Postoperative Treatment Adjuncts
Bernard F. Morrey
CHAPTER 40A: BRACES
RATIONALE
The most common complication of elbow injury and with some arthritic conditions is stiffness. The accepted principle to avoid this after a fracture is rigid fixation. Early motion has also been used to decrease this sequela after fractures and injury at the elbow (see B. Continuous Passive Motion [CPM] below). In spite of these measures, because of limitations imposed by the injury or in executing the ideal treatment, and due to the inherent biology and response to injury, stiffness of the elbow is a common problem (1,2). Unfortunately, the use of aggressive physical therapy to address posttraumatic stiffness is not always successful and, in fact, may contribute to making the contracture worse.
PATHOLOGY OF ELBOW CONTRACTURE
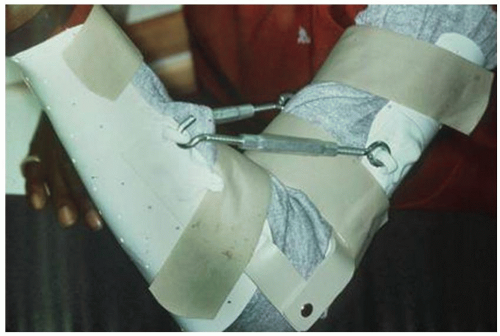
Ankylosis develops from contracting scar tissue as a response to insult, but also is now being recognized to be a function of individual host genetic variation. The goal of splint treatment is to stretch the soft tissues, thus maintaining the length of the capsule and ligaments. The question then arises as to the best method of providing a force to stretch the periarticular soft tissues: dynamic or static adjustable splinting. Initial efforts to mechanically stretch the contracted tissue involved custom turnbuckle braces (Fig. 40A-1). Today, clever dynamic, low-profile devices have been designed and have gained considerable popularity. The selection of one program over the other is dependent on one’s philosophy and interpretation of the concepts of wound healing and contracture (3), and goals of splint usage (4,5 and 6). Even today, clinical studies do not reveal superiority of one over the other (7).
MANAGEMENT OF ELBOW STIFFNESS
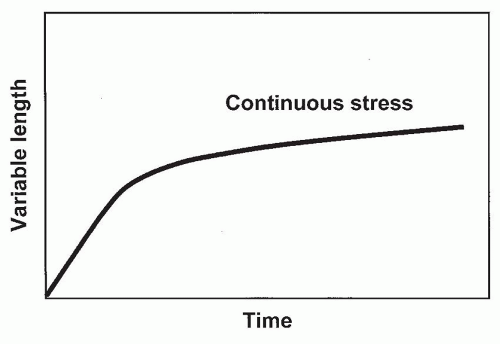
Dynamic Splinting
Because dynamic splints are readily available (Fig. 40A-2), this method is probably the most popular means of treating impending or established stiffness. The rationale of dynamic splinting is based on considering the elbow capsule as a viscoelastic tissue. The response of such a tissue to a constant force is a deformation, which is called creep (Figs. 40A-3 and 40A-5). However, the constant force may cause irritation of the soft tissue, and hence, inflammation and pain may be associated with dynamic splinting. Nonetheless, this type of splinting remains a commonly employed option for many (6,8).
 FIGURE 40A-2 Commercially available dynamic braces. The tension and excursion may be adjusted by the patient. The designs are attractive and low profile. |
Static Adjustable Splinting
With this approach, a specific force is applied to the elbow that results in a discrete stress being imparted to the tissue (Fig. 40A-4). However, since the splint position is not further altered, the soft tissue is allowed to undergo a process called stress relaxation that occurs over a period of time in response to the fixed position (Fig. 40A-5). It is felt that stress relaxation lessens the likelihood of tissue irritation and of inflammation. Thus, in our opinion, the elbow is more amenable to this type of load application and splint philosophy since it is inflammation that breeds additional swelling and scarring. Although this type of splinting has been documented to be quite effective (9), one recent study suggests both systems work equally well (7). Unfortunately, the application of these principles to enhance forearm rotation, while attempted (Fig. 40A-6), has been less successful. This is because the mechanical advantage required of bracing devices is not available at the forearm.
 FIGURE 40A-4 Current commercially available static adjustable braces. Note the effort to gain mechanical advantage with the “JAS”TM design. |
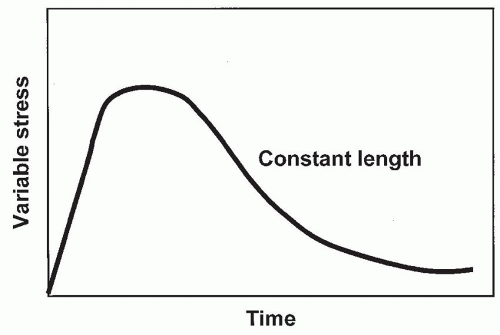 FIGURE 40A-5 Tissue response to a single discrete force results in stress relaxation of the viscoelastic tissue over time. |
INDICATIONS/CONTRAINDICATIONS
Indications
The indication for elbow splint therapy is the presence of a flexion or extension contracture that is amenable to stretch deformation. Experimental data (2) and clinical experience suggest tissue may respond to this type of therapy in three stages as follows (9): (a) onset to 3 months from injury, highly effective; (b) 3 to 6 months, moderately successful; and (c) 6 to 12 months, variably effective. A stable articulation and a reasonably intact articular surface are prerequisites for splint therapy to be effective in any of these stages.
Contraindications
Poor-quality skin that does not tolerate the constant forces from the splint
Excessive or increasing swelling can also cause the development of neural symptoms that require splint discontinuance or program alteration as follows: sensory—alter the pressure points; motor—alter basic program or discontinue. Regardless of the type of splinting, the clinician must be assured that exerting force across the joint causes considerable increased joint contact stresses (11).
STATIC ADJUSTABLE SPLINTS
At the present time in the authors’ practice, a single brace is used to attain full extension and flexion (Fig. 40A-7). With traditional humeral-based support, the stabilizing humeral strap tends to cause the soft tissue to “bunch up” in flexion, which limits further flexion. This problem is less an issue when an extension torque is applied.
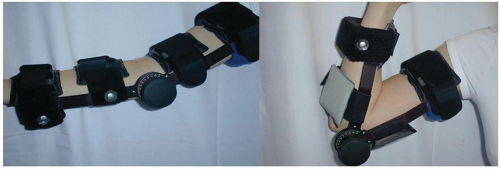 FIGURE 40A-7 A static adjustable brace currently used by the author in which the force is directly applied to the axis of rotation. |
Application
The Mayo brace is applied with the hinge aligned to the elbow flexion axis. Any brace used should have broad surfaces to designate force at the wrist and forearm. All braces come with specific application instruction.
The precise use is described below in a format designed to be individualized and given to the patient. In all instances, the patient assumes responsibility for the use of the brace.
GENERAL PATIENT INSTRUCTIONS FOR THE USE OF STATIC ADJUSTABLE BRACES
The following general guidelines are given to the patient for the use of the static adjustable brace and should be modified depending on individual needs and progress.
I. General Goals
To attain improved motion of the elbow, inflammation must be avoided. This is done with the use of the anti-inflammatory agents, heat and ice, and education of the patient to the signs of inflammation.
II. Cardinal Signs of Inflammation
Increased soreness, increased discomfort with use, swelling, or, commonly, a progressive loss of motion rather than improvement from day to day
III. Treatment of Inflammation
Avoid the causative factor. Be less vigorous with torque and duration: Adhere to the heat/ice program, and take anti-inflammatory agents as prescribed. If this seems inadequate, the program may need to be modified. Check with your doctor.
IV. Direction of Improvement
Often, both increased elbow flexion and extension are being sought. In general, the motion that is needed most is addressed at night as well as during the day. The opposite motion is encouraged during the day.
V. Typical Splint Program (20-Hour Program, 0 to 3 Weeks from Injury or Surgery) (Table 40A-1)
Morning. Upon rising in the morning, remove the splint. Gently flex and extend the elbow while taking a hot bath or shower for approximately 15 minutes. Take anti-inflammatory agent.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree