Postsurgical Management of Partial Foot and the Syme Amputation
Edmond Ayyappa and Heather Worden
Learning Objectives
On completion of this chapter, the reader will be able to do the following:
Partial foot and Syme-level amputations present advantages and challenges to the patient and the rehabilitation team. Preservation of the ankle and heel (in partial foot amputation) and most of the length of the lower limb (in Syme amputation) has an important advantage of distal weight-bearing capability: The individual with partial foot or Syme-level amputation is often able to ambulate without a prosthesis if necessary. The prosthesis, however, provides protection for the vulnerable distal residual limb for patients with vascular compromise and neuropathy.
The length and shape of the residual limb present three challenges for successful fitting and prosthetic training for patients with partial foot or Syme amputation: suspension of the prosthesis on the residual limb, distribution of weight-bearing forces within the prosthesis, and attachment and alignment of the prosthetic foot. This chapter defines the most common partial foot and Syme amputations, and reviews the prosthetic management options currently available. Also identified are specific indications and contraindications for the various prosthetic designs.
Partial foot amputations
Until the advent of antibiotics, disarticulation through the joints of the foot reduced the risk of sepsis and shock and improved the prognosis for healing compared with amputations that transected bone. The earliest partial foot amputation was recorded in 434 BC by the Greek historian Herodotus,1 who told of a Persian warrior who escaped death while in the stocks by disarticulating his own foot. He hobbled 30 miles to a nearby town, where he was nursed to health until he could construct a prosthesis for himself. Later he became a soothsayer for the Persian army but ultimately was recaptured by the Spartans and killed.
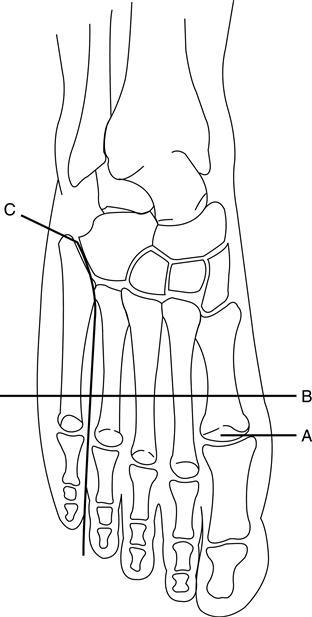
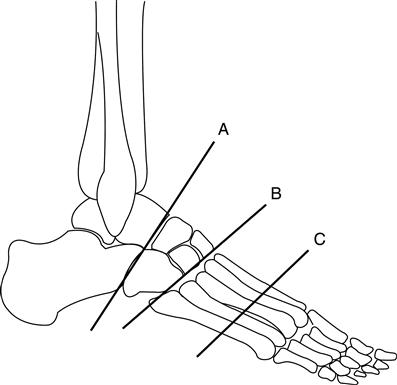
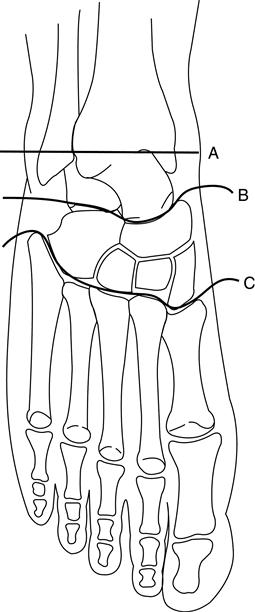
At present, partial foot amputations include a wide variety of ray resections, digit (phalangeal) amputations, and metatarsal transections (Figure 22-1). Midfoot amputations include surgical ablation at the Chopart and Lisfranc levels (Figure 22-2).2 Chopart disarticulation involves the talocalcaneonavicular joint and separates the talus and navicular as well as the calcaneus and cuboid.3 Lisfranc disarticulation separates the three cuneiform bones and the cuboid bone from the five metatarsal bones of the forefoot.
The three hindfoot amputations are the Pirogoff, Boyd, and Syme. The Pirogoff amputation is a wedging transection of the calcaneus, followed by bony fusion of the calcaneus and distal tibia with all other distal structures removed. In a Boyd amputation, the calcaneus remains largely intact rather than being wedged before arthrodesis with the tibia. Today these amputations are infrequently performed on adult patients. Neither provides an easy fit with a prosthesis. The Boyd amputation has received positive clinical reviews when used in the management of congenital limb deficiencies in children in which the amputated limb is shorter than the sound limb.4,5 In this case, there are usually fewer postoperative complications, such as scarring and heel pad migration, and less susceptibility to the bony overgrowth common in children with congenital limb deficiencies. The Syme amputation is performed more frequently in adults because of the ease of prosthetic management at this level (Figure 22-3). Because of the length of the residual limb in Pirogoff and Boyd amputations, the attachment of a prosthetic foot lengthens the limb when a prosthesis is worn. A heel lift on the contralateral sound limb is usually necessary to counteract this artificially long prosthetic limb.
Proximal partial foot amputations often result in equinus deformities because of muscular imbalance created by severed dorsiflexors and intact triceps surae.6–8 Nevertheless, many individuals with a partial foot amputation function extremely well. In one survey, physicians and prosthetists reported that patients with partial foot amputation function better than those with the Syme amputation.9 Although surgeons and prosthetists have long supported the Syme amputation in preference to the Lisfranc or Chopart amputations, many patients with midfoot amputation achieve high levels of function. For example, Jack Dempsey, a professional football player with a midfoot amputation, set several all-time field goal records wearing a custom-designed kicking boot.10
Gait Characteristics After Partial Foot Amputation
A person with a partial foot amputation typically has vascular insufficiency, is usually between the ages of 60 and 70 years, has compromised proprioception and sensation, and has weak lower limb musculature. After a Syme or partial foot amputation a patient may be able to ambulate without a prosthesis but has a loss of the anterior lever arm in ambulation and an inefficient, somewhat dysfunctional gait. The primary need immediately after amputation is to protect the remaining tissue, which is vulnerable to vascular or neuropathic disease. The neuropathic walker developed at Rancho Los Amigos Medical Center locks the ankle in a custom-molded, foam-lined, thermoplastic ankle-foot orthosis (AFO) (Figure 22-4). A rocker bottom is contoured to promote a smooth rollover as a substitute for the second and third rockers of gait, and the orthosis provides optimum protection for the insensate residual foot. For patients with adequate protective sensation, the risk of tissue breakdown is less and a custom shoe insert with in-depth or postoperative shoes often provides adequate protection.
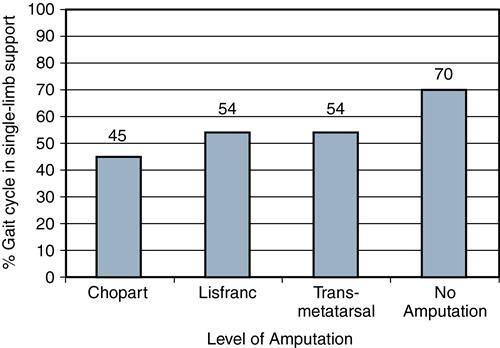
A review of gait in partial foot case histories showed variations in single-limb support time directly related to the reduction of the forefoot lever arm of a partial foot and subsequent increase in the force concentration on the distal end during terminal stance, reflected as reduced time in single-limb support on the limb with amputation (Figure 22-5).11
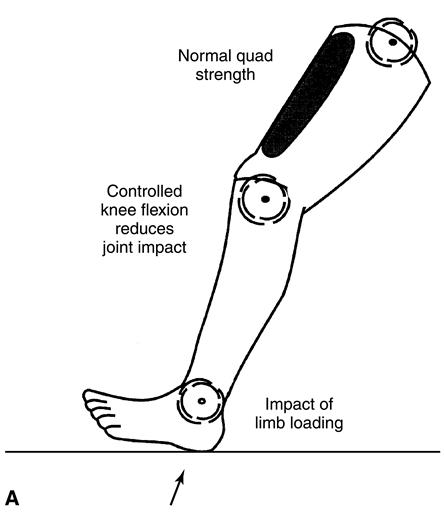
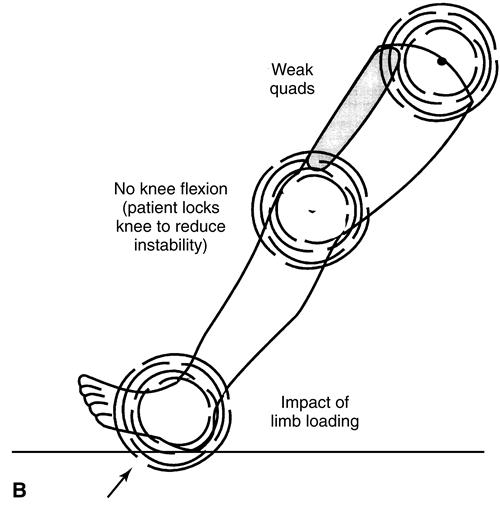
In a person with a whole foot, a fully intact anterior lever arm preserves elevation of the center of mass at terminal stance. With normal quadriceps strength and eccentric control, slight knee flexion (15 to 20 degrees) provides shock absorption as weight is rapidly transferred onto the limb during loading response (Figure 22-6). Most people with dysvascular partial foot and a Syme amputation demonstrate significant weakness of the quadriceps. This functional weakness threatens eccentric control of the usual knee flexion angle that occurs during loading response. To compensate, the patient may keep the knee extended during loading response. This strategy shifts the ground reaction force vector to a position anterior to the knee joint axis, thus reducing the workload of the quadriceps. Although this compensatory strategy enhances early stance phase stability, it sacrifices the shock absorption mechanism at the knee and hip joints, increasing the likelihood of cumulative joint trauma at both joints (see Figure 22-6, B). Neuropathic impairment of proprioception and sensation may further complicate control of the knee in early stance. In addition, compromised forefoot support increases center of gravity displacement. A penalty of higher energy cost results.
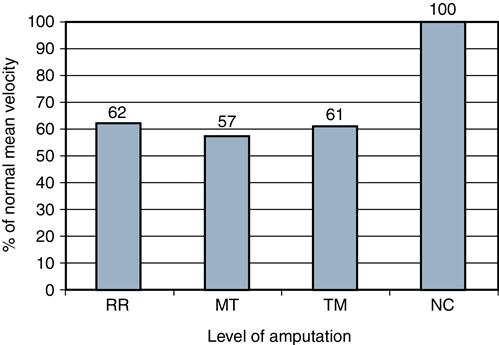
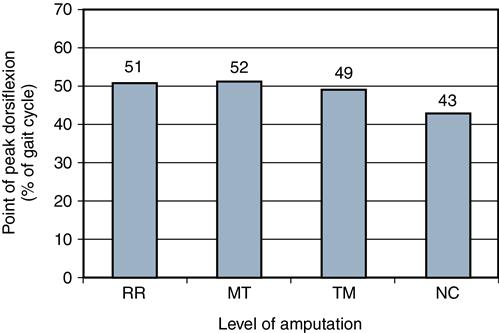
A recent study of the gait of persons with partial foot amputation included 18 patients with transmetatarsal amputations, 11 with one or more metatarsal amputations, 15 with ray resections, and two with either a Lisfranc or a Chopart amputation.11–13 One portion of the analysis focused on the mechanics of the residual limb rockers. Partly because of a delay in the forefoot rocker, patients with all types of partial foot amputations walked with a significantly slower velocity than control subjects with healthy, intact feet (Figure 22-7). Peak ankle dorsiflexion was also significantly delayed for all three partial foot groups compared with those with intact feet. Although the control group with intact lower limbs reached peak ankle dorsiflexion at a point 43% into the gait cycle, patients with partial foot amputation did not reach peak dorsiflexion angle until nearly the halfway point of the gait cycle (Figure 22-8). This delay in reaching peak dorsiflexion subsequently delays forward progression over the shortened stance limb and the transition to double-limb support.
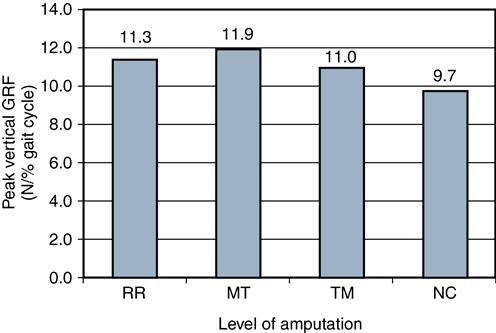
The rise rate of the vertical ground reaction force is the amount of force that occurs in 1% of the gait cycle and can be expressed as Newtons divided by the percent of the gait cycle. After controlling for variation in velocity, the rise rate of the vertical ground reaction force from mid to terminal stance (as the force pattern nears its F2 peak) was significantly lower for all three amputation groups compared with the control group (Figure 22-9). Peak vertical ground reaction forces were significantly higher for the sound limb than the affected limb, likely reflecting an abrupt unloading of the partial foot amputation limb.
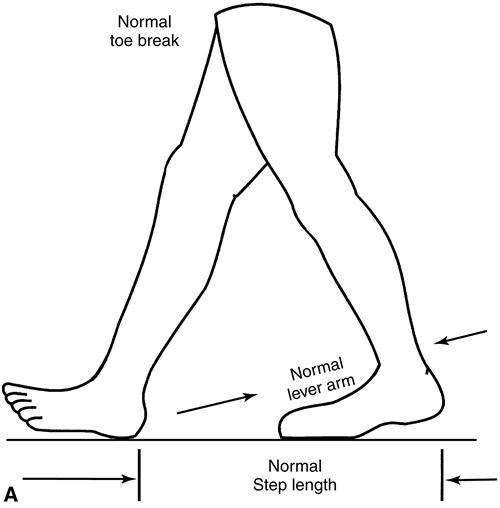
The forefoot lever arm of the trailing limb typically provides anterior support and results in adequate terminal stance support time (Figure 22-10). This results in appropriate step length of the advancing limb. By contrast, inadequate anterior support of the trailing limb of the partial foot amputee reduces the lever arm, resulting in premature toe break and forefoot collapse. The step length of the advancing limb may be correspondingly reduced (Figure 22-10, B).
An inverse relation exists between surface area and peak pressure when body weight is loaded on the foot during stance. This relation is especially important for individuals with partial foot amputation during terminal stance. As the plantar surface area of the supporting forefoot is reduced, the magnitude of the pressure is increased.11–13 The reduced forefoot lever arm also creates abrupt weight transfer to the contralateral side and can reduce step length, stride length, and velocity. Without prosthetic support, the advancing sound-side step length diminishes. Fear, insecurity, and pain aggravated by increased pressure near the amputation site collectively create an abrupt transfer of weight to the sound side, thus increasing the magnitude of the initial vertical force peak.14
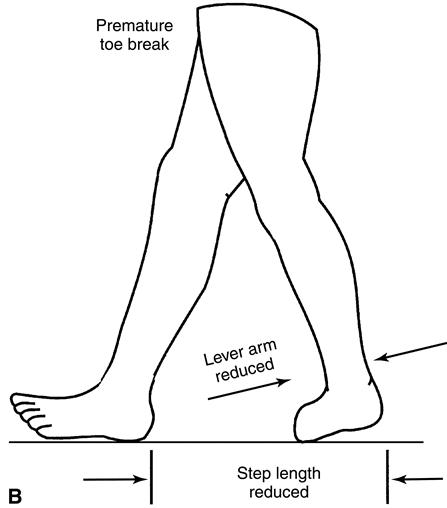
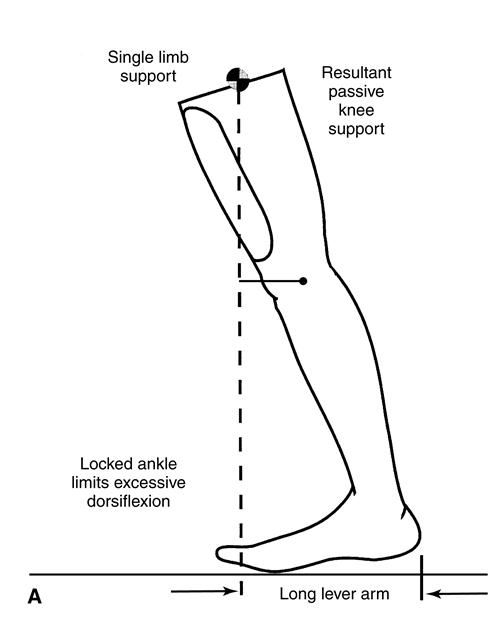
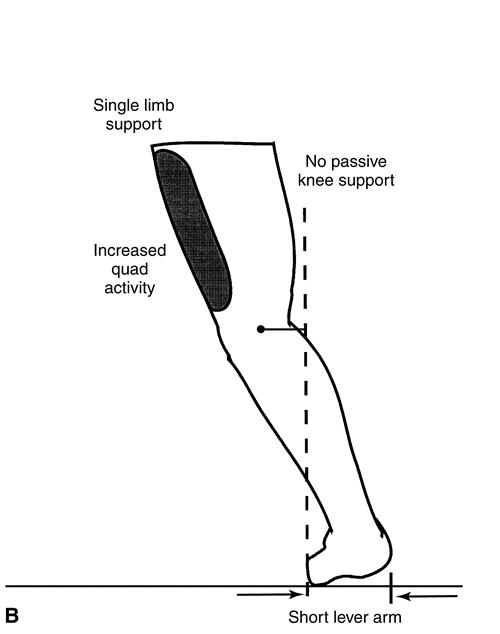
In normal gait, the weight line is positioned more and more anterior to the knee joint as the gait cycle moves from midstance into terminal stance and preswing phases (Figure 22-11). As a result, the limb is held in a passive, energy-efficient extended knee position, effectively supporting body weight and increasing stability in late stance. The length of the forefoot lever arm is one of the key determinants of this support. For persons with partial foot amputation, the lever arm of the foot is greatly reduced, leading to a less-effective, premature loss of support at the end of stance phase. This shorter lever places the ground reaction force closer to or behind the knee in late stance (Figure 22-11, B). Because much of the passive stability provided by a normal forefoot lever in late stance is absent, the quadriceps must contract to maintain stance phase stability, contributing to an increased energy cost of walking for persons with partial foot amputation.
Pinzur and colleagues15 described a functional relation between gait velocity and the level of amputation at the foot. As the amputation level becomes more proximal (as the length of the residual foot decreases), changes in temporal and kinetic gait characteristics include reduced sound-side step length, decreased velocity, increased energy cost, and increased vertical load on the sound side. An inverse relation exists between the length of the remaining portion of the forefoot and the time spent in single-limb support on the amputated side.14 When the level of amputation is proximal to the metatarsal heads, medial support is lost at loading response. This may require orthotic “posting” to limit resultant valgus deformity. Patients with partial foot amputation frequently have plantar flexion contracture develop from muscle imbalance. Any plantar flexion contracture, in turn, increases pressure at the distal residual limb during terminal stance, causing discomfort, pain, and risk of ulceration.16 A contracture is even more problematic for individuals with Hansen disease or diabetic neuropathy because they already have compromised sensation.17,18 Shoes worn without prosthetic replacement of the missing forefoot quickly become disfigured, collapsing at a displaced toe break, further endangering the vulnerable areas of the residual limb.19 The areas of the residual foot most vulnerable to tissue damage during walking include the distal end, first and fifth metatarsal heads, navicular, malleoli, and tibial crest. The longitudinal and transverse arches, the heel pad, and the area along the pretibial muscle belly are pressure-tolerant areas for loading in a custom shoe or prosthesis.
Prosthetic Management
During the 1800 s, digit amputations were fitted by a wood or cork sandal with a leather ankle lacer.20,21 Partial foot amputations were sometimes fitted with a socket and keel fashioned from one piece of carefully chosen root wood, the grain of which followed the curve of the ankle. This was referred to as the natural crook technique. Another commonly used historical design incorporated steel-reinforced leather sockets.22
In recent decades, a wide variety of prosthetic options for individuals with partial foot amputation have emerged. The prescribing physician and patient care team must familiarize themselves with the broad array of options available in prosthetic components and design so that prescription considerations can best accommodate the special needs of each patient. Because of variability in level of amputation, sensitivity or insensitivity of the residual limb, concurrent foot deformity, and patient activity, no single prosthetic prescription can be used for all patients with foot amputation.23 As the amputation level becomes more proximal and the length of the residual foot decreases, prostheses are more likely to incorporate supramalleolar containment or more superior support. This is especially true as a patient’s activity level increases. Commonly used prosthetic approaches include toe fillers placed inside the shoe, a foot orthosis or an arch support, the University of California Biomechanics Laboratory (UCBL) orthosis to control heel position, and a boot or slipper made of flexible urethane resin (Smooth-On, Easton, PA). Cosmetic restoration of silicone and several variations of AFOs are also in common use.
The length and degree of flexibility of the prosthetic forefoot affect the anterior lever arm and consequently foot and ankle motion. The biomechanical goal is to allow anterior support in the area of the lost metatarsals as well as a controlled fulcrum of forward motion as the foot-ankle complex pivots over the area of the lost metatarsal heads in the third rocker of late stance. An additional goal is to minimize pressure at the amputated distal end within the socket or shoe.
Toe Fillers and Modified Shoes
If a simple filler is prescribed, an extended steel shank or band of rigid spring steel should also be placed within the sole of the shoe, extending from the calcaneus to the metatarsal heads. The challenge that faces the prosthetist is to match the appropriate degree of forefoot flexibility to the needs of each patient. For an energy-efficient and cosmetic gait, relative plantar rigidity should give way to at least 15 degrees of forefoot flexibility distal to the metatarsal heads. The extended steel shank is helpful in providing a limited degree of buoyancy that substitutes for the lost anterior support of the foot.24 Stiffening the sole with a spring steel shank increases the lever arm support, but often at the expense of additional pressure on the distal end of the residual limb.25
For a patient with a more complex partial foot amputation, a rocker bottom shoe modification distributes force over a greater area and advances stance more quickly and efficiently. A curved roll or buildup on the plantar surface of the shoe encourages tibial advancement while minimizing weight-bearing pressures on the distal amputated end (Figure 22-12). For optimal function the plantar contour of a rocker bottom should follow a radius originating from the knee joint center but break or roll more abruptly just distal to the metatarsal heads. Although a rocker bottom assists rollover, it also compromises symmetry of gait. It is often prescribed for individuals with chronic pain or in conjunction with a custom-molded accommodative interface for those with a neuropathy-related risk of reamputation. Extra-depth shoes have 6 to 8 mm or more of space inside the shoe on the plantar surface to accommodate an orthotic insert or prosthesis and may be useful for patients with digit or ray amputations.23
Custom-molded shoes, when used in conjunction with a filler and shank, improve the comfort level and reduce the risk of ulceration in many dysvascular patients with amputation. They are not as subject to forefoot collapse, provide major protection to the endangered foot, and may last longer than stock shoes.26
Custom Shoe Inserts and Toe Fillers
A custom-molded, flexible, plantar shoe insert is one of the options for individuals with amputation of the hallux or first ray. This orthotic approach is typically used in combination with extra-depth shoes. The goal is to provide a flexible anterior extension to compensate for a missing or shortened first ray to improve the third rocker and yet support and protect the amputation site during the simulated metatarsophalangeal hyperextension in late stance and preswing.27 This provides some relief for metatarsal head pressure, supports the arch, and probably assists in normalizing the ground reaction force pattern during terminal stance and preswing. It may incorporate a toe filler to prevent premature forefoot shoe collapse.28–30 Toe fillers consist of soft foam material such as room-temperature vulcanized elastomer, which fills the voids in the toe box of the shoe. They provide limited extension of the shoe life and a moderate degree of cosmesis. They also act as spacers, keeping adjoining toes properly positioned and reducing abnormal motion that can otherwise lead to ulceration. The toe filler alone provides limited mechanical advantage. A spring steel shank within the sole of the shoe and extending from midcalcaneus to the metatarsal heads can further improve gait. An alternative to the spring steel shank is a longitudinal support built into a flexible custom insole. Either support device must end at the metatarsal heads to allow hyperextension of the metatarsophalangeal joints. A foot orthotic with arch support and filler is preferable to the simple filler because it can be used in different shoes and because it provides plantar support to an already compromised weight-bearing surface.31 Custom insoles can also be made from a sawdust and epoxy resin instead of foams and thermoplastics.
The UCBL orthosis, a foot orthosis that encapsulates the calcaneus, was developed at the UCBL during the 1960s and was comprehensively described in 1969.32,33 The UCBL orthosis is designed to provide better control of subtalar and forefoot position than are custom-made shoe inserts, reducing motion and thus friction with a closer fit or purchase over the calcaneus and forefoot (Figure 22-13).34 The UCBL orthosis design can be effectively incorporated into a custom orthosis and filler for persons with partial foot amputation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree