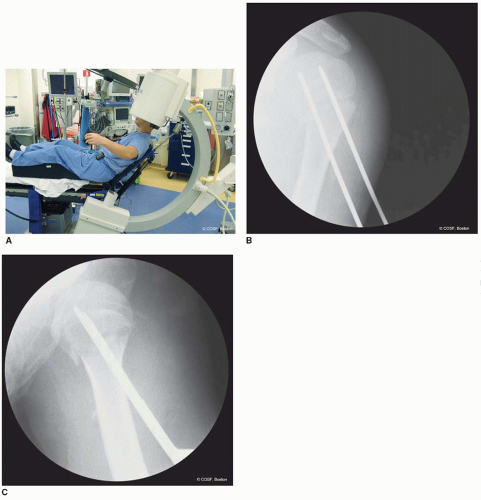
The patient is placed supine on a radiolucent table or in the modified beach chair position (Figure 26-4).
We prefer the modified beach chair position, as it allows full shoulder motion and facilitates intraoperative fluoroscopy in the AP and axillary projections. Due to the deforming muscle forces, CR is generally facilitated by general anesthesia with muscle paralysis. The entire shoulder and ipsilateral upper extremity is prepped and draped to facilitate fracture manipulation and fixation. Longitudinal traction followed by flexion, abduction, and external rotation of the humeral diaphysis is applied, reversing the deformity and reducing the distal fragment to the proximal fragment. Alternatively, shoulder abduction followed by forward flexion to 90 degrees followed by external rotation may be utilized to achieve reduction. Intraoperative fluoroscopy in orthogonal planes is used to assess the adequacy of fracture reduction. In situations where an adequate CR cannot be achieved, usually due to soft tissue interposition (biceps tendon, periosteum), open reduction is required. The standard deltopectoral approach is used to expose the fracture site, clear any interposed soft tissue, and restore anatomic alignment. Direct visualization as well as intraoperative fluoroscopy is utilized to confirm reduction.
We prefer the modified beach chair position, as it allows full shoulder motion and facilitates intraoperative fluoroscopy in the AP and axillary projections. Due to the deforming muscle forces, CR is generally facilitated by general anesthesia with muscle paralysis. The entire shoulder and ipsilateral upper extremity is prepped and draped to facilitate fracture manipulation and fixation. Longitudinal traction followed by flexion, abduction, and external rotation of the humeral diaphysis is applied, reversing the deformity and reducing the distal fragment to the proximal fragment. Alternatively, shoulder abduction followed by forward flexion to 90 degrees followed by external rotation may be utilized to achieve reduction. Intraoperative fluoroscopy in orthogonal planes is used to assess the adequacy of fracture reduction. In situations where an adequate CR cannot be achieved, usually due to soft tissue interposition (biceps tendon, periosteum), open reduction is required. The standard deltopectoral approach is used to expose the fracture site, clear any interposed soft tissue, and restore anatomic alignment. Direct visualization as well as intraoperative fluoroscopy is utilized to confirm reduction.
Once reduction is achieved, percutaneous skeletal fixation using smooth 0.0625” or 5/64” K-wires is performed. Stab incisions are made laterally at the level of the deltoid insertion through the dermis only. While this starting position necessitates a steeper angle for pin placement, this inferior starting position lessens the risk of iatrogenic axillary nerve injury.20




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree