Chapter 31 Primary, Double, and Triple Varus Knee Syndromes
Diagnosis, Osteotomy Techniques, and Clinical Outcomes
INDICATIONS
The predominant indication for HTO is lower limb osseous malalignment (Fig. 31-1) in younger patients who have medial tibiofemoral joint pain and wish to maintain an active lifestyle. The goal is to correct the mechanical abnormality of excessive loading of the medial tibiofemoral compartment by redistributing weight-bearing loads onto the lateral compartment. Varus malalignment is present when the weight-bearing line (WBL) crosses less than 50% of the mediolateral transverse width of the tibial plateau.
Unfortunately, a prior medial meniscectomy is a major risk factor for progression of arthritis in these knees. Because any underlying arthritis is expected to progress, it is advisable to perform HTO while the joint damage is in the early stages before the development of severe articular cartilage deterioration and loss of tibiofemoral joint space.52,113
Lower limb varus malalignment in these knees is not overcorrected to valgus when there is no damage to the articular cartilage in the medial tibiofemoral compartment. The goal in these knees is to correct the varus to a neutral alignment and then proceed in a staged manner (if required) with a cruciate and posterolateral reconstruction as required. Correction of the varus alignment decreases the risks of failure of the ligament reconstructive procedures.96,98,99,101
CONTRAINDICATIONS
Major concavity of the medial tibial plateau with loss of bone stock is a contraindication to HTO. On standing 45° posteroanterior (PA) radiographs,121 knees that demonstrate no remaining articular cartilage space to the medial compartment are not candidates. An arthroscopic procedure just before HTO helps to assess the amount of remaining articular cartilage and remove symptomatic meniscus fragments and other tissues.
Critical Points CONTRAINDICATIONS
A relative contraindication is a body weight over 200 pounds (91 kg) (Fig. 31-2). Although there may be some patients in whom HTO is indicated who weigh up to 225 pounds (102 kg), this operation is avoided in patients with a higher body weight because the beneficial effect of unloading the medial compartment will not be achieved.28
A relative contraindication is increased medial slope to the affected medial tibial plateau in the coronal plane due to advanced medial plateau concavity.27 This finding indicates that it will not be possible to significantly unload the medial compartment with HTO, and the joint will remain with all of the weight-bearing confined to the medial compartment. This problem can be tested prior to surgery with varus-valgus stability tests at 30° knee flexion. In these knees with advanced medial arthritis, there is no neutral point in which there is simultaneous contact of the medial and lateral compartments. The tibia behaves like a teeter-totter, with contact alternating between the medial and the lateral compartment and obvious separation of the noncontacted compartment.
The issue of concurrent patellofemoral arthritis has been addressed by prior studies.28,83,123 In general, the symptomatic state should be addressed and the patient warned preoperatively that patellofemoral symptoms might continue or progress. Marked patellofemoral symptoms would contraindicate an HTO.123 The finding of asymptomatic articular cartilage changes to the patellofemoral joint is not a contraindication to HTO, because clinicians have noted that the end result in terms of longevity of the HTO depends on the symptomatic medial tibiofemoral compartment.28,68,93
LOWER LIMB ALIGNMENT: PRIMARY, DOUBLE, AND TRIPLE VARUS KNEES
Critical Points LOWER LIMB ALIGNMENT: PRIMARY, DOUBLE, AND TRIPLE VARUS KNEES
Primary varus: amount of varus angulation due to:
Double varus: amount of varus angulation due to:
Triple varus: amount of varus angulation due to:
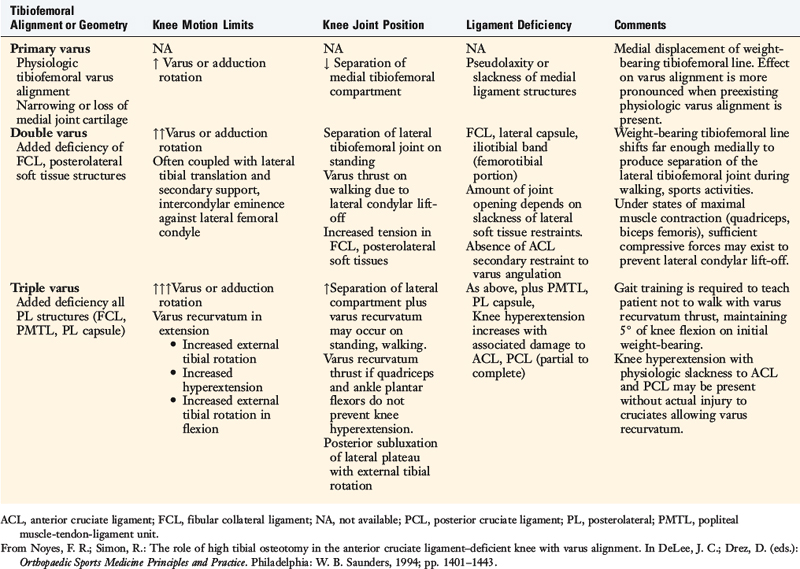
The terms primary varus, double varus, and triple varus knee were devised to classify varus-aligned knees with associated ligament deficiencies (Table 31-1).93 This classification system is based on the underlying tibiofemoral osseous alignment and the additional effect of separation of the lateral tibiofemoral compartment (due to deficiency of the posterolateral structures) on the overall varus lower limb alignment, as calculated from the WBL.
The term primary varus refers to the physiologic tibiofemoral osseous angulation and any further increase in angulation owing to altered geometry (narrowing) of the medial osteocartilagenous tibiofemoral joint (Fig. 31-3). The tibiofemoral WBL shifts into the medial tibiofemoral compartment as the narrowing progresses and the lateral compartment is unloaded. Three degrees of varus angulation approximately doubles medial compartment pressures.36,46
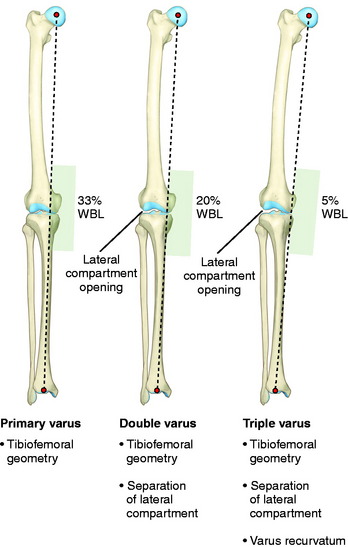
FIGURE 31-3 Schematic illustration of primary, double, and triple varus knee angulation. WBL, weight-bearing line.
As the WBL shifts into the medial compartment, there are increased tensile forces in the posterolateral soft tissues, including the iliotibial tract and ligament structures. There is corresponding separation of the lateral tibiofemoral compartment during standing, walking, and running activities (lateral condylar lift-off).75,125 This is called a double varus knee because the lower limb varus malalignment results from two factors: the tibiofemoral osseous and geometric alignment and separation of the lateral tibiofemoral compartment from deficiency of the posterolateral structures.
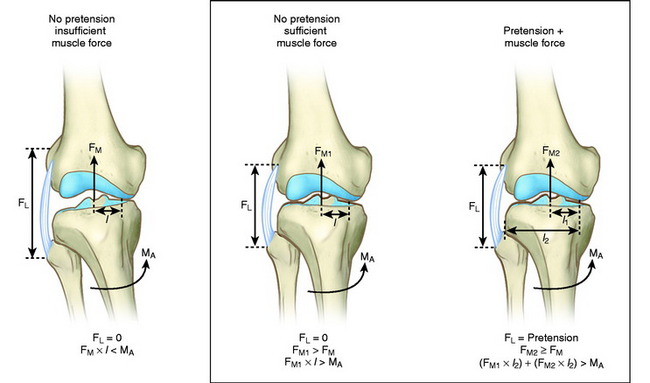
A combination of active and passive restraints resists separation of the lateral tibiofemoral compartment under dynamic loading conditions.45,86 The quadriceps, biceps femoris, and gastrocnemius muscles and iliotibial band act in a dynamic manner to resist adduction moments at the knee joint during gait and, with weight-bearing loads, resist lateral tibiofemoral separation. If these muscle forces do not provide a functional restraint to excessive lateral tensile forces, separation of the lateral tibiofemoral joint occurs.
In the triple varus knee, injury to the FCL and posterolateral structures produces a varus recurvatum position of the limb.54 The triple varus knee results from three causes: tibiofemoral varus osseous malalignment, increased lateral tibiofemoral compartment separation due to marked insufficiency of the FCL and PMTL, and varus recurvatum in extension. The varus recurvatum occurs because of abnormal external tibial rotation and knee hyperextension reflecting deficiency of the posterolateral structures and possibly the ACL. Owing to the increase in lateral compartment opening, the WBL shifts farther medially, as shown in Figure 31-3.
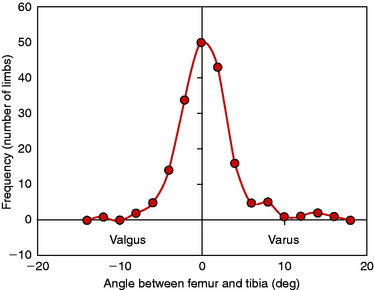
Eckhoff and coworkers36 reported important three-dimensional measurements in 90 individuals (180 limbs) and showed that there is considerable variation in coronal alignment between subjects and between right-left lower limbs (Fig. 31-4). One qualification to the data is that the hip-knee-ankle computed tomography (CT) measurements were obtained under non–weight-bearing conditions.
GAIT ANALYSIS
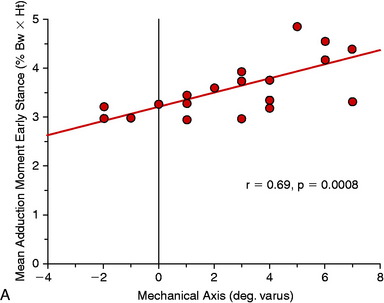
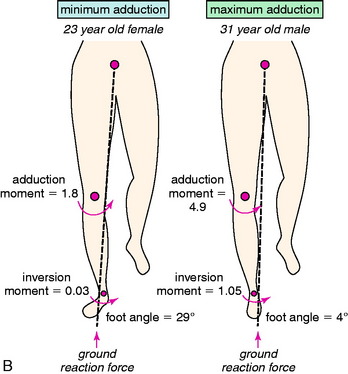
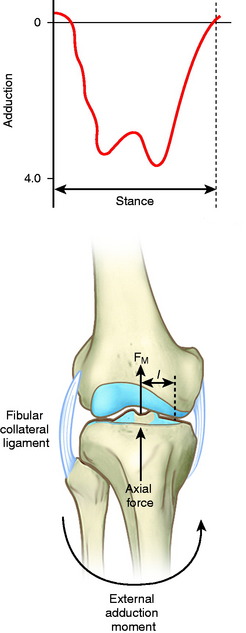
Although a high adduction moment may be anticipated as a result of varus malalignment, the moments and loads on the knee joint cannot be reliably predicted from the static measurement of lower limb alignment on radiographs.109 Many factors in patients with ACL deficiency, varus malalignment, and posterolateral deficiency can be assessed by gait analysis. Abnormal limb alignment, either varus or valgus in the coronal plane or hyperextension in the sagittal plane, produces substantial alterations in the moments and forces about the knee joint (Fig. 31-5).109 The analysis of external moments about the knee during gait allows the clinician to understand the effect of the altered gait dynamics on the knee joint. Abnormally high knee adduction moments increase the risk for progression of medial tibiofemoral arthritis owing to excessive loading.118 The success of HTO has been related to lowering these moments to below-normal values.118,137 In addition, gait analysis allows calculation of abnormally high tensile forces in the lateral soft tissue restraints that increase the risk of elongating these tissues from lateral condylar lift-off with activity. Abnormal tensile loads on posterolateral soft tissues preclude successful FCL and PMTL reconstruction. Markholf and associates76 reported that lateral tibiofemoral compartment loading lateral condylar lift-off had a marked effect on providing joint stability.
Authors’ Study Conclusions
ACL, anterior cruciate ligament; HTO, high tibial osteotomy.
Many studies have documented that the external moments about the knee joint and the corresponding tibiofemoral compartment loads are markedly influenced by individual gait characteristics and adaptations that occur after injury.5,8–11,16,23,62,85,118,137 ACL deficiency may produce marked abnormalities in moments about the knee joint in the sagittal plane, which is further affected by lower limb varus malalignment. Patients with ACL deficiency may show a decrease in the magnitude of the external flexion moment (quadriceps-reduced gait) or an increase in the external extension moment (hamstrings-protective muscle force).6,7 These effects are discussed in Chapter 6, Human Movement and Anterior Cruciate Ligament Function: Anterior Cruciate Ligament Deficiency and Gait Mechanics. The alignment of the foot markedly influences the knee adduction moment. Patients with toe-in, or less than normal external axial rotation of the foot during stance phase, tend to have a higher knee adduction moment as the WBL passes farther medial to the knee joint.4
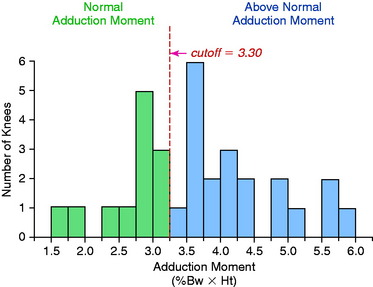
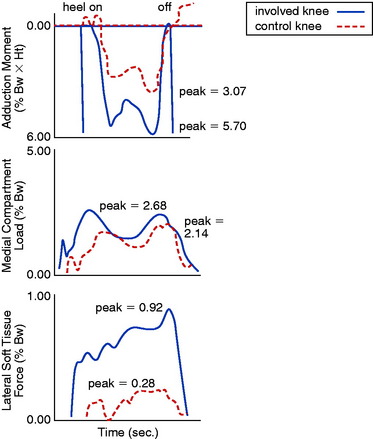
Gait analyses were conducted in a study at the authors’ institution109 involving 32 patients with ACL deficiency and varus angulation. A force plate and an optoelectronic system were used to measure forces and moments of the lower limb and knee joint. Knee joint loads and ligament tensile forces were calculated using a previously described mathematical model.125 Sixty-two percent of the patients had an abnormally high magnitude of the moment, tending to adduct the affected knee (Fig. 31-6). The calculated medial tibiofemoral loads were excessively high in 66% of the patients (P < .01). Forty-seven percent of the patients had predicted abnormally high lateral ligament tensile forces (P < .05). The adduction moment showed a statistically significant (P < .05) correlation to predicted high medial tibiofemoral compartment loads and high lateral ligament tensile forces (P < .01). A shift had occurred in the center of maximal joint pressure to the medial tibiofemoral compartment, with a corresponding increase in the lateral ligament tensile forces to achieve frontal plane stability (Figs. 31-7 and 31-8). If muscle forces are not sufficient to maintain lateral tibiofemoral compressive loads, tensile forces develop in the lateral ligament tissues. The data indicate that, in knees with high lateral ligament tensile forces, separation of the lateral tibiofemoral joint occurs with “condylar lift-off” during weight-bearing.
The magnitude of the flexion moment (which is related to quadriceps muscle force) was significantly lower in 47% of the patients (P < .05), and the extension moment (related to hamstring muscle force) was significantly higher in 50% (P < .05). These findings indicated that a gait adaptation occurred that diminished quadriceps muscle activity and enhanced hamstring muscle activity hypothesized to provide anteroposterior stability of the knee joint.16
The authors99 studied patients with varus-angulated knees with insufficient posterolateral structures in whom prior posterolateral reconstructive procedures failed and an HTO was required before further soft tissue reconstructive procedures could be done. One explanation for these clinical findings is that these knees had a varus or hyperextension thrust during the stance phase of gait, which placed undue tensile forces on the deficient posterolateral structures (Fig. 31-9). Untreated varus malalignment has also been identified as a predisposing cause of failure of ACL reconstructions98,101 and posterior cruciate ligament (PCL) reconstructions96 as well.
CLINICAL EVALUATION
Subjective and Functional Outcome
Patients complete questionnaires and are interviewed for the assessment of symptoms, functional limitations, sports and occupational activity levels, and their perception of the overall knee condition according to the Cincinnati Knee Rating System (see Chapter 44, The Cincinnati Knee Rating System).13
Symptoms of pain, swelling, and giving-way are well-recognized consequences of ACL-deficiency.108 However, in the knee with combined varus malalignment and ACL deficiency, several different knee subluxations may produce symptoms of instability. These include anterior subluxation of the tibia, separation of the lateral tibiofemoral compartment on walking (varus thrust), posterior subluxation of the lateral tibial plateau (with knee flexion and external tibial rotation), and excessive hyperextension or varus recurvatum with a back-knee or feeling of the knee joint going into hyperextension. By history and asking the patient to demonstrate the knee instability, the surgeon must carefully determine the subluxations present.
Physical Examination
A complaint of medial joint line pain may or may not correlate with the degree of medial compartment articular cartilage damage.50,58 In the early stages, the patient usually complains of medial pain that occurs with sports activities, but not with daily activities. When pain occurs with daily activities, it is highly likely that extensive damage exists to the joint articular cartilage. Loss of the medial meniscus is the major risk factor for the progression of arthritis in the medial compartment.37
The physical examination of the knee joint to detect all of the abnormalities in the varus-angulated knee is comprehensive (Table 31-2) and includes assessment of (1) the patellofemoral joint, especially possible extensor mechanism malalignment due to increased external tibial rotation and posterolateral tibial subluxation; (2) medial tibiofemoral crepitus on varus loading, indicative of articular cartilage damage even if not visible on radiographs; (3) pain and inflammation of the lateral soft tissues due to tensile overloading; (4) gait abnormalities (excessive hyperextension or varus thrust) during walking and jogging104; and (5) abnormal knee motion limits and subluxations compared with the contralateral knee.106
TABLE 31-2 Diagnosis of Abnormalities
| Abnormality | Diagnostic Test |
|---|---|
| Tibiofemoral alignment | Full-length standing radiograph: double support (closure of lateral tibiofemoral joint required). |
| Narrowing of medial tibiofemoral joint | Change in millimeters from opposite side on weight-bearing 45° posterior on stress radiograph. |
| FCL insufficiency | Increase in lateral joint opening at 30° of flexion. |
| FCL, PMTL, PL capsule insufficiency | |
| Lateral tibiofemoral joint separation | |
| Varus recurvatum | Standing tests with patient assuming maximal knee hyperextension position provides greatest subluxation. |
FCL, fibular collateral ligament; PL, posterolateral; PMTL, popliteal muscle-tendon-ligament unit.
From Noyes, F. R.; Simon, R.: The role of high tibial osteotomy in the anterior cruciate ligament–deficient knee with varus alignment. In DeLee, J. C.; Drez, D. (eds.): Orthopaedic Sports Medicine Principles and Practice. Philadelphia: W. B. Saunders, 1994; pp. 1401–1443.
Diagnostic Clinical Tests
The medial posterior tibiofemoral step-off on the posterior drawer test is done at 90° of flexion (Fig. 31-10). This test is performed first to identify that the tibia is not posteriorly subluxated, indicating a partial or complete PCL tear. A KT-2000 arthrometer test may be done at 20° of flexion (134 N force) to quantify total anteroposterior (AP) displacement. The Lachman test is performed at 20° of knee flexion. The pivot shift test is done and the result recorded on a scale of 0 to 3, with a grade of 0 indicating no pivot shift; grade 1, a slip or glide; grade 2, a jerk with gross subluxation or clunk; and grade 3, gross subluxation with impingement of the posterior aspect of the lateral side of the tibial plateau against the femoral condyle.
FCL insufficiency is determined by the varus stress test at 0° and 30° of knee flexion (see Fig. 31-10). The surgeon estimates the amount of joint opening (in millimeters) between the initial closed contact position of each tibiofemoral compartment, performed in a constrained manner avoiding internal or external tibial rotation, and the maximal opened position. The result is recorded according to the increase in the tibiofemoral compartment of the affected knee compared with that of the opposite normal knee. This comparison is crucial, and it is important to avoid measuring only the degrees of varus or valgus rotation in the involved knee.
An increase in medial joint opening may occur compared with the opposite knee that represents a pseudolaxity, because the increase is actually due to medial tibiofemoral joint narrowing. When the test is conducted under a varus stress, the medial joint opening returns the limb to a more normal alignment, and there is no true medial ligamentous damage. The true amount of medial and lateral tibiofemoral compartment opening is later confirmed during the arthroscopic examination with gap tests. The primary and secondary restraints that resist lateral joint opening have been described previously.45 The abnormal medial joint opening depends on the knee flexion angle at which the test is conducted and the integrity of the secondary restraints.
Tibiofemoral Rotation Test
The tibiofemoral rotation test was first described by the senior author103 and is used to estimate the amount of posterior tibial subluxation (see Fig. 31-10). The test is conducted in the following manner: (1) the tibia is positioned at 30° of knee flexion, in neutral rotation, (2) the position of the anterior aspect of the medial and lateral tibial plateaus are determined in reference to the femoral condyles by palpation, (3) the tibia is externally rotated to its maximum position, (4) the positions of the medial and lateral tibial plateaus are palpated to determine an abnormal posterior subluxation of the lateral compartment or anterior subluxation of the medial compartment, (5) the examiner observes the location of the tibial tubercle to determine any increase in external tibial rotation compared with the opposite normal knee, and (6) the test is repeated at 90° of knee flexion and may also be conducted by starting at the neutral tibial rotation position and progressing to internal tibial rotation.
Critical Points CLINICAL EVALUATION
Assessment of symptoms and functional limitations with activity: Cincinnati Knee Rating System
Tibiofemoral Rotation (Dial Test)
The advantages of the tibiofemoral rotation test over the traditional posterolateral drawer test55 are (1) the knee may be positioned at varying flexion positions (30° and 90°); (2) the tibia is less constrained because the foot is not held fixed to the examining table; and (3) the axis of tibial rotation can be observed as the tibia is rotated externally and internally. More information is gained when the tibiofemoral rotation tests are performed with the patient in a supine position. In the prone position, it is difficult to palpate the medial and lateral tibiofemoral position required to diagnose the abnormal compartment subluxations. The only indication for the prone dial test is a PCL-deficient knee in which the tibia can be gently displaced to a reduced anterior position during the rotation tests. In the supine position, the tibia can also be displaced anteriorly to prevent posterior subluxation, which makes the interpretation of the dial test more difficult.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree