Fig. 3.1
Varus-displaced, surgical neck two-part-fracture of the proximal humerus of a 68-year-old male after a car accident, treated with a proximal humerus nail (Synthes®)
3.7.5 Plates
3.7.5.1 Indications
Plates have a wide spectrum of indications. Even in osteopenic, complex fracture patterns, stable osteosynthesis can be achieved using plates. Today, angular stable locking plates are state-of-the-art. Less complex fractures can be treated by closed reduction and minimally invasive plate osteosynthesis using MIPO techniques. More complex fractures should be addressed by open reduction and lateral plate osteosynthesis. Limitations are poor bone quality, head-splitting fractures, and a medial comminution, especially in varus-displaced fracture types. An additional tension-band suturing is recommended inasmuch as it provides less secondary displacements of the tuberosities.
3.7.5.2 Positioning
Beach-chair position
Supine position
3.7.5.3 Approach
Anterior, deltopectoral approach
Anterolateral approach
Lateral approach
Minimally invasive approach
3.7.5.4 Implant-Related Risks
Secondary loss of reduction (especially in varus-displaced fractures)
Primary and secondary intraarticular malposition of screws
Implant failure
Injury of the axillary nerve if a lateral or anterolateral approach is chosen
Iatrogenic injury of the long head of the biceps tendon
3.7.5.5 Results
Successful healing can be achieved with locking plates, even in osteoporotic four-part-fractures (Fig. 3.2). However, it is essential to pay special attention to the following.
Anatomic reduction
Proper plate positioning below the greater tuberosity and in line with the shaft axis
Correct primary screw placement in the humeral head with subchondral bone purchase
Medial calcar screw support from inferior-lateral to superior-medial in varus-type fractures
Sutures through the rotator cuff to the plate
A recent prospective multicenter trial conducted by the AO shows an overall good clinical outcome using plates in 346 patients. The individual Constant score reaches values between 85 % and 87 % after 1 year follow-up [22, 25]. Nonunion is seen only in up to 5.8 %. It is remarkable that there was a high unsuspected rate of complications, up to 45 %. According to the systematic review of 791 patients treated with a locking plate, Thanasas confirmed a high incidence of complications. Osteonecrosis occurred in 7.9 %, screw cut-out in 11.6 %, and reoperations in 13.7 % [26]. Analysis of these complications shows that most result from surgical mistakes and are therefore avoidable. This is true for a wrong placement of the plate, especially a too high position resulting in an impingement, and for the primary intraarticular perforation of the screws. To decrease these mistakes, it is recommended to use a supine position, placing the shoulder on small shoulder supports to allow a precise intraoperative X-ray control in two perpendicular views without moving the arm.
Nevertheless, a meta-analysis published by Lanting in 2008 that included 66 studies and 2,155 fractures demonstrated that angularly stable plates seem to be favorable to nails in three- and four-part fractures [24].
Varus displaced humeral head four-part fractures, especially in combination with a medial comminution, are challenging, even today. In these cases, it is advisable to reduce the proximal humerus anatomically and to restore the calcar as precisely as possible. It is proven that a remaining varus angulation of 120° is a strong predictor of a secondary varus collapse with consequent secondary screw cut-out [27]. In addition, it is generally accepted to support the medial column with ascending calcar screws and/or a slight impaction of the humeral head. In cases of a medial comminution, implantation of an intramedullary fibular graft is shown to be beneficial. Augmentation with bone substitutes is disappointing because they do not integrate and are not able to prevent a secondary varus collapse.
Krappinger and colleagues determined several prognostic factors predicting a failure of plate osteosynthesis. These were for patients aged 63 years and older, with poor bone density of less than 95 mg/ccm, a nonanatomical reduction of the proximal humerus, and a lack of restoration of the medial calcar. The risk of failure highly increases in the presence of two or more risk factors [28]. Similar predictors of failure were detected by Südkamp and colleagues in a path analysis of factors for functional outcome at 1 year in 463 proximal humeral fractures [29].


Fig. 3.2
Valgus-displaced humeral head four-part fracture of a 72-year-old male treated with Philos®-plate. (a) Preoperative fracture situation, (b) the intraoperative result, (c) the result 2 days postop, and (d) the result at 1 year postop
3.7.6 Fracture Arthroplasty
3.7.6.1 Indications
Indications for fracture arthroplasty are mainly given if a stable osteosynthesis is not achievable because of either bad, osteoporotic bone quality and/or comminution of the proximal humerus. The poor bone quality can be estimated by measurements on preoperative CT scans [30] and/or based on the thickness of the metaphyseal cortex on plain X-rays. If both the medial and lateral cortex are less than 4 mm in length, severe osteoporosis is obvious [31]. Head-splitting fractures and impression-fractures involving more than 40 % of the humeral head surface are also considered to be treated with a fracture arthroplasty. However, in young patients, an osteosynthesis should be attempted because a secondary fracture arthroplasty in these fracture sequelae achieves better results. Humeral head ischemia should also be considered with care because only the humeral head ischemia seems to be predictable according to the predictors of Hertel [7] but not its consecutive development of an avascular necrosis [32]. This is also underlined by the fact that not every avascular necrosis of the humeral head becomes symptomatic.
In cases of a preexisting cuff-tear arthropathy or massive rotator cuff tear, a reverse shoulder arthroplasty is indicated. It is also suggested by some authors to use reverse shoulder arthroplasty generally in patients aged 75 and above. This recommendation derived from the bad outcome of many anatomic fracture arthroplasties accompanied by a secondary cuff insufficiency because of displaced and / or resorbed tuberosities.
3.7.6.2 Positioning
Beach-chair position
If a supine position was chosen when previously attempting an osteosynthesis, it is also possible to convert into a fracture arthroplasty using the supine position
3.7.6.3 Approach
Anterior, deltopectoral approach (standard)
3.7.6.4 Specific Risks
Secondary loss of reduction and/or resorption of the tuberosities
Incorrect implantation of the prosthesis (e.g., retrotorsion, height)
Incorrect dimension of the prosthesis (e.g., overstuffing)
Nerve lesion (axillary nerve)
Infection
3.7.6.5 Results
It is possible to achieve good clinical results, in terms of pain relieve and function, using an anatomical fracture arthroplasty. Hertel shows a main Constant score of 70/100 points [32] (Fig. 3.3). Other authors report less positive results, including a main Constant score of 41/100–64/100 points [33]. It is well known that the outcome strongly depends on the anatomic ingrowth of the tuberosities. Especially in the elderly, a secondary displacement and/or resorption of the tuberosities is frequently seen [34–36]. To decrease this risk, it is crucial to implant the prosthesis in an anatomic position avoiding any overstuffing and to reduce the tuberosities properly. It is also recommended to use autologous bone grafting, retrieving cancellous bone out of the humeral head and using tubercables instead of sutures in order to increase primary fixation. In order to prevent a negative winging effect of the tuberosities, a medial embracing fixation technique should be used.
The reverse fracture arthroplasty seems to be independent of the ingrowth of the tuberosities because the effective moment of the deltoid muscle is increased. In fact, it is still crucial to achieve an ingrowth of the tuberosities in order to achieve sufficient internal and external motions that are necessary for all daily activities. Until now, it was not possible to state the superiority of reverse fracture arthroplasty in comparison to anatomic fracture arthroplasty measured with the Constant score. Using reverse fracture arthroplasty, a mean Constant score between 53/100 points and 68/100 points can be achieved [37, 38]. Gallinet compared both systems in a matched-pair study in 2009 [39]. Reversed prostheses showed better results in terms of abduction, forward flexion, and Constant score (53/100 points versus 39/100 points, respectively). However, rotation was better with anatomic prostheses. The DASH score was equal in both groups. Typical complications differed significantly. The main complication was an abnormal tuberosity fixation in 17.6 % in the anatomic arthroplasty group and inferior glenoid notching in 93.7 % in the reverse arthroplasty group. According to the study published by Favard, one should use the reverse fracture arthroplasty with care, especially in patients aged less than 75 years [40–42]. Although Favard described a survival rate of reverse prostheses of 89 % after 10 years, taking removal or conversion to a hemi-arthroplasty as an endpoint, it is noteworthy that 72 % of all patients showed a Constant score of 30/100 points or less 10 years postoperatively [43]. This may be explained by a secondary weakness of the deltoid muscle and / or a polyethylene disease.
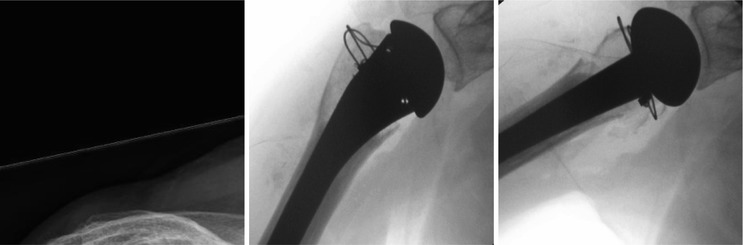
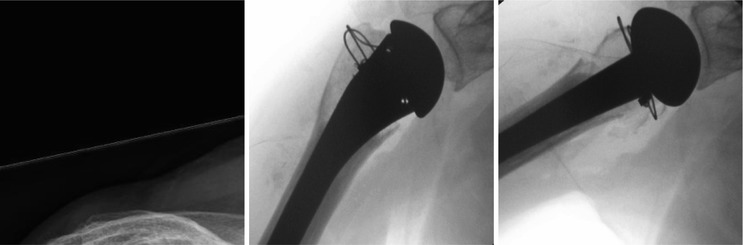
Fig. 3.3




Severely displaced humeral-head four-part fracture of an 86-year-old female resulting from a domestic fall, treated with an anatomic fracture prosthesis (Epoca®)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








