INTRODUCTION
Serous wound drainage after total knee arthroplasty (TKA) is not uncommon, but prolonged drainage is associated with an increased risk of developing infection. If infection is suspected, early irrigation and debridement is indicated to prevent chronic infection involving the prosthetic components.
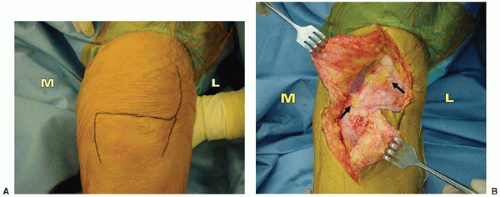
Skin necrosis can rapidly lead to exposure of the implant and deep infection of the TKA. The risk of skin necrosis can be reduced by utilizing previous scars and more lateral incisions in the multiply scarred knee when possible, and maintaining full-thickness skin and subcutaneous flaps during surgical exposure, as well as limiting early knee range of motion (ROM) after surgery. If full-thickness necrosis occurs, with resultant exposure of the TKA, prompt debridement and soft tissue coverage is necessary. Most soft tissue defects can be covered successfully with a medial gastrocnemius muscle flap transposition.
POSTOPERATIVE WOUND DRAINAGE
Blood drainage from the wound after TKA is common during the first few days after surgery. Once the wound is sealed and the skin begins to epithelialize, drainage should diminish considerably. However, serous fluid drainage can continue for up to a week in some patients. The fluid may originate from edema, blood debris, and ischemia in the subcutaneous tissues. When drainage is present, the wound is at a higher risk of developing infection (
1,
2). Infection is more likely to occur in patients with poor vascularity of the soft tissues, diabetes, immunosuppressive disorders, malnutrition, steroid use, and in obese patients with large subcutaneous tissue planes exposed during surgery (
3,
4).
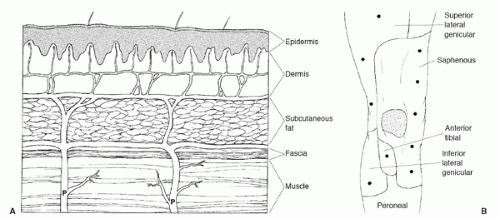
Surgical technique can affect the vascularity to the skin and subcutaneous layer. Ideally, the skin incision is placed in close proximity to the arthrotomy incision to avoid elevating soft tissue flaps. However, prior scars often restrict the location of the surgical incision so that flaps are required to expose the medial retinaculum and permit use of a medial parapatellar arthrotomy. Blood vessels perforate through the fascia to form an anastomosis deep to the subcutaneous layer, which supplies circulation to the subcutaneous tissue and skin (
Fig. 33-1) (
5). Dissection of the subcutaneous tissue should be performed along the subfascial plane between the deepest portion of the subcutaneous layer and deep fascia. If full-thickness skin and subcutaneous soft tissue flaps are dissected from the fascial layer, relatively large flaps can be raised without compromising soft tissue vascularity. If dissection is carried out into the subcutaneous plane and subcutaneous tissue is left attached to the fascia, however, the overlying soft tissue can become devascularized and lead to ischemia or necrosis (
Fig. 33-2).
Wound drainage management depends on the location of fluid accumulation (superficial or deep) and presence or absence of infection (
Table 33-1). Serous drainage originating from edema in the subcutaneous layer does not necessarily represent infection, but the expression of fluid through the surgical incision indicates that the wound is not sealed. Incomplete wound healing indicates that the wound does not provide a complete barrier to contamination from the skin. Sterile dressings should be maintained on the wound and changed daily as often as necessary to collect wound drainage.
When drainage is present, the wound is at risk of developing infection from skin contamination (
1,
2). If the drainage volume decreases daily and clinical signs of infection (fever, erythema, and induration) are absent, however, then the drainage can be treated with dressing changes alone and without antibiotics or surgical debridement. Antibiotics can be used to manage a noninfected draining surgical wound as a prophylactic measure to prevent infection because the wound is incompletely sealed and exposed to skin contamination. However, antibiotic therapy alone for treatment of a deep post- operative infection is not an appropriate method to eradicate infection. If there is a clinical suspicion that deep infection is present and the source of wound drainage is not clear, then use of antibiotics may suppress an infection and make the diagnosis more difficult to establish. Therefore, the distinction between a wound that is not infected and draining from the subcutaneous tissues and one that is infected or draining from the knee joint into the subcutaneous layer is important.