Prosthetic Options for Persons with Upper-Extremity Amputation
John R. Zenie
Learning Objectives
On completion of this chapter, the reader will be able to do the following:
Impact of technology
Prosthetic management of individuals with upper-extremity amputations presents all allied health professionals, including prosthetists, with a set of unique challenges. For those wearing an upper–extremity limb, the TD of the prosthesis is not covered or obscured by clothing in the same way that a lower-extremity prosthesis is “hidden” by pants, socks, and shoes. By the virtue of its level, the person with upper-extremity amputation must cope with not only physical appearance changes, but the loss of some of the most complex movement patterns and functional activities of the human body.
In addition, limb deficiency in the upper extremity deprives the patient of an extensive and valuable system of tactile and proprioceptive inputs that previously provided “feedback” to guide and refine functional movement.1,2 Even the simplest tasks related to grasp and release become challenging. The ability to position prosthetic limb segments in space, as well as the ability to maintain advantageous postures needed to manipulate objects, challenge the medical community to continuously improve the functional and aesthetic outcomes of prosthetic replacement for patients in this population.3–5
Many of these challenges have been addressed with new and emerging technologies. These new technologies have made it possible, in some circumstances, to successfully “fit” a patient with high-level amputation who previously would have little or no reasonable expectation to succeed with traditional technology and fitting techniques.2,6,7 Advanced socket interface designs and material science have afforded prosthetists the ability to offer stronger, more stable platforms for all levels of amputation, while in most cases saving substantial amounts of weight. Similarly, more innovative suspension strategies and interface mediums have increased the functional ranges of motion a patient can comfortably achieve.8
These advancements have had a profound and positive effect on the comfort, function, and compliance of both conventional body-powered and externally powered prostheses at all levels of amputation. Furthermore, the huge strides made in the externally powered arena have in large part been driven by these advancements and technological breakthroughs.
Length of the residual limb
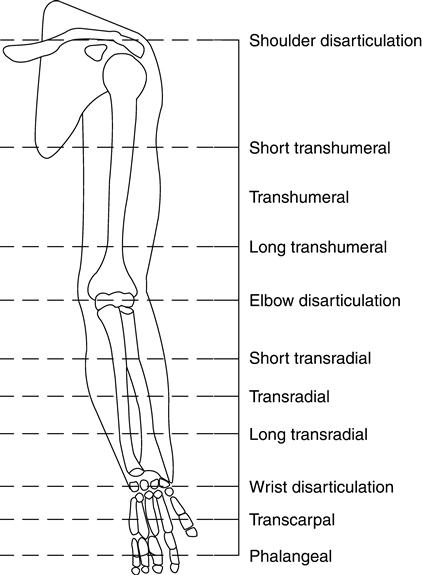
Amputations to the upper extremity can be classified or named by the limb segments affected (Figure 30-1). The most distal are at the finger, partial hand or transcarpal levels. Amputations that separate the carpal bones from the radius and ulna are referred to as wrist disarticulations. Amputations that occur within the substance of the radius and ulna are classified as transradial amputations. When the humerus is preserved but the radius and ulna are removed, the amputation is referred to as an elbow disarticulation. Those that leave more than 30% of humeral length are designated as transhumeral amputations. Shoulder disarticulations are those in which less than 30% of the proximal humerus remains. More proximal amputations that invade the central body cavity, resecting the clavicle and leading to derangement of the scapula, are described as forequarter amputations or scapulothoracic amputations. In clinical prosthetic and rehabilitation practices, transradial and transhumeral amputations account for nearly 80% of all upper-extremity amputations.6
All patients who have amputations of the upper extremity require a complete and thorough examination at the levels of involvement and of associated functional and physiological deficits associated with that specific amputation. For patients with partial hand amputations, the range of motion (ROM) of any remaining digits and the condition of the structural bones of the hand have a profound effect on the selection of possible prosthetic options. The inclusion or absence of an intact thumb also dictates the parameters of fitting.
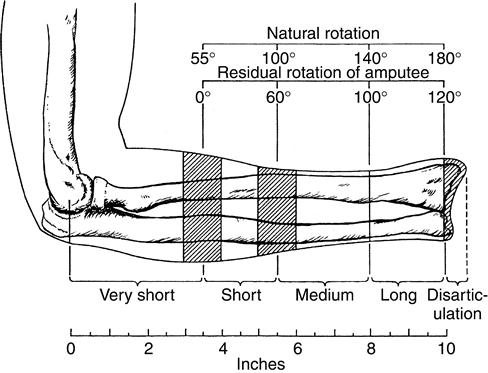
For those with transverse amputations of the forearm, the length of the residual limb affects the amount of functional elbow flexion and forearm pronation and supination that will be retained independent of prosthetic intervention.1 Articulations between the radius and the ulna along the entire forearm are necessary to provide for natural anatomical movements in supination and pronation; as the level of amputation moves proximally from the styloid process of the radius toward the elbow, the ability to perform and to use pronation and supination during functional activities is progressively lost (Figure 30-2). When the residual forearm is extremely short, all transverse motion is essentially lost, and it is difficult to gain any active functional forearm rotation for prosthetic use.
Amputations at the level of the elbow (elbow disarticulation) derive little functional benefit from the added length because the length of the limb limits options for cosmetic and functional placement of elbow units within the prosthesis, without substantially improving functional leverage.
Although the primary concern of surgeons who perform an upper-extremity amputation is adequate closure of the wound, they must also consider the potential advantages of a fairly long lever arm, balanced by an understanding of the space requirements for prosthetic components. Provided that adequate skin and tissue viability are not compromised, consideration should be given to adequate room for a full array of prosthetic componentry.
Upper-extremity prosthetic component
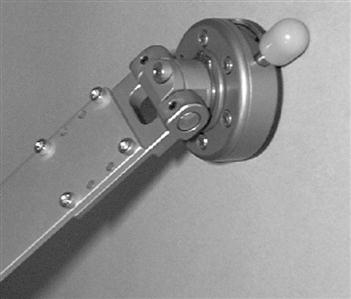
Prosthetic components can be thought of as a means to replace lost functional capacity associated with the anatomical loss of limb segments. A TD is employed to replace grasp and release. An elbow mechanism is used to replace the humeral-ulnar articulation; a shoulder mechanism is placed proximally to provide humeral orientation in space at the shoulder disarticulation and scapulothoracic amputation levels. Rotators can be placed in the forearm of the prosthesis to substitute for pronation and supination or above the elbow unit to substitute for internal and external rotation of the shoulder as well.9,10
Partial Hand, Transcarpal, and Wrist Disarticulation
Until recently, patients with digit, partial hand, or transcarpal amputations were often offered passive (nonfunctioning) cosmetic prostheses (restorations).11 Depending on the characteristics of the residual limb, a functional prehensile post might have been fabricated to regain some grasp and release capability of the affected limb. Recent advances in technology and microprocessors have made externally powered options more readily available (Figure 30-3).12 These advances permit electric control despite the extremely distal amputation site. Consideration must be given preoperatively to any remaining functional digits. The status of sensation and mobility of these digits should not be understated. If functional range and sensation are inadequate, the surgeon considers a more proximal level of amputation.
The wrist disarticulation residual limb provides a long and functional lever for prosthetic use.13 If the radial and ulnar styloid processes are preserved, then the prosthetist can use a positive suspension strategy over these prominences to keep the prosthesis and stable suspended on the residual limb, making harnesses unnecessary. The disadvantage of wrist disarticulation, however, is limitation in room to fit a wrist and hand unit into a cosmetically acceptable prosthesis. If the styloid processes have been modified or removed during surgery, more aggressive proximal suspension strategies are necessary. In addition, the extra residual limb length leads to a difference in arm length once the wrist and prosthetic hand unit is in place, which might be cosmetically unacceptable to the patient. In such cases, a more proximal amputation would allow for a full complement of prosthetic options.
Transradial and Transhumeral Considerations
For most adult transradial prostheses, nearly 8 inches of space is necessary beyond the distal residual limb for the prosthetic wrist rotator and TD or hand.13 Similarly, at the transhumeral level, approximately 6 inches of space must be present beyond the distal residual limb to accommodate a mechanical elbow mechanism within the prosthesis.14 For patients with a short residual humerus, a conventional (body-powered) prosthetic system may not be realistic, and even an externally powered prosthesis may be difficult or problematic to fit, suspend, and control. When the residual humerus is short, it may be necessary to treat a transhumeral amputation functionally as a shoulder disarticulation (Figure 30-4).
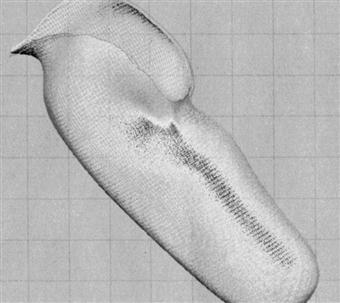
Positive models to fabricate any contemporary prosthesis can be secured with conventional plaster direct molding techniques similar to those used for lower-extremity amputations. Model acquisition and data collection are also possible using computer-aided design. Both direct contact and optical methods are finding ever-increasing utility in modern practice. This technology is particularly valuable as a means to quantify and document volume and shape changes, enhancing fit and function for optimal clinical outcomes (Figure 30-5).
Etiology of upper-extremity amputation
The etiology of upper-extremity amputations varies widely. The earliest recorded use of limb prosthesis was that of a soldier who reportedly amputated his own limb around 484 BC.15 One of the earliest known prostheses was fabricated of copper around 300 BC.16 These early attempts at prosthetic management predate early surgical considerations for lifesaving reasons by many decades. Ambrose Pare, whom many consider the father of modern orthopedic surgery, introduced early surgical techniques around 1529.17 Public belief is that Pare performed the earliest upper-extremity amputation, an elbow disarticulation, late in 1536. The incidence and prevalence of upper-extremity amputation over the past several centuries is attributed to advances in the pharmacological and surgical management of disease, as well as trauma.18 Upper-extremity trauma related to industry, mechanized farming, and armed conflict has been the catalyst for medical and prosthetic advancements in the twentieth century.6
The National Center for Health Statistics reports approximately 50,000 new amputations every year in the United States. With a ratio of 1:4 upper-extremity to lower-extremity amputations the number of existing and new upper-extremity amputees is both significant and most likely a population that is underserved. As the number of upper limb cases is relatively small in comparison to lower-limb cases, many prosthetic practitioners who are highly skilled and qualified in the arena of lower-limb prosthetics, have far lesser experience and confidence when dealing with complex upper-limb management. Furthermore, in the realm of externally powered prosthetics, fewer practitioners still have the additional education and certifications to work with these complex systems.
Of the approximately 54 million persons in the United States with disabilities, at least 10% have had amputations.19 Although the exact number of patients with amputations is unknown, the number of patients with acquired and congenital amputations is significant. Of all persons with amputations, the number of patients with amputations to the upper extremity is small in comparison to all total amputations.19 Compelling evidence suggests an estimated 10,000 new amputations to the upper extremity each year.20 These numbers represent a large number of individuals who require prosthetic intervention.
The primary cause of acquired amputations is trauma.6 Other causes of upper-extremity amputation are the various sarcomas, as well as congenital limb deformities, including amelias and phocomelias.21–23 Amputations to address congenital limb deficiencies are most often performed on individuals younger than 15 years old, while amputation after traumatic injury is most often performed on those between 15 and 45 years old.24 Seventy percent of all upper-extremity amputations occur in persons younger than 64 years of age.6,24 Because trauma is more likely to occur in the operation of machinery or in combat, many more amputations occur among males than females.24
Preprosthetic care
All patients with upper-extremity amputation, regardless of cause, require some degree of preprosthetic management. This is particularly essential with a recent amputation but includes even those persons who have worn prosthetic devices previously. Comprehensive preprosthetic and prosthetic management is a strong predictor of optimal rehabilitation outcomes.25,26 After amputation surgery, facilitation of wound healing and effective pain management are the foundations for all other types of preprosthetic care. Care is most effective if coordinated through a multidisciplinary team—the prosthetist, surgeon, nurses, physical and occupational therapists, counselors, and others as necessary.7
Edema and Volume Control
Edema and volume control are additional key elements of preprosthetic care. If the wound site is adequately protected and bandaged, compressive wraps or shrinkers should be used as soon as possible. In most cases, multidirectional shrinker garments are more effective than other methods, including elastic bandages.27 Shrinkers appear to more efficiently control volume and shape the residual limb. When donned properly, shrinkers have far less tendency to migrate or shift position on the residual limb. In addition, shrinkers are more effective at creating the consistent distal toward proximal pressure gradient that is most effective. The compressive garment should terminate proximal to the joint above the amputation site when possible. With the transhumeral amputation, this requires the shrinker to include a modified shoulder cap. Such a device is rarely commercially available and usually requires custom fabrication on site. This additional effort has been shown to produce favorable results in comparison with shrinkers that terminate more distally.26 Due diligence must be exercised to ensure that appropriate tension and compression gradients are achieved and maintained. Effective and timely volume management influences more than the residual limb volume and shape; many patients report that this compression is a surprisingly efficient tool in the management of phantom sensation.27
Skin Care, Desensitization, and Range of Motion
The services of a skilled therapist have proven invaluable in the areas of skin care, desensitization, and scar mobilization. Preprosthetic ROM and strengthening should be undertaken concurrently as tolerated.
Skin care can present some significant challenges, particularly when an individual has sustained a traumatic amputation. Chemical and electrical injuries with associated skin grafts can become problematic, particularly when irregular and uneven surface topography is present.28 Maintaining skin integrity throughout both the fitting and postdelivery phase of rehabilitation is extremely important. The appropriate medical professional should carefully assess any postoperative open lesions. Blast and percussion injuries also present a complex array of socket interface and electrical conductivity issues.29 This type of injury frequently displays an unusual soft tissue consistency. The tissue is unlike that of crushing, degloving injuries. Tissues exposed to the enormous energy associated with blast injuries frequently respond to the outside compressive forces of shrinkers and preparatory sockets much more dramatically than do tissues injured by other sources. This phenomenon must be considered carefully, as its effects profoundly affect any rehabilitation plan.
The nature of any volume management protocol in and of itself begins the limb maturation and desensitization process simultaneously. Further and more focused efforts must be undertaken to assure that limb volume is both stabilizing and fostering a limb shape or contour that is favorable to donning, wearing, and operating a prosthetic device.28 Limbs with large longitudinal contours or bulbous distal contours are least desirable. Residuum with insignificant tissue or skin coverage should also be avoided whenever possible. Ideally the residual limb is long enough to provide a functional lever arm but not so long as to preclude the use of a wide array of prosthetic components. Residual limbs with effective myodesis frequently display smaller myoelectric artifact without any apparent or material loss of volitional potential.
Preprosthetic ROM should be maximized regardless of the planned prosthetic intervention. Strengthening of the muscles about and proximal to the amputation is paramount. However, a more global approach to strengthening affords the patient a more expeditious and complete rehabilitation. These efforts to maximize ROM and increase volitional power should not overlook the secondary movers or accessory stabilizers. For patients with transradial amputations, for example, maximizing ROM and strength of pronation and supination is an important determinant of positive functional outcomes.
Adaptation Process
Patients and families facing amputation, whether congenital or acquired, adjust and cope with absence or loss of the limb differently.30 The extent or level of involvement often has little to do with the complexity of the adaptation process. All persons must find ways to deal with the functional and aesthetic issues related to limb loss. Adaptation is an ongoing process rather than a specific event. In many cases the services of a qualified psychotherapist are valuable, providing the patient and caregivers are amenable to such intervention.
Most professionals agree that there is a fairly short window of opportunity within which the prospects for successful rehabilitation are greatest, although there is disagreement about the duration of this “optimal rehabilitation” period. In most circumstances the earlier a patient can be evaluated, fitted, and trained, the more likely a positive rehabilitation outcome occurs.6 Malone and colleagues25 suggest high levels of success with patients fit within the first 30 days following amputation. In addition, individuals fit with a prosthesis as early as possible return to work quickly, many within 4 nbsps of injury.6,25
Prosthetic examination and evaluation
Examination of persons with upper-extremity amputations should include complete documentation of the involved limb’s ROM. Care should be exercised to identify both the active and passive ranges. Volitional muscle control should be evaluated and documented. Limb shape and contour, as well as tissue consistency, are important elements in the evaluation. Particular attention must be paid to any grafts, scars, or painful areas of the residuum. Pertinent medical history must be duly noted, as it may affect not only prosthetic development but all phases of the rehabilitation protocol.
The past medical history must adequately address any injuries or pathologies on both sides of the body. For patients with high-level amputations, the prosthesis, regardless of configuration or power source, ultimately has some integrated components across one or both of the axilla, as well as the thoracic wall.
The objective of all prosthetic interventions should be to restore as much functional potential as possible.31 This is best accomplished by using components, materials, and interface designs to most closely approximate the lost body segments and functions. The appropriateness of any design should address the patient’s vocational, recreational, and aesthetic needs. The needs of most patients can be met with one or more prosthetic options.
Prosthetic options
Depending on the patient’s situation, the prosthetist and rehabilitation team can make a number of recommendations. These include not providing a prosthesis, providing a passive prosthesis or cosmetic restoration, designing a conventional body-powered system, or providing a sophisticated myoelectrically controlled prosthetic limb with multiple components.
No Prosthesis
A significant percentage of patients with upper-extremity amputations elect not to use a prosthesis on a regular basis.6 In many cases this decision can be traced to a poorly conceived or executed prosthetic device that was provided early in the patient rehabilitation process.25 Some potential wearers report that the devices they have been exposed to are uncomfortable, heavy, and too slow during use or difficult to don and suspend.6 The advent of advanced materials has enabled prosthetists to build lighter, stronger, and more comfortable systems, as well as extremely cosmetic restorations. Despite these advancements, not all individuals with amputations integrate a prosthesis into their body image. The prosthetist or rehabilitation team should follow patients who choose not to use a prosthesis initially at regular intervals (often yearly) to ensure that their functional needs are being met. Given the rate of technological development, new components or devices are likely to become available to address problems the patient might have had at an earlier time.
Passive Prostheses and Restorations
This category of prosthesis consists of systems that do not possess the ability to actively position a mechanical elbow in space or actively provide grasp and release function, or both. The absence of these properties does not, however, render the prosthesis as passive as the name would suggest. These devices are extremely functional in terms of supporting objects or stabilizing items during bimanual tasks and activities, especially for young children with congenital deficiencies.32,33 These systems most frequently have a self-suspending design and use a realistic hand as a TD. Suspension is achieved either with specific socket interface geometry or suction negative pressure. The absence of operational mechanical components generally results in an extremely lightweight prosthesis.
The finish of these devices varies widely. Production latex cosmetic gloves provide an cost-effective medium for many patients. Many individuals, however, seek out more realistic restorations (Figure 30-6). These restorations require substantially greater investments in time and financial resources. This investment is most often rewarded with an extremely aesthetic, very natural appearing device. Silicone is the media of choice for these cosmetic limbs, primarily because it is practically impervious to outside contaminants. Where latex readily stains and deteriorates in ultraviolet light, silicone does not mark and, for all practical purposes, is inert. Generally, the additional cost of silicone is mitigated by its superior cosmesis, durability, and increased coefficient of friction (Figure 30-6).
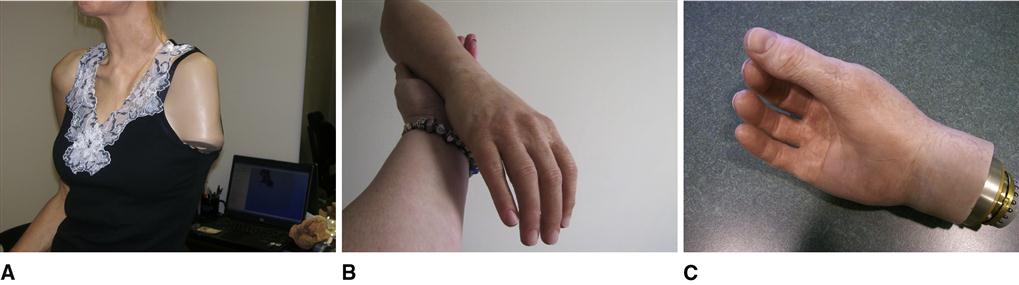
Laser scanning and computer modeling to create near perfect “mirror“ images of high level amputations, such as shoulder disarticulations, and scapulothoracic amputations (see Figure 30-6, A).
Conventional Body-Powered Systems
Conventional (body-powered) systems include any prosthesis that uses a control cable system to translate volitional muscle force and shoulder or arm movement to operate a TD or prosthetic elbow.34 The patient must use specific strategies in order to effectively create enough excursion in the cable to control the TD or preposition the forearm in space. In most instances the glenohumeral joint contributes the largest amount of excursion in conventional prosthetic control. Glenohumeral flexion typically has more than ample excursion and satisfactory power to provide useful motors for this type of control. Additional excursion can be achieved through scapular and biscapular abduction (scapular protraction). These secondary movements allow a well-trained and skilled prosthetic wearer to increase the functional work envelope, the space in which the wearer can effectively control the TD.
For most conventional upper-extremity prostheses, the functional envelope is limited to a relatively small area below the shoulders, above the waist, and not far outward past shoulder width.34 Many prosthetic wearers have significant difficulty with tasks that involve grasp-and-release tasks above the head or down near the feet. Because the control strategy involves generating cable excursion through flexion or protraction, or both, tasks and activities occurring behind the back are impossible. Despite these functional limitations, conventional prostheses have provided many patients with reliable and durable prosthetic systems.
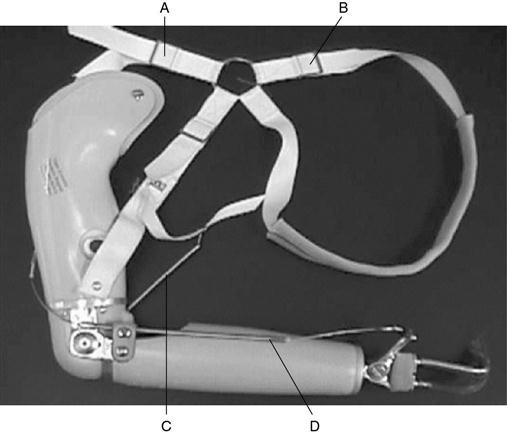
Figure-of-Eight Suspension and Control Cable
The foundation of all conventional body-powered prostheses is a harnessing system that provides both a firm anchor for the control cables and, in many cases, a stable means of suspension. Most conventional systems use a figure-of-eight–style harness (Figure 30-7). The terminal ends of the figure-of-eight are formed by means of an axillary loop that is fit over the opposite shoulder, a control attachment cable, and an anterior suspension component on the amputated side. Most prosthetists recommend that the center of the figure-of-eight be positioned just below the seventh cervical vertebra and slightly toward the sound side.34 The straps of the two axillary loops can be mobile by means of attachment to a circular ring or fixed with a sewn cross point. The use of a center ring often makes the donning process less difficult and appears to provide the most satisfactory ROM. Harnessing materials are most frequently constructed of medium weight Dacron webbing with both leather and plastic integrated components.
Cable Control for Self-Suspending Sockets
If the prosthetist recommends a self-suspending socket, the anterior suspension of a figure-of-eight harness is not necessary. In these instances a figure-of-nine harness, consisting mainly of the contralateral axillary loop, is used to minimize cumbersome harnessing while still maximizing a firm anchor for the control cable. Self-suspending sockets may be of an anatomically contoured design or that of a flexible silicone interface, with either a locking or suction valve mechanism.
Control and Suspension for Bilateral Prostheses
For patients with amputation of both upper extremities, careful clinical consideration must be given to achieving an easily donable and highly functional prosthetic system. Instead of using a traditional figure-of-eight harness with a contralateral axillary loop for each prosthesis, the two anterior suspension components are linked.35 In this arrangement, the bilateral prosthetic system is effectively stabilized by the equal counteracting forces from each prosthesis. On the basis of the patient’s functional needs, the prosthetist may use either a single- or dual-ring system to maximize the efficiency of the conventional prostheses (Figure 30-8). The second ring in the system, mounted below the primary ring, is used exclusively for the control attachment straps. The more proximal ring is used for the anterior suspensor straps and, for patients with bilateral transhumeral residual limbs, the connection of elbow locking straps.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree