Fig. 1.1
Plain film image demonstrating geographic pattern in eosinophilic granuloma of the skull

Fig. 1.2
Plain film image showing peripheral sclerosis in a metaphyseal fibrous defect of the upper end of the tibia
Fig. 1.3
Fibrous dysplasia in the upper end of a femur with a sharp line of demarcation (arrow)

Fig. 1.4
Giant cell tumor of the upper end of a tibia showing no sharp demarcation
The roentgenographic appearance is said to be moth eaten if there are multiple, tiny lucencies admixed with normal appearing bone (Fig. 1.5). This appearance suggests an aggressive lesion such as lymphoma.
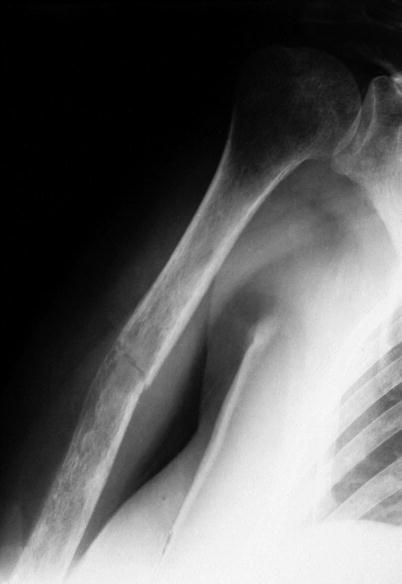
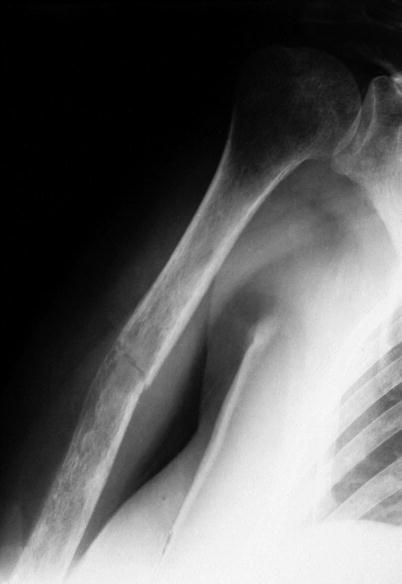
Fig. 1.5
Plain film image: moth-eaten pattern in lymphoma involving humerus, associated with pathologic fracture
Permeative describes a process in which there are multiple tiny lucencies coursing through bone (Fig. 1.6). The appearance may deceptively look like normal bone. Permeative lesions are usually associated with small cell malignancies such as Ewing sarcoma. It has to be remembered that osteomyelitis can present with any of these patterns and suggest a neoplasm.
Fig. 1.6
Plain film image: permeative pattern with multiple tiny lucencies in Ewing sarcoma of femur
Computerized tomograms (CT) are not especially useful except for identifying small amounts of mineral and identifying the nidus of osteoid osteoma (Fig. 1.7a–c). It may also be helpful in anatomically complicated locations such as the spine.
Fig. 1.7
(a–c) Osteoid osteoma in a cervical vertebral lamina. CT scan is helpful in complicated locations such as the spine
Magnetic resonance imaging (MRI) has become routine in the management of bone tumors. The features are generally nonspecific and do not help in diagnosis. But it is the best modality for accurately delineating the extent of a tumor. Measurements are made before chemotherapy is commenced in order to resect the involved segment of bone post-chemotherapy.
Classification
Dr. Lichtenstein presented a classification scheme that has stood the test of time. The tumors are classified depending on the kind of matrix produced or the cytology of the tumor cells in cases without matrix production. The cases are then divided to benign and malignant counterparts.
Classification Scheme
Chondrogenic
Benign: Osteochondroma, chondroma, chondroblastoma, chondromyxoid fibroma
Malignant: Chondrosarcoma and variants
Osteogenic
Benign: Osteoid osteoma and osteoblastoma
Malignant: Osteosarcoma and variants
Hematopoietic
Benign: N/A
Malignant: Myeloma and lymphoma
Fibrogenic
Benign: Desmoplastic fibroma
Malignant: Fibrosarcoma
Smooth Muscle
Benign: Leiomyoma
Malignant: Leiomyosarcoma
Tumors of Unknown Origin
Benign: Giant cell tumor
Malignant: Malignant giant cell tumor, Ewing sarcoma, adamantinoma
Vascular
Benign: Hemangioma
Malignant: Angiosarcoma, hemangiopericytoma
Fibrohistiocytic
Benign: Fibrous histiocytoma
Malignant: Malignant fibrous histiocytoma
Notochordal
Malignant: Chordoma
Lipogenic
Benign: Lipoma
Malignant: Liposarcoma
Neurogenic
Benign: Neurilemmoma
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








