Lower-extremity amputation secondary to dysvascular disease, including diabetes and peripheral vascular disease, is a major health problem in the United States. Due to the increased comorbidities in this patient population, pre-operative rehabilitation evaluation by a multidisciplinary team is crucial to ensure optimal patient outcomes. This article discusses the key factors that may affect functional outcomes in this patient population and outlines important history and physical examination components that should be evaluated pre-operatively.
The relationship between dysvascular diseases, specifically diabetes mellitus (DM) and peripheral vascular disease (PVD), and amputation risk is well established. Eighty-two percent of all amputations in the United States are due to dysvascular causes. Ninety-seven percent of these are lower-extremity amputations, including transmetatarsal, transtibial (TTA), and transfemoral amputations (TFA). Since 1980, the population of people living in the United States with DM has more than doubled to a current prevalence of 7.7% overall and 18.4% for those over age 65. As the US population ages and the prevalence of dysvascular diseases increases, the number of older dysvascular amputees also will increase. It is predicted that the number of lower-extremity amputations in the geriatric population will rise from 28,000 per year in 2001 to 58,000 per year by 2030. Trends in level of amputation in the dysvascular population also have been changing over the past few decades, with a stronger emphasis on preserving the knee joint, if possible, to improve the probability of successful prosthetic fitting. In a study of major lower-extremity amputations at a large academic medical center on the East Coast, 73% of performed procedures were TTAs and only 26% were TFAs. There seem to be, however, many regional differences regarding the level of amputation trends. In a population-based study done in Minnesota, which examined all lower-extremity amputations in one county over a 20-year period, a 64% TTA rate versus 36% TFA rate was reported. Two other studies reported even lower TTA rates, from 55% to 60%, and TFA rates as 40% to 45%.
General outcomes
Mortality after amputation in dysvascular patients is high. In a retrospective review of 788 patients undergoing major lower-extremity amputation at an academic tertiary center, overall 30-day mortality of 8.6% was reported, but a considerably higher rate of 16.5% was found for those undergoing TFA. At 1 and 5 years after amputation, overall survival of this group was reported at 69.7% and 34.7%, respectively, and again was significantly worse for the TFA population. Similarly, another retrospective chart review of 154 patients at a university hospital and a Department of Veterans Affairs hospital, reported 1- and 3-year survival rates after major lower-extremity amputation as 78% and 55%, respectively. Another study, based solely in the United States veterans population, found a 7-year survival rate of 39%. Conversion rates from TTA to TFA in these studies ranged from 9.4% to 11%. Recent studies have begun to focus on functional outcome for dysvascular patients undergoing amputation. One-year functional prosthetic use rates, ranging from 23% to 77% after major lower-extremity dysvascular amputations, have been reported.
Multidisciplinary approach
The loss of a limb can have significant functional consequences and may lead to the loss of independence for many older dysvascular patients. Proper rehabilitation evaluation and management is crucial to ensure successful outcomes for these patients. Rehabilitation should be focused on improving function for all these patients, maximizing independence, addressing psychological needs related to limb loss, and ensuring that quality of life is maintained. These goals are crucial for patients who are prescribed prosthetic limbs and for patients who will not be able to ambulate with a prosthetic limb. The approach to dysvascular amputees, as for many other rehabilitation populations, requires a skilled multidisciplinary team that participates in evaluation of patients not only post-operatively but also pre-operatively.
Although traumatic amputations often are performed under emergent situations, which preclude significant pre-operative evaluation from a multidisciplinary care team, patients presenting with diabetic foot infections and critical limb ischemia should have a team evaluation. Although some dysvascular patients present with urgent infections that require immediate surgical intervention, in most cases amputations can be delayed until patients have had appropriate evaluations completed. Delay often is necessary to treat any active infection prior to definitive amputation. Dysvascular patients, therefore, can benefit from the expertise of a multidisciplinary team that can initiate an appropriate amputee-focused rehabilitation plan of care based on a patient’s unique biopsychosocial profile. Biologic, functional, social, and psychological factors must be evaluated and discussed with the team, and an appropriate surgical and rehabilitation plan can be developed and discussed with patients prior to amputation.
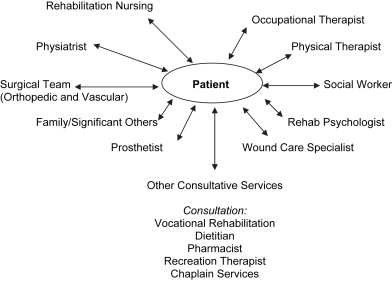
The members of a preoperative amputation team can vary greatly between institutions depending on the resources available and the organization of the institution ( Fig. 1 ). As with all rehabilitation teams, crucial members are physiatrist, physical therapist, occupational therapist, social worker, rehabilitation psychologist, recreation therapist, and vocational counselor. An amputee team additionally needs to include wound care nurse specialists, prosthetists, orthotists, and a surgical team. The members of a surgical team may vary from hospital to hospital but most often include vascular and orthopedic surgeons and podiatrists. Specifically, for dysvascular patients, an evaluation by vascular surgery is crucial to evaluate blood flow with regard to wound healing and to plan any potential revascularization procedures.
Ideally, a team should be involved in the full spectrum of amputation prevention and amputee care once amputation occurs, including foot ulcer prevention, wound care, pre-operative evaluation, surgical care, post-operative care, prosthetic fitting, and lifelong follow-up regarding amputee care. It should be stressed that the role of rehabilitation does not begin post-operatively but must be fully integrated into the continuum of care to ensure quality care and optimal patient outcomes.
The pre-operative process starts with lower-extremity ulcer prevention in patients who are at high risk of foot ulcers related to DM and PVD. Periodic evaluation of sensation and blood flow and identification of biomechanical foot deformities is crucial in prevention of ulcers and eventual amputation. A team working with a primary care provider can help optimize medical status, make appropriate diagnostic referrals, and prescribe appropriate footwear and orthotics.
For patients who develop wounds, evaluation by a wound care specialist to determine the cause of the ulcer and treatment plan is required. Often, to hasten wound healing, non–weight-bearing status is prescribed for patients; in that case, necessary equipment to decrease weight bearing on the affected limb must be prescribed. Patients also may benefit from proper training by a physical therapist to properly use a prescribed assistive device and to demonstrate that they can properly transfer or ambulate without weight bearing on the affected extremity. A team also must take into account the amount of deconditioning that rapidly occurs in this population as a result of limiting weight bearing and prescribe exercise programs that can be accomplished without worsening a foot ulcer. For patients with evidence of ischemia or poorly healing wounds, the involvement of the vascular surgery team is crucial to determine if there are any specific vascular interventions that can be performed to improve blood flow and wound healing. When wounds are not healing and amputation is considered, a physiatrist should evaluate patients (if not already involved in the care of the patients). The prevention of diabetic foot ulcers and the treatment of diabetic infections are discussed in articles by authors, Howard, Miller and Henry, elsewhere in this issue.
Inpatient evaluation of dysvascular patients often revolves around patients with a rapidly worsening infected diabetic ulcer and worsening systemic symptoms or patients with worsening lower-extremity ischemia and rest pain. For these patients, a rapid assessment of the situation is crucial to determining the need for amputation surgery, appropriate level of amputation, pre-operative and post-operative rehabilitation plans, and patient goals. For inpatients and outpatients facing a pending amputation, many factors must be considered in the pre-operative evaluation. Rehabilitation evaluation should not only focus on patients with future prosthetic ambulation potential but also provide treatment of patients for whom ambulation is unlikely. These patients also need rehabilitation interventions to maintain and improve their mobility and activities of daily living (ADL) functions. This article reviews the key factors to evaluate and consider when evaluating dysvascular patients before a potential amputation. The same factors also apply to patients who are evaluated by a rehabilitation team post-operatively.
Multidisciplinary approach
The loss of a limb can have significant functional consequences and may lead to the loss of independence for many older dysvascular patients. Proper rehabilitation evaluation and management is crucial to ensure successful outcomes for these patients. Rehabilitation should be focused on improving function for all these patients, maximizing independence, addressing psychological needs related to limb loss, and ensuring that quality of life is maintained. These goals are crucial for patients who are prescribed prosthetic limbs and for patients who will not be able to ambulate with a prosthetic limb. The approach to dysvascular amputees, as for many other rehabilitation populations, requires a skilled multidisciplinary team that participates in evaluation of patients not only post-operatively but also pre-operatively.
Although traumatic amputations often are performed under emergent situations, which preclude significant pre-operative evaluation from a multidisciplinary care team, patients presenting with diabetic foot infections and critical limb ischemia should have a team evaluation. Although some dysvascular patients present with urgent infections that require immediate surgical intervention, in most cases amputations can be delayed until patients have had appropriate evaluations completed. Delay often is necessary to treat any active infection prior to definitive amputation. Dysvascular patients, therefore, can benefit from the expertise of a multidisciplinary team that can initiate an appropriate amputee-focused rehabilitation plan of care based on a patient’s unique biopsychosocial profile. Biologic, functional, social, and psychological factors must be evaluated and discussed with the team, and an appropriate surgical and rehabilitation plan can be developed and discussed with patients prior to amputation.
The members of a preoperative amputation team can vary greatly between institutions depending on the resources available and the organization of the institution ( Fig. 1 ). As with all rehabilitation teams, crucial members are physiatrist, physical therapist, occupational therapist, social worker, rehabilitation psychologist, recreation therapist, and vocational counselor. An amputee team additionally needs to include wound care nurse specialists, prosthetists, orthotists, and a surgical team. The members of a surgical team may vary from hospital to hospital but most often include vascular and orthopedic surgeons and podiatrists. Specifically, for dysvascular patients, an evaluation by vascular surgery is crucial to evaluate blood flow with regard to wound healing and to plan any potential revascularization procedures.
Ideally, a team should be involved in the full spectrum of amputation prevention and amputee care once amputation occurs, including foot ulcer prevention, wound care, pre-operative evaluation, surgical care, post-operative care, prosthetic fitting, and lifelong follow-up regarding amputee care. It should be stressed that the role of rehabilitation does not begin post-operatively but must be fully integrated into the continuum of care to ensure quality care and optimal patient outcomes.
The pre-operative process starts with lower-extremity ulcer prevention in patients who are at high risk of foot ulcers related to DM and PVD. Periodic evaluation of sensation and blood flow and identification of biomechanical foot deformities is crucial in prevention of ulcers and eventual amputation. A team working with a primary care provider can help optimize medical status, make appropriate diagnostic referrals, and prescribe appropriate footwear and orthotics.
For patients who develop wounds, evaluation by a wound care specialist to determine the cause of the ulcer and treatment plan is required. Often, to hasten wound healing, non–weight-bearing status is prescribed for patients; in that case, necessary equipment to decrease weight bearing on the affected limb must be prescribed. Patients also may benefit from proper training by a physical therapist to properly use a prescribed assistive device and to demonstrate that they can properly transfer or ambulate without weight bearing on the affected extremity. A team also must take into account the amount of deconditioning that rapidly occurs in this population as a result of limiting weight bearing and prescribe exercise programs that can be accomplished without worsening a foot ulcer. For patients with evidence of ischemia or poorly healing wounds, the involvement of the vascular surgery team is crucial to determine if there are any specific vascular interventions that can be performed to improve blood flow and wound healing. When wounds are not healing and amputation is considered, a physiatrist should evaluate patients (if not already involved in the care of the patients). The prevention of diabetic foot ulcers and the treatment of diabetic infections are discussed in articles by authors, Howard, Miller and Henry, elsewhere in this issue.
Inpatient evaluation of dysvascular patients often revolves around patients with a rapidly worsening infected diabetic ulcer and worsening systemic symptoms or patients with worsening lower-extremity ischemia and rest pain. For these patients, a rapid assessment of the situation is crucial to determining the need for amputation surgery, appropriate level of amputation, pre-operative and post-operative rehabilitation plans, and patient goals. For inpatients and outpatients facing a pending amputation, many factors must be considered in the pre-operative evaluation. Rehabilitation evaluation should not only focus on patients with future prosthetic ambulation potential but also provide treatment of patients for whom ambulation is unlikely. These patients also need rehabilitation interventions to maintain and improve their mobility and activities of daily living (ADL) functions. This article reviews the key factors to evaluate and consider when evaluating dysvascular patients before a potential amputation. The same factors also apply to patients who are evaluated by a rehabilitation team post-operatively.
History
As in all patient evaluations, accurate, detailed history of patient condition is crucial to developing accurate assessment and recommendations. Key components of patient history as related to potential amputation are discussed later and outlined in Table 1 .
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






