CHAPTER 32 Proximal Femoral Osteotomies in Adults for Secondary Osteoarthritis
Femoral Osteotomies for Adult Deformity
Surgical technique
Surgical Technique for Intertrochanteric Osteotomy
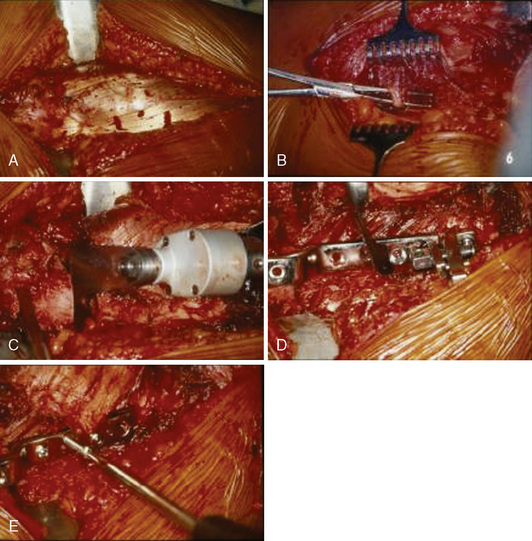
A standard lateral approach is used for all intertrochanteric osteotomies. The vastus lateralis is exposed by incising the fascia lata and reflected with Hohmann retractors to visualize the lateral femur (Figure 32-1, A). The vastus lateralis is sharply removed in the avascular plane from the vastus ridge. The vastus lateralis is detached from the intermuscular septum by blunt dissection, which allows for a wide inspection of the upper femur. Several perforating branches of the profunda femoral artery traverse the vastus lateralis and should be ligated correctly to avoid a postoperative hematoma; care should be taken so that the blunt dissection does not damage these vessels (see Figure 32-1, B). If it is necessary to inspect the hip joint, the approach can be extended proximally (i.e., the Watson-Jones approach), and the joint capsule can be opened to inspect the joint. The joint capsule is not routinely opened but rather only opened when indicated (e.g., for hump resection in a post-SCFE deformity). The linea aspera is decorticated. The seating chisel is inserted in the correct position, and the rotation is marked by placing a K-wire on each side of the planned osteotomy. Before this osteotomy is made, the seating chisel should be pulled back approximately 1 cm. An osteotomy parallel to the seating chisel is then made just proximal to the lesser trochanter (see Figure 32-1, C). Depending on the desired correction, a full or half wedge is removed to allow for the calculated varus–valgus or flexion–extension correction. During the osteotomy, blunt Hohmann retractors are placed around the femur to protect the femoral vessels and the femoral nerve. The definitive fixation is performed under compression with the classic AO (arbeitsgemeinschaft fur osteosynthesefragen) 90-degree or 100-degree blade plate, with different offsets that range from 10 mm to 20 mm. For cases in which extreme valgization is needed (e.g., for the treatment of femoral neck nonunions), a double-angled 120-degree or 130-degree blade plate can be used. For specific cases (e.g., intertrochanteric lengthening), a condylar plate is the preferred option. For all of our intertrochanteric osteotomies that involve the use of more or less right-angled blade plates, we performed the fixation under compression with the use of the AO compression device (see Figure 32-1, D and E). With the use of lateral compression, even open-wedge osteotomies heal without problems.
Potential Pitfalls and Considerations for Intertrochanteric Osteotomy
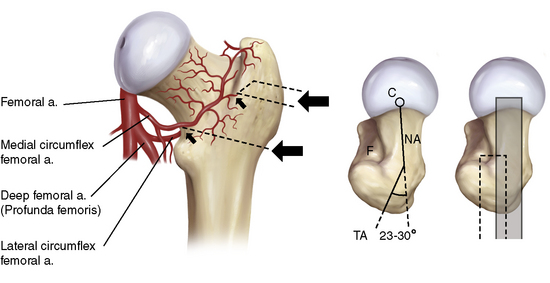
In addition, the placement of the seating chisel or blade plate can cause problems. The occurrence of AVN caused by the osteotomy is a worry. The vascular supply of the femoral head is provided by branches of the dorsal circumflex artery, which can be damaged in the intertrochanteric fossa if the femoral neck is perforated by the seating chisel. This can be avoided with the correct placement of the seating chisel (Figure 32-2).
When flexion or extension is added to the osteotomy, the position of the femur after the osteotomy should be anticipated when planning the placement of the blade plate. For example, a seating chisel that is inserted too far anteriorly cannot be fixed properly to the femur after a flexion osteotomy (Figure 32-3).
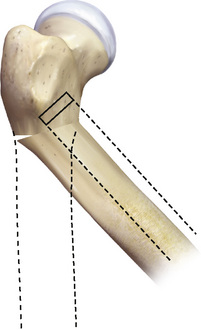
Figure 32–3 Schematic drawing of the possible faulty placement of a blade plate in an flexion osteotomy.
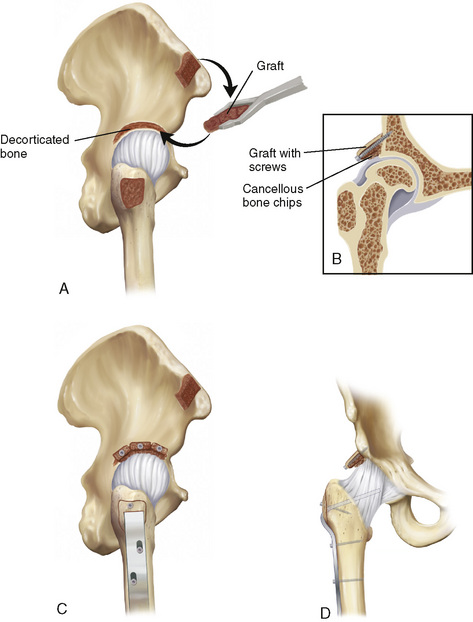
Surgical Technique for Shelf Plasty
For every procedure, an anterolateral approach was used that was similar to that used with a regular intertrochanteric osteotomy. The gluteal muscles are released with the use of an extracapsular osteotomy of the major trochanter. A cancellous–cortical bone graft is harvested from the ipsilateral interior iliac crest; this graft is bent into two or three blocks and predrilled for screw fixation. The joint capsule remains intact, but it is thinned on the superolateral side until head motion is visible. The supra-acetabular iliac bone is decorticated, and the prepared bone graft is fixated with 3.5-mm or 4.5-mm lag screws, with the patient’s leg in the calculated adduction or abduction position. When the function is tested in adduction, the graft should show plastic deformity. Some cancellous bone is pressed between the thinned joint capsule and the bone graft. A temporary screw fixation of the major trochanter is performed, if necessary, in combination with a distalization procedure (Figure 32-4). We performed distalization when the tip of the major trochanter was positioned higher than the center of rotation of the femoral head after correction. An intertrochanteric osteotomy is then performed in accordance with the standard AO technique; this technique is described earlier in this chapter.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree