Principles of Lower Extremity Orthoses
Michelle M. Lusardi
Learning objectives
On completion of this chapter, the reader will be able to:
There are many factors to consider when selecting a lower extremity orthosis for individuals with musculoskeletal or neuromuscular dysfunction who have difficulty with mobility and walking. An orthosis may be designed to substitute for impaired muscle performance in the presence of weakness to improve foot clearance in the swing phase of gait.1 An orthosis may be used to provide stance phase stability and support to enhance alignment of limb segments when there is structural instability of one or more lower extremity joints.2 An orthosis may be designed to limit joint motion or unload forces during weight bearing to allow healing after surgery or prevent injury to vulnerable joints.3 For persons with impaired motor control and abnormal tone, orthoses may enhance mobility by minimizing the impact of abnormal movement associated with hypertonicity by positioning limb segments for optimal function.4,5 Alternatively, an orthosis may be used to minimize the risk of development of bony deformity and contracture associated with longstanding hypertonicity, especially in growing children.6 Given the many different reasons that an orthosis might be prescribed, there is no “one size fits all” option: Health professionals must clearly define what they want an orthosis to accomplish, consider its practicality and cost, and sort through the many options available to select the design and components that will best meet the patient’s needs and goals.
This chapter systematically reviews the design, and the pros and cons of ankle-foot orthoses (AFOs), knee-ankle-foot orthoses (KAFOs), and hip-knee-ankle-foot orthoses (HKAFOs) as a means to improve mobility and function for children and adults with neuromuscular dysfunction. We will start with a quick review of the gait cycle and its “rockers” as a foundation for understanding how an orthosis can provide stance phase stability or enhance swing phase mobility. Then we will compare and contrast the various AFO designs, discuss contemporary KAFO components and design, explore traditional HKAFOs and their uses, investigate the clinical use of the parapodium and standing frames, and finally consider orthotic options for reciprocal gait for patients with significant neuromuscular disease or disability. We will apply our growing understanding of lower extremity orthoses in problem-based cases for children and adults with cerebral palsy, hemiplegia following stroke, postpolio syndrome, and spinal cord injury (SCI).
What type of orthosis is best?
When an individual with neuromuscular or musculoskeletal dysfunction has difficulty with mobility and walking, decisions about orthotic options are best made by collaborative interaction within the framework of an interdisciplinary team.7 Members of this team include the person who will be using the orthosis, their family members or caregivers, any physicians involved in his or her care (e.g., a neurologist, orthopedist, or physiatrist), the physical and occupational therapists who are likely to be involved in functional training, and the orthotist who will design, fabricate, deliver, and maintain the orthosis. The combined knowledge and skills of all members of the team ensure that the prescription will best match orthotic design to the patient’s functional needs (Table 9-1).8 If the team is not able to gather in one place as decisions are being made, there must be effective strategies for communication in place so that each team member can contribute his or her unique perspective about why an orthosis is indicated and how the orthosis will facilitate the indiviudual’s functional ability.
Table 9-1
Components of the Preorthotic Prescription Examination Organized by ICF Categories
| ICF Category | Domain | Concerns | |
| Body structure and function | Joint integrity and stability | Ligamentous instability, joint deformity | |
| Range of motion | Soft tissue contracture, joint deformity | ||
| Limb length and alignment | Rotational deformity, unequal limb length | ||
| Muscle length | Fixed versus modifiable contracture | ||
| Overall flexibility | Ability to don/doff; impact of orthosis on trunk, back | ||
| Motor control | Quality of voluntary motion | ||
| Muscle tone | Flaccidity, hypotonicity, hypertonicity, fluctuating tone | ||
| Muscle performance | Strength, power, endurance | ||
| Involuntary movement | Impact on tolerance of orthosis | ||
| Coordination | Ability to don/doff | ||
| Somatosensory function | Ability to detect skin irritation/damage | ||
| Perceptual function | Ability to don/doff | ||
| Upper extremity function | Ability to don/doff | ||
| Postural control, balance | Ability to don/doff | ||
| Visual function | Ability to perform skin checks, donning/doffing | ||
| Cognitive function | Understanding of how to use orthosis | ||
| Cardiovascular endurance | Ability to functionally use orthosis | ||
| Activity level | Gait analysis | Observational | Primary gait problems and compensations |
| Kinematic | Primary gait problems and compensations | ||
| Kinetic | Impact of orthosis on moment throughout gait cycle | ||
| Energetics | Impact of orthosis on physical work of walking | ||
| Assistive device | Safe function with orthosis and assistive device | ||
| Various surfaces | Impact of resistance, unstable surface on gait | ||
| Transitions | Sit to/from stand | Preparing to walk and returning to seated position | |
| To/from floor | Activities on the floor (especially for children/play) | ||
| Managing falls | How to protect self and recover from fall | ||
| Inclines/stairs | Degree of mobility in home and public environment | ||
| Activities of daily living | Donning/doffing | Will assistance be necessary? Who will provide help? | |
| Self care | How will orthosis impact on self-care ability? | ||
| Toileting | Will orthosis need to be removed to use the bathroom? | ||
| Dressing | Ability to manage clothes and shoes | ||
| Participation level | Home | Ability to take part in family activities, roles | |
| School | Mobility in classroom, hallways, outside play areas | ||
| Work | Mobility in entrance, workspace, common areas | ||
| Leisure | Mobility over surfaces, use of tools/devices | ||
| Transportation | Ability to drive, use public transportation | ||
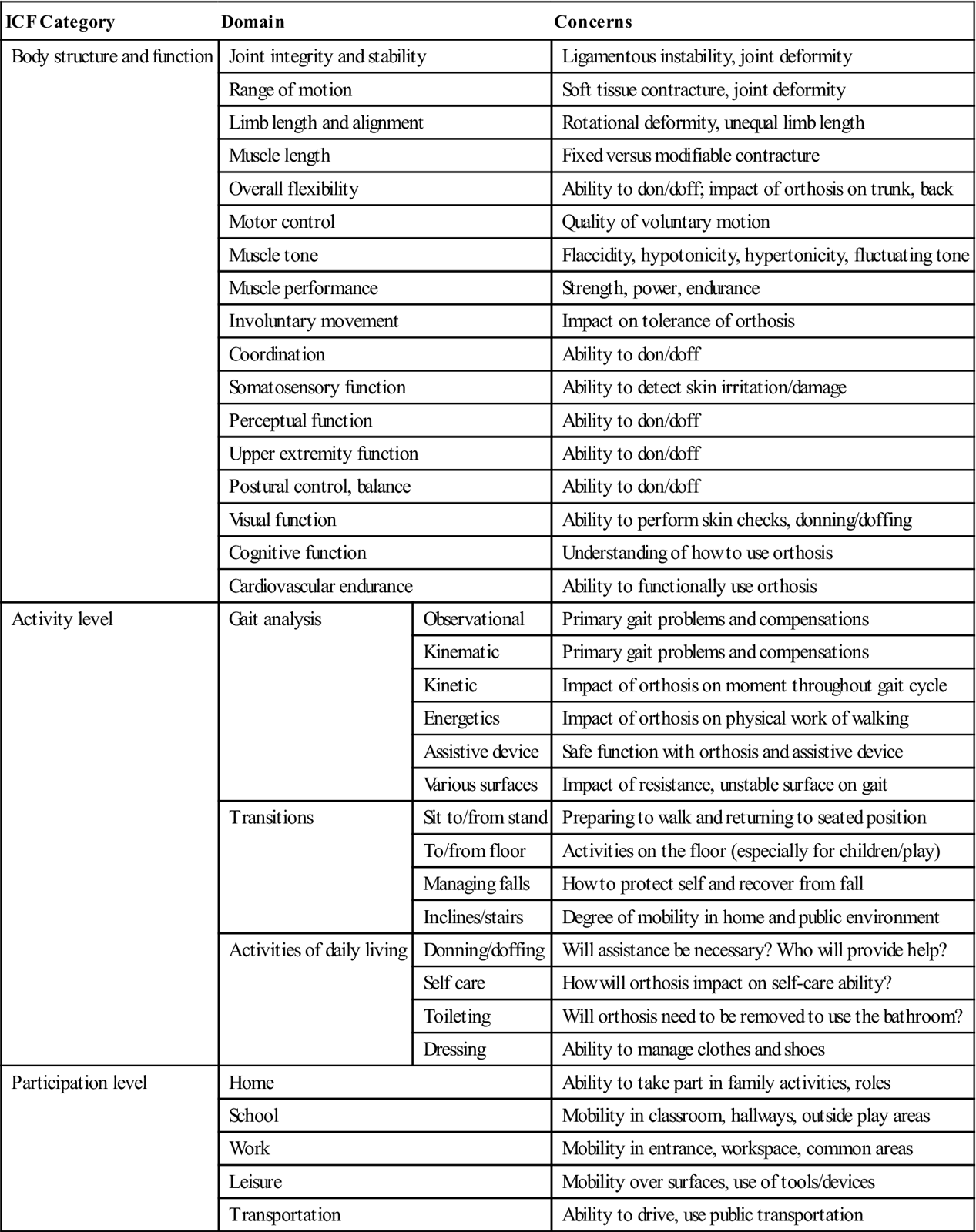
Physical therapists examine the patient to provide information about muscle performance and motor control, range of motion, alignment of the limbs, information about the gait cycle with attention to both primary impairments and the compensation strategies the individual uses while walking, as well as how the orthosis might impact biomechanically on other daily motor tasks (e.g., a child’s ability to get up and down from the floor).9 Physicians bring to the team an understanding of the specific disease or disorder that the patient is dealing with, including the condition’s natural history and likely prognosis, types of secondary musculoskeletal problems that are commonly encountered, and any cognitive, developmental or multisystem involvement that may be associated with the disease.10 Family members and the individual needing the orthosis are concerned with practical issues, such as who will be responsible for applying (donning) or removing (doffing) the device and the ease with which this can be accomplished, as well as information about the types of activities that the individual wants to be involved in while using the orthosis (lifestyle and leisure activities).11 The orthotist uses knowledge of materials and biomechanics, information provided by team and family members, and results of the individual’s physical examination to design and fabricate the orthosis that will best address the mobility problem that needs to be solved.9
The team must not overlook the significant contribution of the individual and caregiver in the prescription process. The use of an orthosis enhances as well as constrains lower limb function; as such, it requires considerable adjustment on the part of the person who will be wearing the orthosis. An understanding of the individual’s or the caregiver’s expectations about what the orthosis will accomplish is a key component of orthotic prescription and training. Discussion and education about what an orthosis will and will not do for the wearer can minimize potential mismatch of expectation versus actual outcome. Acceptance and functional use of the orthosis depends on just how well it meets identified needs and goals, as well as the cost of its use in terms of inconvenience and disruption of lifestyle.12
Careful consideration of the individual’s diagnosis is also critical when selecting materials and designing the orthosis.13 Questions that the team should consider during the decision making process include: Can we reasonably expect that an individual’s musculoskeletal or neuromuscular status is stable and likely to remain the same over time? Does the disease typically have a progressive course, such that decline in function is anticipated over time? Or, as in the case of traumatic injury, will the person’s condition and functional ability improve with time as healing occurs? What can be expected in terms of muscle function and strength, range of motion and joint function, and functional mobility and gait over time? How might growth and developmental status influence future orthotic needs? All of these must be accounted for in the design of the orthosis.
The selection of any orthotic device must include careful consideration of four factors:
Consideration of these four factors guide clinical decision making when comparing and contrasting the various options for lower extremity orthoses. Characteristics of an ideal orthosis are summarized in Box 9-1.
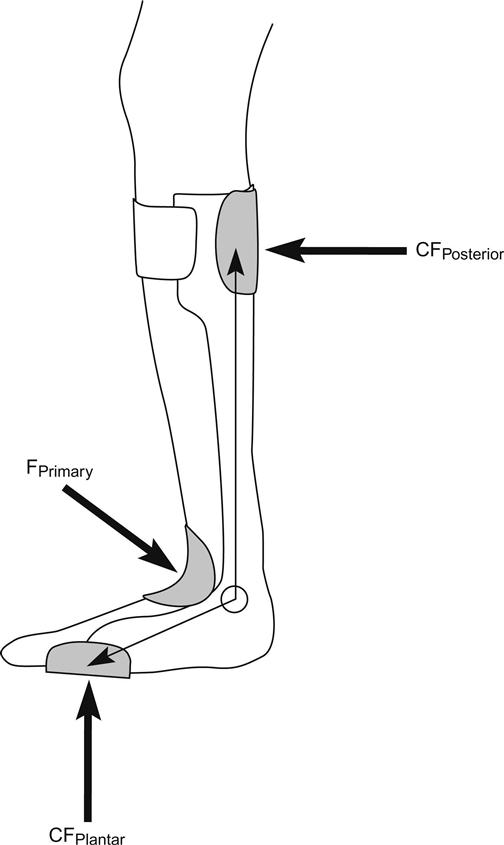
To help an individual use the orthosis most effectively, the physical therapist must understand how the orthosis should fit with respect to its design (i.e., what are the optimal trim lines?) and force control systems (how does it act on the limb segments?) (Box 9-2). Every orthosis uses force applied to the limb to accomplish the goals of its design. An orthosis is most comfortable and effective when (Figure 9-1):
1. The forces are distributed over large surface areas to minimize pressure on skin and soft tissue.
3. The sum of the primary force and opposing counterforces of each control system equals zero.
Determinants of functional gait
There are five factors that influence how well an individual is able to walk.14 The first is stance phase stability: The limb in contact with the ground must be stable enough to support body weight and respond to the ground reaction forces (GRF) as the individual moves through stance phase. The second is clearance in swing: The advancing limb must clear the ground adequately during swing phase to minimize risk of stumbling and trips. Swing limb clearance is influenced by the ability to maintain a level pelvis by stance limb abductor muscle as well as by action of the hip, knee flexors, and dorsiflexors of the swing limb as they relatively shorten the length of the swinging limb. The third is swing phase pre-positioning: By the end of swing, the foot about to contact the ground must be positioned for an effective initial contact and loading response as stance begins. The fourth is adequate step length: There must be adequate motor control and range of motion at the hip, knee, ankle, and forefoot of both limbs so that optimal step length can occur. The fifth is energy conservation: If there are problems with timing, muscle performance, coordination, or postural control during the gait cycle, the energy cost of walking rises substantially, and efficiency of ambulation is compromised.
If neuromuscular or musculoskeletal dysfunction substantially interferes with these determinants, functional ambulation may be an unrealistic goal without an appropriate orthosis. Refer to Chapter 5 for greater detail about characteristics of the normal and pathological gait cycle.
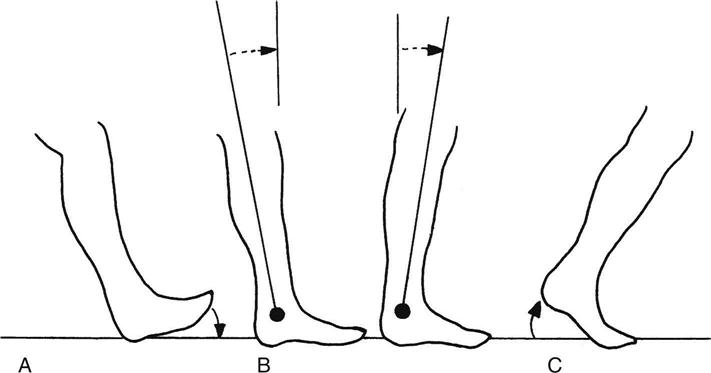
The rockers of stance phase
Orthotists describe three transitional periods, or rockers, during stance phase of walking as the body progresses forward over the foot (Figure 9-2).15 During the first (heel) rocker, there is a controlled lowering of the foot from neutral ankle position at initial contact to a plantarflexed foot flat, as well as acceptance of body weight on the limb during loading response. When motor control and muscle performance is efficient, eccentric contraction of the quadriceps and anterior tibialis prevents “foot slap” and protects the knee as GRF is translated upward toward the knee. In the second (ankle) rocker, the tibia begins to rotate over the weight-bearing foot, from its initial 10 degrees of plantarflexion at the end of loading response, then through vertical into dorsiflexion as midstance is completed. Eccentric contraction of the gastrocnemius and soleus muscles “puts on the brakes” to control the speed of the forward progression of the tibia over the fixed foot throughout midstance. At the start of the third (toe) rocker, the forefoot has converted from its mobile adaptor function of early stance to a rigid lever for an effective late stance, and the heel rises off the ground so that body weight has to roll over the first metatarsophalangeal joint through push-off in terminal stance. During fast walking and running, acceleration occurs as active contraction of the gastrocnemius-soleus complex propels the foot and leg into swing phase.
All lower extremity orthoses provide some degree of external stability to foot and ankle joints; as a result, the smooth transition through the rockers of stance phase is often compromised.16 Disruption of forward progression during stance negatively impacts step length, cadence, and single limb support time.15 The optimal orthotic prescription must balance the need to provide external support with the possible compromise on forward progression and mobility: The orthotist strives to select an orthotic design that provides minimum necessary stability so that mobility will be the least compromised.16 In many instances, modifications of footwear, such as the addition of a cushion heel (which simulates controlled lowering of the foot in loading response) or a rocker bottom sole (which simulates forward progression of the tibia over the foot throughout midstance), can substitute to some degree for the mobility lost when external control is necessary.17 The rehabilitation team must weigh the impact of stability provided by an orthosis on progression through stance and its impact on a patient’s functional status: At times compromise is unavoidable if the patient’s functional deficits are to be addressed effectively.
Prefab, custom fit, or custom molded?
How does the team determine whether an individual would benefit from a relatively less expensive prefabricated orthosis versus a more costly (in both time and money) custom-molded orthosis designed specifically for the person? There are a number of factors to consider in making this decision.
The effectiveness of an AFO is determined by to the intimacy and consistency of its fit. Thermoplastic AFOs can be very effective in controlling a wide range of orthopedic deformities; however, this requires a total contact, intimate fit in all three planes of motion. Intimacy of contact between limb and orthosis is best achieved in custom molded designs.
Mass manufactured, prefabricated orthoses are available in a wide spectrum of orthotic designs, by shoe size, and made of a number different of materials. The degree to which they can be modified or adjusted to fit an individual varies; this may be problematic for persons with foot deformity, extremely wide or narrow feet, or large calf muscles. They are attractive to payers because they are significantly less expensive that custom-fit or custom-molded orthoses. Many rehabilitation professionals, however, are not satisfied with the ability of a prefabricated orthosis to provide optimal external support and control of motion over time: Durability is directly related to the quality of material used and by the lack of intimate fit to an individual’s limb. Even a minimal amount of pistoning or heel elevation within the orthosis during walking can lead to skin irritation or breakdown, and in the presence of hypertonicity, increase of underlying abnormal extensor tone. Therapists may opt to use a trial run with prefabricated orthoses as an evaluative tool to determine which orthotic design might best meet the patient’s needs during the time that a custom orthotic is being prepared or when the patient’s condition requires use of an orthosis for only a short time period.18 Because prefabricated orthoses do not fit the foot intimately, they should be used with extreme caution in persons with neuropathic foot conditions whose ability to perceive soft tissue irritation and damage is compromised.19
Another alternative is an orthosis that begins as a manufactured “blank” that is then custom fit using heating or relieving techniques or the application of additional materials to obtain as close a fit to the individual’s foot and limb as possible. While custom-fit orthoses provide better control than similar prefabricated versions, they are not as effective in terms of fit and function as a custom-molded orthosis.20 Custom-fit orthoses may be appropriate when change in functional status (either improvement or deterioration) is anticipated, such that the orthosis will need to be replaced or adjusted frequently.
Custom-molded orthoses provide the optimal control of the limb and, because of their intimate fit, are especially important for patients with impaired sensation, significant hypertonicity, or risk of progressive deformity associated with their condition. The orthotist constructs the orthosis around a rectified model of the person’s limb, ensuring adequate pressure relief over vulnerable areas (i.e., bony prominences) and building in the desired stabilizing forces based on the orthotic prescription.21 Refer to Chapter 6 for more details about the process of fabrication.
The only true contraindication of a custom-molded thermoplastic design is significantly fluctuating limb size, associated with conditions that lead to edema of the braced extremity.22 When limb size fluctuates, intimacy of custom molded fit is lost: When the limb is at its lowest volume, excessive movement of the limb within the orthosis occurs, compromising orthotic control and increasing risk of skin irritation and damage. When the limb is significantly edematous, the AFO may become constricting, leading to pressure-related problems. For persons with congestive heart failure, advanced kidney disease on dialysis, or other conditions associated with unpredictable fluctuation in limb volume, the total contact of a custom-molded orthosis may be inappropriate, and a conventional double upright orthotic design should be considered.
Appropriate footwear
Whether the decision is to use a prefabricated, custom-fit, or custom-molded orthosis, the ultimate ability of the AFO to meet its therapeutic goals depends on the type and condition of the individual’s footwear.17 Refer to Chapter 7 for more information about key characteristics of shoes worn with an orthosis. Recognition of the need to consider footwear is not always intuitive to the individual, caregivers, or health professionals working on improving the ability to ambulate. It may be necessary for the individual to wear a shoe that is one-half to a whole size larger to accommodate an orthosis; a shoe that is too short or too tight can interfere with the biomechanical function of the orthosis. Shoe closure of an oxford style or athletic shoe (whether tied with laces or closed with Velcro) often provides the diagonally directed force that stabilizes the calcaneus in the heel cup of the orthosis; if the calcaneus moves out of position during walking, the effectiveness of orthotic control is compromised. Loafer type shoes and most sandals do not provide adequate stabilizing forces during the stance phase of gait. While most thermoplastic AFO designs allow individuals to alternate among several pairs of shoes, changing heel heights dramatically alters the biomechanical function of the orthosis. The orthotist and therapist share responsibility for patient and family education about appropriate footwear, monitoring shoe condition to assess impact of wear and tear on its construction and stability, as well as ongoing evaluation of the effectiveness of the orthosis in meeting the individual’s functional needs over time.
Ankle-foot orthoses
AFOs are, by far, the most frequently prescribed device used to control the lower extremity during each phase of the gait cycle for individuals with neuromuscular or musculoskeletal impairments that make walking difficult. It is important to note that the acronyms used to name lower extremity orthoses describe joints that are positioned within the orthosis. In reality, AFOs also effectively address stability of the knee joint (proximal to the orthosis) during stance.23
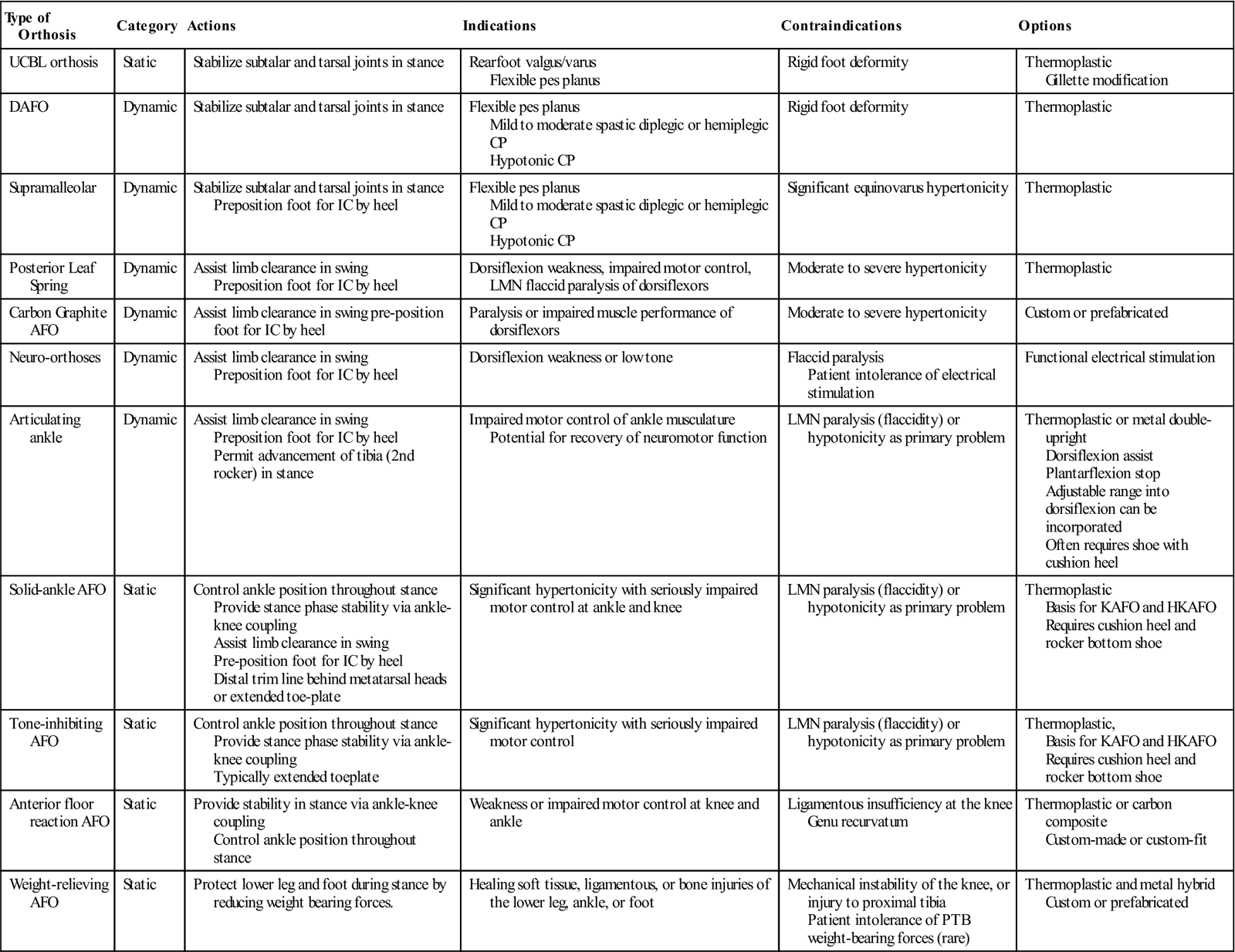
AFOs fall into two categories: static orthoses that prohibit motion in any plane at the ankle (e.g., solid ankle AFO, anterior floor reaction AFO, patellar tendon–bearing/ weight-relieving AFO). In contrast, dynamic orthoses allow some degree of sagittal plane motion at the ankle (e.g., posterior leaf spring or spiral AFOs, articulating ankle AFOs). Whether static or dynamic, the primary goal of an AFO is to provide just enough external support for stability in stance and clearance in swing with minimal compromise of forward progression through the heel, ankle, and toe rockers of gait.16 The actions, indications, and contraindications for the various AFO designs are summarized in Table 9-2.
Table 9-2
| Type of Orthosis | Category | Actions | Indications | Contraindications | Options |
| UCBL orthosis | Static | Stabilize subtalar and tarsal joints in stance | Rearfoot valgus/varus Flexible pes planus | Rigid foot deformity | Thermoplastic Gillette modification |
| DAFO | Dynamic | Stabilize subtalar and tarsal joints in stance | Flexible pes planus Mild to moderate spastic diplegic or hemiplegic CP Hypotonic CP | Rigid foot deformity | Thermoplastic |
| Supramalleolar | Dynamic | Stabilize subtalar and tarsal joints in stance Preposition foot for IC by heel | Flexible pes planus Mild to moderate spastic diplegic or hemiplegic CP Hypotonic CP | Significant equinovarus hypertonicity | Thermoplastic |
| Posterior Leaf Spring | Dynamic | Assist limb clearance in swing Preposition foot for IC by heel | Dorsiflexion weakness, impaired motor control, LMN flaccid paralysis of dorsiflexors | Moderate to severe hypertonicity | Thermoplastic |
| Carbon Graphite AFO | Dynamic | Assist limb clearance in swing pre-position foot for IC by heel | Paralysis or impaired muscle performance of dorsiflexors | Moderate to severe hypertonicity | Custom or prefabricated |
| Neuro-orthoses | Dynamic | Assist limb clearance in swing Preposition foot for IC by heel | Dorsiflexion weakness or low tone | Flaccid paralysis Patient intolerance of electrical stimulation | Functional electrical stimulation |
| Articulating ankle | Dynamic | Assist limb clearance in swing Preposition foot for IC by heel Permit advancement of tibia (2nd rocker) in stance | Impaired motor control of ankle musculature Potential for recovery of neuromotor function | LMN paralysis (flaccidity) or hypotonicity as primary problem | Thermoplastic or metal double-upright Dorsiflexion assist Plantarflexion stop Adjustable range into dorsiflexion can be incorporated Often requires shoe with cushion heel |
| Solid-ankle AFO | Static | Control ankle position throughout stance Provide stance phase stability via ankle-knee coupling Assist limb clearance in swing Pre-position foot for IC by heel Distal trim line behind metatarsal heads or extended toe-plate | Significant hypertonicity with seriously impaired motor control at ankle and knee | LMN paralysis (flaccidity) or hypotonicity as primary problem | Thermoplastic Basis for KAFO and HKAFO Requires cushion heel and rocker bottom shoe |
| Tone-inhibiting AFO | Static | Control ankle position throughout stance Provide stance phase stability via ankle-knee coupling Typically extended toeplate | Significant hypertonicity with seriously impaired motor control | LMN paralysis (flaccidity) or hypotonicity as primary problem | Thermoplastic, Basis for KAFO and HKAFO Requires cushion heel and rocker bottom shoe |
| Anterior floor reaction AFO | Static | Provide stability in stance via ankle-knee coupling Control ankle position throughout stance | Weakness or impaired motor control at knee and ankle | Ligamentous insufficiency at the knee Genu recurvatum | Thermoplastic or carbon composite Custom-made or custom-fit |
| Weight-relieving AFO | Static | Protect lower leg and foot during stance by reducing weight bearing forces. | Healing soft tissue, ligamentous, or bone injuries of the lower leg, ankle, or foot | Mechanical instability of the knee, or injury to proximal tibia Patient intolerance of PTB weight-bearing forces (rare) | Thermoplastic and metal hybrid Custom or prefabricated |
Biomechanical Principles
The biomechanical principles of AFOs are founded on the functional anatomy of the ankle-foot complex. Dorsiflexion and plantarflexion of the ankle are multiplanar (i.e., movement occurs in all three planes of motion) as the talus rotates through the mortise of the ankle in both open chain movement, and when the mortise moves over a relatively fixed (weight-bearing) talus in a closed chain movement.24 The proximal surface of the mortise is shaped by the syndesmosis (fibrous articulation) between the distal tibia and fibula. The medial wall of the talocrural joint is formed by the medial malleolus, a downward extension of the tibia. The lateral wall, formed by the lateral malleolus of the fibula, is both longer and shifted posteriorly. Because of the shape of the articular surfaces of the talus in its mortise and the offset position of the malleoli, the axis of the ankle joint is slightly oblique, running in an anteromedial to posterolateral direction. As a result, dorsiflexion is accompanied by some degree of forefoot pronation and abduction along with hind foot valgus. Plantarflexion is accompanied by forefoot supination with adduction and hind foot varus. Note that during stance, movement occurs in closed chain situation because the foot is fixed on the ground by weight-bearing forces, so that the mortise rolls over the head of the talus.
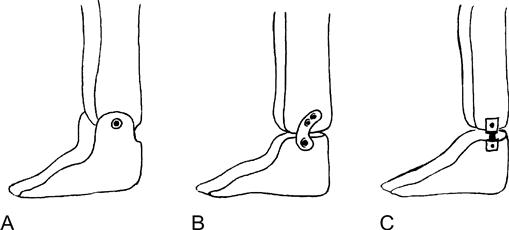
If an AFO has mechanical ankle joints, the axis of the mechanical joints should be aligned as closely as possible to the obliquely oriented anatomical axis of motion (Figure 9-3). The mechanical joint heads are placed at approximately midline of the malleoli in the sagittal plane. This strategy reduces likelihood of abnormal torque and shearing between the orthosis and limb as the individual wearing the orthosis walks. When there is incongruence between the anatomical and mechanical axes, excessive motion of the limb within the orthoses is likely, and action of the mechanical ankle joint is compromised.
Static ankle-foot orthoses
Static AFOs are the most aggressive of the AFO designs in providing external support. They restrict ankle and foot motion is all three planes to provide significant stance phase stability and swing limb clearance. Because of their rigidity, however, these orthoses greatly compromise transitions through the first (heel), second (ankle), and to a lesser degree third (toe) rockers of stance phase. Individuals using static AFOs do better functionally wearing a shoe with a cushion heel and rocker bottom to simulate these key transitions. The decision to recommend a static AFO should be made carefully, weighing the benefit of greater stability against the cost of lost mobility.
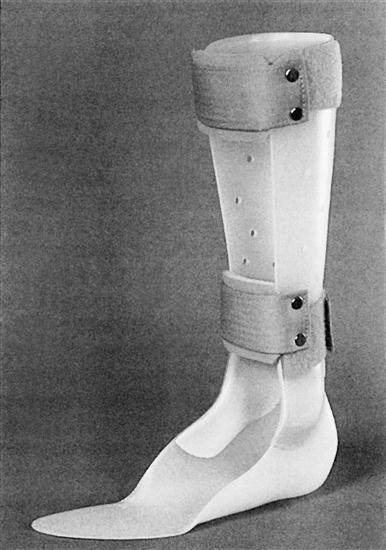
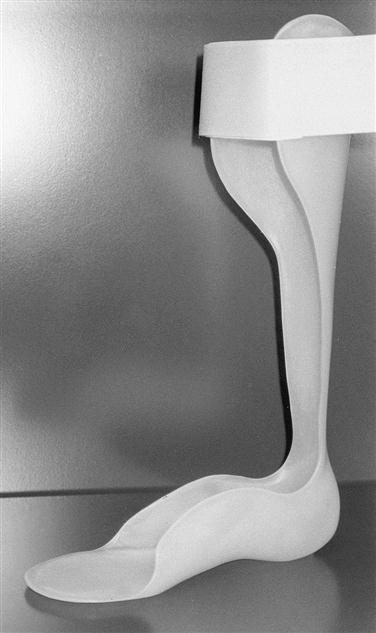
Solid Ankle-Foot Orthoses
The solid-ankle AFO (SAFO), also known as a rigid AFO, is typically fabricated from relatively thick thermoplastic and aims to hold the ankle and foot in as close to biomechanically neutral position (zero degrees of ankle dorsiflexion, subtalar and calcaneal neutral, with a balanced forefoot) as possible given the individual’s functional anatomy.25 The anteroposterior trim line of the SAFO falls at or near the midline of the medial and lateral malleolus (Figure 9-4). Medial and lateral corrugations may be incorporated into the shell of the orthosis to provide additional strength when hypertonicity or excessive weight creates loading forces that require a stronger orthosis. The proximal border is typically trimmed to fall 1.5 inches below the apex of the head of the fibula. The footplate it either trimmed just short of the plantar metatarsal heads or can be lengthened beyond the metatarsal distally into a toe plate if hypertonicity is a concern.26 Some orthotists recommend the addition of a tone-inhibiting bar if hypertonicity is severe.27 There is a tradeoff to consider if the footplate is lengthened: It is much easier to fit into and put on shoes with a shorter footplate; assistance may be necessary to don shoes when the SAFO has a full toeplate.
SAFO Control Systems
There are four distinct control systems incorporated into the SAFO design (Figure 9-5). To resist plantarflexion during swing phase, there is a fulcrum force applied at the anterior ankle (by strapping or by the shoe’s laces or Velcro closure) opposed by a distal counterforce upward under the metatarsal heads and a proximal counterforce at the posterior proximal surface of the AFO. To resist dorsiflexion during stance phase, there is an upward and inward compressive force at the posterior heel, opposed by a distal downward counterforce delivered by the shoe, and a proximal force applied by the anterior closure straps just below the knee. It is important to note that the locked ankle created by an AFO generates an extensor moment at the knee during stance. In this way, a SAFO can substitute for impaired motor control or muscle performance of knee extensors for persons with stroke, cerebral palsy, or other neuromotor dysfunction.
To resist varus and inversion of the foot, a medially directed force is applied just above and below the lateral malleolus with laterally directed counterforces at the proximal medial tibia and the medial foot. To resist valgus and eversion of the foot, there is a laterally directed force applied above and below the medial malleolus, with medially directed counterforces just below the fibular head proximally and at the lateral foot distally.
The degree of control for the foot is also influenced by the position of the trim lines of the foot section. When there is midtarsal joint deformity with forefoot abduction or adduction to contend with, trim lines are adjusted to capture the shafts of the first and fifth metatarsals. If there is too much subtalar valgus, the height of the medial wall is increased, and a flange might be placed proximal to the medial malleolus. These strategies provide greater surface area for distribution of corrective forces applied by the orthosis, so that the patient is more comfortable with the external stability it provides. If knee hyperextension at midstance is a problem for individuals with impaired motor control, the orthotist might fabricate the SAFO set in just a couple of degrees of ankle dorsiflexion, rather than neutral, to minimize excessive extension moment and preserve knee joint health over time. A Gillette modification can be added to the outer medial or lateral surface of the heel cup to influence excessive valgus or varus moment at the knee joint during stance. A medial or lateral post (similar to those used in a biomechanical foot orthosis) can be incorporated into the foot section to equalize forefoot to rearfoot relationships or to enhance biomechanical effects on the knee.
Progression Through Stance Phase
The SAFO biomechanically interferes with transitions through all three rockers of gait in stance phase because of the fixed ankle position inherent in the design.
The orthosis prevents the controlled lowering of the foot that usually occurs in the ankle/first rocker during loading response. If the shoe does not have a compressive cushion heel to mimic controlled lowering, the orthosis propels the tibia rapidly to achieve foot-flat position. The individual wearing the orthosis needs some eccentric ability of the quadriceps to counteract the rapid knee flexion moment that accompanies the SAFOs propulsive force acting on the tibia. This is especially true if the SAFO has been set in a few degrees of dorsiflexion to minimize risk of knee hyperextension in early stance.
The proximal anterior strapping used to hold the limb in the upper part of the SAFO acts with the fixed ankle position to prevent forward progression of the tibia over the weight-bearing foot during the second/ankle rocker that typically occurs during midstance. If the individual’s shoe does not have rocker bottom characteristics, this check of forward momentum compromises effective preparation for push-off and transition from stance into swing phase and necessarily shortens stride length achieved by the swinging limb.
In nonpathological gait, there is 60 degrees of extension at the hallux during the third, or toe rocker of gait. For persons wearing a SAFO with a footplate that extends into a stiff toeplate, the third/toe rocker of the foot will certainly be limited. A shoe with rocker bottom characteristics can assist a smoother rollover when extension of the hallux is limited.
Indications for SAFO
The SAFO design is often selected for individuals with moderate to severe hypertonicity where equinovarus significantly impairs the ability to walk.26,28,29 It may also be used for persons with unpredictable fluctuating muscle tone (athetosis) to provide external stability that makes ambulation possible in the presence of unpredictable variation in antigravity tone.30 While the SAFO has been used in persons with multiple sclerosis with tremor and ataxia, the evidence of its efficacy for improved coordination during walking is limited.31 It may be recommended for persons with significant generalized lower extremity weakness or significant hypotonicity, providing external support as a substitute for impaired muscle performance that would otherwise prevent ambulation.32,33 In both of these circumstances the SAFO is a substitute for severely impaired muscle activity. A custom-molded SAFO has also been used to protect the foot and ankle in the management of persons who need stabilization after foot or ankle surgery, or for those with ankle instability and pain secondary to rheumatoid arthritis.34,35
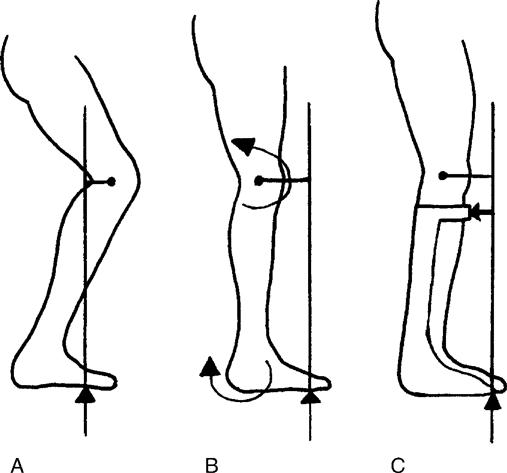
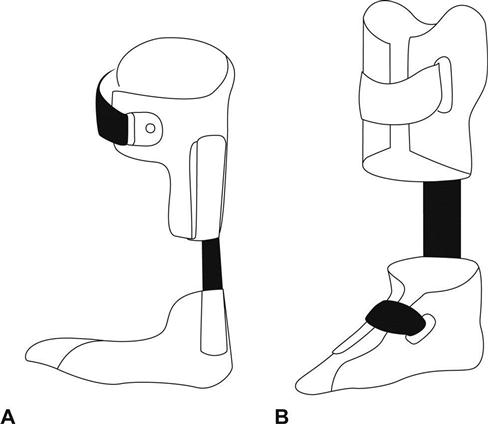
The Anterior Floor Reaction Ankle-Foot Orthosis
All static AFO designs use moments that result from the GRF to provide stability during stance. An orthosis that has evolved from the basic SAFO design to better address impaired motor control of the knee and weakness of the quadriceps is the anterior floor reaction orthosis (FRO)36,37 (Figure 9-6). The FRO is fabricated to hold the ankle in a few degrees of plantarflexion. This restricts the ability of the tibia to roll forward over the foot in the second/ankle rocker of gait, creating an extensor moment that stabilizes the knee during stance (Figure 9-7). If stability is also needed in late stance phase, a stiff toeplate can be added to reinforce the extension moment at the knee. The FRO and SAFO use the same force systems to control foot and ankle position. Whether the FRO is fabricated in a single piece (see Figure 9-7A) or as a SAFO with the addition of a thermoplastic anterior shell (see Figure 9-7B), padding is added where the FRO contacts the proximal surfaces of the tibia to make the extra extension force delivered by the orthosis more tolerable to the wearer.
The FRO is often used for children with cerebral palsy who demonstrate “crouch gait,” or for children with myelomeningocele and persons with postpolio syndrome who have paralysis or weakness at the knee and ankle.36–38 To be efficacious, the FRO relies on a GRF vector that passes anterior to the anatomical knee joint. As knee and hip flexion contractures approach or exceed 10 degrees, the GRF vector nears or passes posterior to the anatomical knee joint, and the FRO is less effective in stabilizing the knee during stance.36 The FRO is contraindicated for persons with notable recurvatum during stance as well as those with cruciate ligament insufficiency; in these circumstances, the extra knee extension moment can further damage joint structure. While the rigid control of ankle and knee enhances mechanical stability in stance, these external restrictions imposed by the FRO may compromise efficacy of postural responses. In those with balance impairment, an ambulatory assistive device (e.g., a cane, Lofstrand crutches, or rolling walker) may be needed for safety, especially if FROs are worn on both limbs.
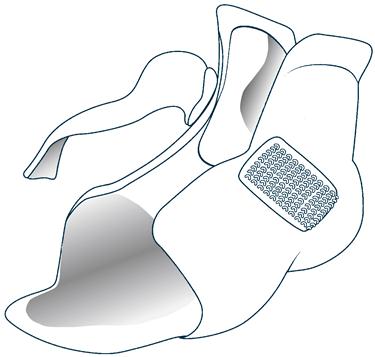
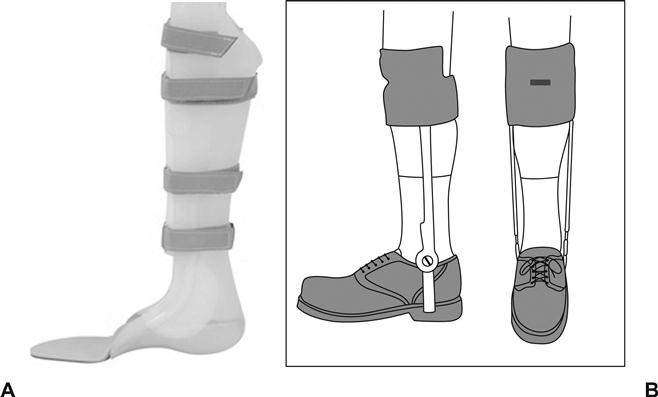
Weight-Relieving Ankle-Foot Orthoses
The weight-relieving AFO, also known as a patellar tendon–bearing AFO (PTB-AFO), incorporates the intimate fit and load-bearing characteristics of a PTB prosthetic socket into a SAFO or traditional metal double upright AFO (discussed later) as a means of offloading or unloading weight-bearing forces during stance phase for individuals with painful, unstable, or recently repaired ankle or foot (Figure 9-8).39–42 The anterior shell of the AFO is modified to accept weight-bearing forces via the medial tibial flare and patellar tendon bar, along with total contact around the upper calf. As with a PTB prosthetic socket, the proximal portion of the PTB-AFO is set in approximately 10 degrees of knee flexion (with respect to vertical) to load some of the body weight onto the anterior shell at the medial tibial flare and patellar tendon bar during stance. This axial force is then transmitted to the ground through the medial and lateral walls of the thermoplastic orthosis, which may be reinforced with metal uprights or through the medial and lateral uprights of a traditional double upright AFO. This strategy effectively reduces axial loading of the ankle and foot during gait.
The weight-relieving AFO is used for persons with Charcot arthropathy, plantar neuropathic ulcers, slowly healing fractures, severe rheumatoid or osteoarthritis of the ankle, surgically repaired ankles after fracture, synovial debridement in hemophilia, and other circumstances that require protection of the foot and ankle when non–weight bearing is not possible. A tibial fracture orthosis and the Charcot restraint orthotic walker (CROW) are adaptations of the weight-relieving AFO; both encase the entire lower limb to provide maximal reduction of axial loading while healing takes place.43,44 Individuals wearing a weight-relieving AFO must have normal anatomical structure of the knee, adequate muscle performance and motor control of the quadriceps muscles for stability in early stance, and sufficient skin integrity to tolerate the loading forces applied by this orthotic design.
Dynamic ankle foot orthoses
Dynamic orthoses allow some degree of sagittal plane motion at the ankle; many permit dorsiflexion during stance phase to facilitate the second/ankle rocker of gait, but restrict plantarflexion during swing phase to facilitate swing limb clearance, incorporating some type of orthotic ankle joint. These dynamic orthoses are available in both thermoplastic and more traditional metal double-upright designs. These are reviewed in order from least restrictive to most supportive designs.
The UCBL Orthosis
In the 1970s, researchers at the University of California Biomechanics Laboratory developed a custom-molded shoe insert, now known as the UCBL orthosis, as an orthotic intervention for subtalar joint instability (Figure 9-9).45 The UCBL controls flexible calcaneal deformities (rearfoot valgus or varus) as well as transverse plane deformities of the midtarsal joints (forefoot abduction or adduction) by “grabbing” the calcaneus and supporting the midfoot with high medial and lateral trim lines; it realigns the calcaneus, improving the angle of pull of the Achilles tendon, providing a more stable foundation for the articular surfaces of the talus, navicular, and cuboid bones.46 The UCBL is also used to improve functional alignment of children and adolescents with flexible pes planus, a longitudinal arch deformity.47 The Gillette modification, an external post positioned either on the medial or lateral border of the heel cup, can be used to apply additional rotatory moments to the calcaneus during weight bearing. In addition to being useful when there is flexible structural malalignment of the rear and midfoot, the UCBL shoe insert may improve foot performance during stance for persons with hypotonicity. It is important to recognize that the UCBL orthosis acts primarily at subtalar and midfoot tarsal joints during weight bearing; it would not be appropriate for persons with swing phase clearance issues, which require the trim line of the orthosis placed above the ankle joint.
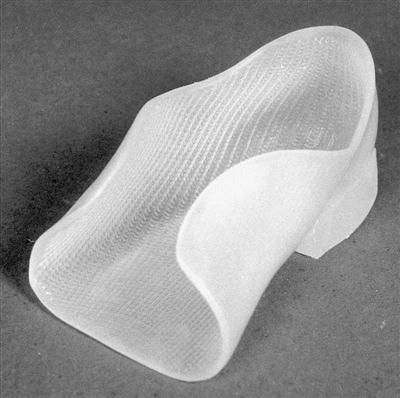
Dynamic Ankle Foot Orthosis
The dynamic ankle-foot orthosis (DAFO), also known as a flexible supramalleolar orthosis (SMO), is a custom-molded orthosis that has evolved from the UCBL shoe insert to better address sagittal plane control of the ankle and foot during stance and to facilitate foot clearance in swing.48 Custom-molded from relatively thin thermoplastic, its proximal trim lines are just superior to the ankle joint, and its distal trim lines encase more of the forefoot than the UCBL (Figure 9-10). By limiting movement of the midfoot and forefoot and by holding the foot in functional position, the DAFO provides a stable base for more effective motor performance and postural control during standing and ambulation.49,50 The DAFO is designed to redistribute plantar pressures of spastic equinovarus from the anterior foot to the heel, perhaps by reducing overall stimulation of reflexes that would otherwise reinforce extensor hypertonicity in children with mild to moderate diplegic cerebral palsy.51 By providing a stable base during stance phase, the DAFO improves swing limb clearance, stride length, cadence, and self-selected walking speed of children with diplegic cerebral palsy, nearly to that of age-matched peers without neuromotor impairment.50,52 Parents of children using DAFOs report improved upright posture as well as enhanced ability of their children to participate in play activities, based on perceived changes in stability, agility, and speed of movement when wearing the DAFO.49 The major complaint about the DAFO was that there was a need to frequently change socks because confinement of the foot within the plastic DAFO shell and shoe contributed to sweaty feet.
Posterior Leaf Spring Ankle-Foot Orthosis
The Posterior Leaf Spring (PLS) AFO is a dynamic thermoplastic AFO designed to accomplish two things53:
The PLS is one of the group of AFOs that provide dorsiflexion assistance. In contrast to the SAFO, medial and lateral trim lines are located well posterior to the midline of both malleoli so that the orthosis is flexible at the anatomical ankle joint (Figure 9-11).54 The degree of flexibility is determined by the thickness of the thermoplastic material used to construct the orthosis and width of the posterior upright in the distal third of the orthosis.54 In custom-molded PLS orthosis, the orthotist tailors the stiffness of the orthosis using the trim line pattern that will best support the weight of the foot during swing as well as the individual’s needs for stability in stance.54
Once the heel contacts the ground at initial contact and loading response begins, the flexible plastic of the PLS serves as a proxy for impaired or absent eccentric activity of the tibialis anterior muscle, slowing but not stopping the foot’s descent toward the ground.53 As stance phase continues, the flexible PSL allows the tibia to roll forward over the weight-bearing foot to accomplish a smooth second/ankle rocker of midstance to terminal stance. As the foot leaves the ground in initial swing, the PLS is able to hold the ankle at the desired neutral 90-degree position, which assists swing clearance and keeps the toes elevated so that next initial contact will be made at the heel. Compared to the stiffness of the SAFO, which makes walking up and down inclines even more challenging than walking on level surfaces, the flexibility inherent in the PLS provides a notable functional advantage.55–57
Owing to its narrow posterior upright and relatively shallow heel cup, a PSL is not as effective in stabilizing the calcaneus and talus during stance as are the SAFO, DAFO, or UCBL designs. This makes it less effective in controlling mediolateral foot position, especially for persons with flexible deformities of the forefoot, midfoot, or rearfoot.58 In these circumstances, the orthotist may opt to place medial and lateral trim lines somewhere between the mid-malleolar position of a SAFO and the narrower PLS to provide additional stability. This modification is sometimes referred to as a semisolid AFO. The modification provides better control of ankle motion, but at the cost of limiting mobility during the second/ankle rocker of gait.59 Note that the flexibility of a PLS and a semisolid AFO make them inappropriate for individuals with significant equinovarus or spasticity of the lower extremity: A high level of abnormal tone will overpower the control systems in these designs.
Additional Dorsiflexion Assist Options
There are a number of commercially available prefabricated as well as custom-molded AFO designs available as alternatives for individuals whose primary need is for dorsiflexion assistance as a substitution for weakness and/or impaired motor control at the ankle. Three of the more frequently used options are reviewed here: (1) Dual Carbon Fiber Spring Orthosis, (2) wearable functional neuromuscular electrical stimulation units, and (3) novel commercially available alternative designs.
Carbon Fiber Spring Orthoses
The Dual Carbon Fiber Spring orthosis (CFO), developed and tested primarily in Germany, is a modification of the traditional PLS design that cuts the PLS into a foot and calf section, then attaches overlapping carbon fiber springs (carbon fiber and Kevlar fibers impregnated with epoxy resin) between the sections (Figure 9-12A).60 Spring resistance is selected based on the individual’s weight. This design aims not only to substitute for impaired or absent anterior compartment muscle activity, but also to enhance the third/toe rocker of stance phase that is typically compromised by thermoplastic AFOs.60 A more powerful push-off is attributed to loading of the spring during early and midstance as the tibia moves forward over the foot, and release of the spring in transition from terminal swing to preswing.61
The CFO design has been adapted to enhance walking ability of children with myelomeningocele and other neuromuscular conditions that contribute to impaired or absent plantarflexor muscle performance.62,63 In this version, the carbon fiber spring is L-shaped (see Figure 9-12B) with its attachment to the foot component (a stiffer version of a supramalleolar DAFO) on the plantar surface rather than posterior heel. The slight distance between the spring and posterior foot section acts as a dorsiflexion stop during stance, allowing some dorsiflexion for second/ankle rocker until the two surfaces come into contact. The proximal carbon fiber spring is fit into a slot in the posterior of a custom-molded section that resembles the upper half of a total contact prosthetic socket. A vertical slot drilled into the proximal spring allows it to slide up and down for several centimeters during stance phase to minimize potential skin friction. This CFO appears to enhance transition through both second/ankle and third/toe rockers of gait, and to provide assistance for push-off. This design has also been incorporated into a knee-ankle-foot orthosis for children who require additional support or control at the knee and hip.64
Both versions of the CFO may require a larger size shoe to accommodate the orthosis in the shoe.
Functional Neuromuscular Electrical Stimulation
For persons with impaired motor control resulting from disease or trauma of the central nervous system, several commercially available, wearable functional electrical stimulation units, also called neuroprostheses, are available (e.g., WalkAide, Hanger Orthopedic Group, Austin, Texas; Odstock Dropped Foot Stimulator, Salisbury, UK; NESS L300 Foot Drop System, Bioness Inc. Valencia, Calif.). The individual wears a cuff that is positioned snugly just below the knee, rather than an orthosis that must fit into the shoe (Figure 9-13). The cuff holds a small stimulator medially with electrodes positioned laterally over motor end points of the peroneal nerve.65 Depending on the model, appropriate timing of the functional electrical stimulation for dorsiflexion activity is determined by a switch worn in the shoe, an inclinometer, or an accelerometer. Most use surface electrodes to deliver the stimulus for muscle contraction although cuffless versions with surgically implantable electrodes are available. Studies evaluating the device have demonstrated improved spatial and temporal characteristics and safety of walking in persons with acute and chronic stroke when worn as an orthosis alone or when integrated with rehabilitation interventions.66–68 Similar findings support its use for persons with traumatic brain injury, multiple sclerosis, and Parkinson’s disease.69–72
Each of these devices must be adjusted to the individual’s typical gait pattern by an orthotist trained to fine-tune the device. To be effective, all of these devices require an intact and healthy peroneal nerve. They would not be appropriate for persons with peripheral nerve injury or neuropathy (e.g., traumatic or compressive dysfunction of the peroneal nerve, Guillain-Barré syndrome, longstanding radiculopathy, lower motor neuron SCI, polio, or postpolio syndrome).
Manufacturers note that such devices are contraindicated in individuals with demand pacemakers or defibrillators, healing fractures, metal implants in the limb, or history of phlebitis; the unit should be used with caution in persons with varicose veins, inflammation in or around the knee, or sensory impairment. While most devices are resistant to splashes, immersion in water during bathing or swimming, or saturation while shoveling snow, for example, will damage the unit, rendering it nonfunctional.
Commercially Available Dorsiflexion-Assist Designs
A number of manufacturers have developed carbon fiber orthoses to provide dorsiflexion assistance at the appropriate times in the gait cycle (e.g., Camp ToeOFF series, Allard USA, Rockaway, N.J.; AFO Dynamic, Ossur Americas, Foothill Ranch, Calif.; Matrix and Matrix Max, Prolaborthotics USA, Napa, Calif.). In contrast to thermoplastic designs, many of these orthoses use a cushioned anterior shin or medial shank piece, held in place by strapping, that transitions into a medial upright and continues into a full footplate (Figure 9-14). These orthoses are designed to pre-position the foot for heel strike at initial contact, substitute for impaired anterior compartment to allow controlled lowering of the foot into foot flat position during the first/heel rocker of loading response, provide some medial-lateral stability during stance while allowing forward progression of the tibial during the second/ankle rocker of stance phase, contribute to push-off in the transition from stance to swing, and support the weight of the foot for effective swing limb clearance.73 Although there is some evidence that these dorsiflexion-assist designs have a positive impact on both the kinematics and energy cost of walking, there have been few published studies that directly compare them with traditional PLS orthoses, or with articulating (hinged) thermoplastic AFOs or traditional metal double upright AFOs with dorsiflexion-assist orthotic ankle joints.73
Hinged Thermoplastic Ankle-Foot Orthosis
The thermoplastic hinged (articulating) ankle-foot orthosis (HAFO) allows sagittal plane motion at the ankle by incorporating a mechanical ankle joint between the foot and calf sections of the orthosis. This variation of the SAFO was designed primarily to allow the tibia to roll over the weight-bearing foot during stance, for a smooth second/ankle rocker, at the same time holding the foot in optimal alignment to control the impact of tone-related equinovarus forces throughout the gait cycle (Figure 9-15). In children with cerebral palsy and in adults after stroke, these orthoses reduce energy cost of walking (compared to barefoot), as well as improve stride length, cadence, and walking speed.74–76 As compared with the SAFO, the HAFO also improves mobility in many functional activities, such as rising from the floor (an important component of play for children), ascending and descending stairs, and walking up or down inclines.56–58 There is some indication that HAFOs lessen the magnitude of abnormal muscle activation associated with spasticity in children with cerebral palsy.77 HAFOs appear to reduce risk of falls in adults with longstanding hemiplegia after stroke, improve static postural control, and have less negative impact on dynamic postural control in standing than SAFOs.78,79 For some children with moderate to severe spastic diplegic cerebral palsy, however, the mobility provided by a HAFO compromises stability in early stance, reinforcing crouch gait pattern, reducing walking speed, and increasing energy cost as compared to a SAFO.74 Multiple perspectives on function, as well as the desired impact on quality of gait, must be considered when deciding which orthosis is best.
The shape, dimensions, and force control systems of the HAFO are almost exactly the same as those of a SAFO, except it has two separate pieces linked by an orthotic ankle joint rather than being a single, solid piece. The HAFO has a larger width at the ankle than the SAFO to accommodate the mechanical ankle joint; this may require larger or wider shoe size to accommodate the orthosis.
Hinged AFOs can be fabricated to allow free motion at the ankle, to allow limited range of motion (i.e., allow dorsiflexion and stop plantarflexion, or the inverse), or to provide some assistance to dorsiflexion, depending on what orthotic ankle joint option motion best meets the individual’s needs and maximizes the resources they bring to the task of walking. A variety of mechanical thermoplastic joints are commercially available (Figure 9-16). Those with true articulations (e.g., the Oklahoma joint) have a single axis of motion that should be aligned as closely as possible to the anatomic ankle joint; other orthotic joints (e.g., the Gillette joint) are flexible and nonarticulating.
Traditional metal orthotic ankle joints have been incorporated into thermoplastic HAFOs as well; These designs are referred to as hybrid orthoses. Simple single axis joints provide mediolateral stability without restriction of available dorsiflexion or plantarflexion; a motion stop can be incorporated if there is need to limit plantarflexion beyond neutral (for stability in early stance) or dorsiflexion (to limit weight bearing on the forefoot in later stance) as the individual’s needs dictate. A bi-channel adjustable ankle joint (also referred to as a double action ankle joint or a double Klenzak joint) (Figure 9-17) can be used to provide assistance and/or limit motion based on an individual’s capabilities and needs for support. If motion assistance is desired, a coil spring is placed in the channel, and a screw is used to adjust compression until the desired level of assistance is achieved. If motion is to be blocked, a solid steel pin is inserted instead of the spring, to stop motion beyond a particular point in the range of motion. Because of its versatility and adjustability, the double action ankle joint is often chosen when change in a patient’s functional status (improvement or deterioration) is anticipated. Orthotic ankle joints such as the Camber Axis Hinge® allow the orthotist to adjust the available range of motion from none (as in a SAFO) through an array of limited anteroposterior stop settings. This would be an advantage when motor control around the ankle and knee is expected to improve over time, for example, in individuals who are recovering from an acute stroke.
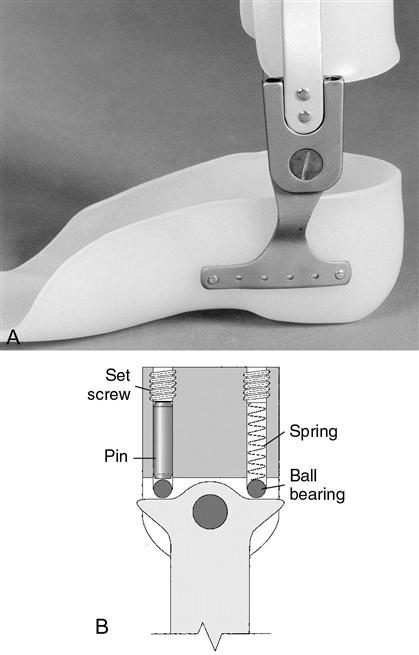
B, The internal anatomy of the double adjustable ankle joint. Ankle joint mobility restrictions (e.g., plantarflexion stop) result from the locations of the pins in the anterior and posterior channels of the orthotic joint. A spring may occupy one of the channels, as depicted here, to assist motion (e.g., dorsiflexion assistance). The ball bearings allow the brace uprights to pivot with ease over the brace stirrup. The set screw can be adjusted to change the relative positions of the rods in each of the channels. (B, From Zablotny CM. Use of orthoses for the adult with neurological involvement. In Nawoczenski DA, Epler ME [eds], Orthotics in Functional Rehabilitation of the Lower Limb. Philadelphia: WB Saunders, 1997. p. 227.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree