Posterior Tibial Tendon Dysfunction
Alan R. Catanzariti
Robert W. Mendicino
Michael P. Maskill
The adult acquired flatfoot deformity (AAFD) is one of the most common disorders seen by foot and ankle specialists. Posterior tibial tendon dysfunction (PTTD) is the most common etiology of this disorder. Treatment options vary and depend on training and individual experience. Increased recognition of the stages of development and sequence of symptoms associated with the dysfunctional posterior tibial tendon has resulted in improved patient outcomes. Despite enhanced diagnostic skills and a focus on early recognition, controversy still exists as to which methods of surgical intervention provide optimal results.
PTTD has been attributed to numerous factors. Although originally associated with obesity in middle-aged women, it more recently has been considered as a gradual degenerative process. PTTD is a progressive disorder that results in a dynamic sequence of events, producing a broad range of symptoms and deformity. The spectrum of pathology varies from tenosynovitis without significant intratendinous disruption to complete tendinosis and/or eventual rupture. The resultant deformity of the subtalar and transverse tarsal joints varies in degree and flexibility.
FUNCTIONAL ANATOMY AND PATHOPHYSIOLOGY
The posterior tibial muscle-tendon unit is the dynamic stabilizer of the hindfoot. The PTT passes posterior to the medial malleolus and medial to the subtalar joint (STJ) axis. It functions as a pulley to dynamically stabilize the medial longitudinal arch, plantarflex the ankle, and supinate the foot through the STJ (1). STJ inversion locks the midfoot and prevents a pronatory moment through the oblique axis of the midtarsal joint (MTJ). A loss of this function creates a mechanical overpull from the peroneus brevis (PB) tendon, forcing the hindfoot into a valgus position. This results in spring ligament and deltoid ligament attenuation that enables the talus to plantarflex and adduct. Plantarflexion and adduction of the talus unlocks the MTJ complex causing further instability and deformity.
A flatfoot is characterized by abduction and supination of the forefoot with a collapsed medial longitudinal arch and a valgus angulation of the heel. AAFD is most often a result of long-standing posterior tibial tendinopathy.
Radiographic evaluation should include anterior-posterior (AP), lateral, lateral oblique, long-leg axial, and hindfoot alignment views. AP radiographs will demonstrate peritalar subluxation with increased talo-first metatarsal angles. Lateral radiographs will also demonstrate an increase in the talo-first metatarsal angle.
The PTT functions throughout the entire gait cycle. The PTT decelerates subtalar pronation and internal tibial rotation at heel contact and accelerates STJ supination and external rotation of the leg during midstance (1). The short excursion of the PTT, usually about 2 cm, maximizes its overall strength and function. For this reason, PTT degeneration and/or lengthening will result in remarkable loss of biomechanical function and strength (2).
Early stages of AAFD will demonstrate a reducible and supple deformity. A gastrocnemius-soleus contracture further accentuates and maintains the deformity. The deformity produces persistent stresses on the midtarsal and STJs, which will eventually lead to dorsolateral peritalar subluxation. Dorsolateral peritalar subluxation is a term coined by Hansen that describes AAFD as medial talar head uncovering on an AP radiograph, with forefoot abduction, supination, and dorsiflexion around the talus through the MTJ (3). This will ultimately lead to a fixed flatfoot deformity.
CLASSIFICATION
Classification of PTTD has been divided into four distinct stages originally described by Johnson and Strom and later modified by Myerson (4,5). Stage I PTTD consists of tendonitis and/or tenosynovitis without osseous deformity. The posterior tibial tendon is also of normal function and length. Stage I deformity usually can be treated nonoperatively with mechanical support and control of inflammation. Stage II PTTD is described as posterior tibial tendonitis with a flexible acquired pes planovalgus deformity. The American College of Foot and Ankle Surgeons (ACFAS) Clinical Practice Guidelines (CPG) for AAFD have divided stage II PTTD into stages IIA (early) and IIB (late) for the diagnosis and treatment of adult acquired flatfoot (6). Stage IIA involves a flexible deformity with minimal hindfoot valgus, the absence of forefoot varus, and forefoot abduction with less than 50% talonavicular subluxation. Surgical management of stage IIA deformities usually includes joint-sparing procedures such as calcaneal osteotomies, arthroeresis procedures, tendon transfers, and posterior muscle group lengthening. Stage IIB describes a flexible deformity with moderate to severe hindfoot valgus and talonavicular subluxation, with or without the presence of forefoot varus. Stage IIB deformities can be surgically treated with isolated hindfoot fusions (subtalar, talonavicular, and calcaneocuboid arthrodesis) and/or medial column procedures (naviculocuneiform (NC) arthrodesis, first tarsometatarsal (TMT) arthrodesis, or dorsal opening wedge osteotomy of the cuneiform) to address forefoot varus, in addition to the joint-sparing techniques mentioned for stage IIA. Furthermore, Myerson has further divided stage II PTTD in II A (hindfoot valgus), II B (flexible forefoot supination), II C (fixed forefoot supination), II D (forefoot abduction), and II E (medial ray instability) (7). Stage III PTTD develops with long-standing deformity in which the flexible deformity becomes more rigid. Hindfoot arthritis may be present, and hindfoot joints become stiff and painful. Various combinations of arthrodesing procedures are performed for treatment of stage III PTTD (triple arthrodesis [TA] or double arthrodesis).
Stage IV was added by Myerson in which he describes a rigid valgus deformity of the hindfoot in combination with valgus talar tilt secondary to deltoid insufficiency and spring ligament attenuation (5). This could subsequently lead to arthritis of the ankle and MTJs. Surgical management of stage IV PTTD may include procedures to augment the attenuated medial soft tissues (medial transpositional osteotomies of the calcaneus and deltoid repair/augmentation) in addition to procedures recommended for stage III PTTD.
Stage IV was added by Myerson in which he describes a rigid valgus deformity of the hindfoot in combination with valgus talar tilt secondary to deltoid insufficiency and spring ligament attenuation (5). This could subsequently lead to arthritis of the ankle and MTJs. Surgical management of stage IV PTTD may include procedures to augment the attenuated medial soft tissues (medial transpositional osteotomies of the calcaneus and deltoid repair/augmentation) in addition to procedures recommended for stage III PTTD.
PHYSICAL EXAMINATION
The diagnosis of symptomatic PTTD is based on clinical and radiographic assessment (5,8,9). An adequate history and physical examination is essential in determining the stage of PTTD and appropriate treatment for the patient. The examination begins by performing a complete evaluation of the overall alignment of the lower extremities, with the patient standing barefoot with the knees exposed. Tibial varum or valgum could possibly be accentuating the heel valgus deformity and may need to be addressed (3,8). Gait evaluation should be performed to evaluate for early heel rise, rigid calcaneal valgus, and apropulsion. Early heel rise can be a sign of gastrocnemius contracture (8,10).
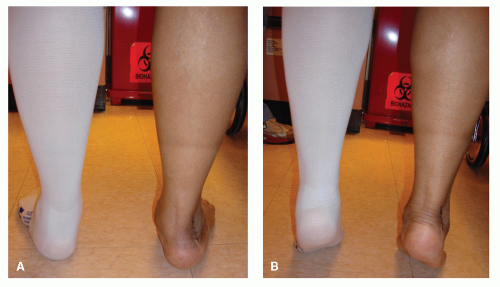
Clinical exam should include the “double heel rise test” and the “too many toes sign.” Johnson first described the “too many toes sign” (4), which is a clinical assessment of the severity of forefoot abduction by the number of toes seen lateral on the affected side when viewing the patient from behind. As the deformity progresses, the number of toes visible will increase. Hindfoot flexibility is evaluated by having the patient perform the “double heel rise test” (8,9). The double heel rise test should be performed to assess the reducibility of the deformity (Fig. 46.1). A valgus heel will reduce to a vertical or varus position indicating a functional STJ in a supple deformity.
Stage I PTTD will appear as an isolated symptomatic tendonitis in the absence of deformity with no loss of function or muscle strength. As the deformity progresses to stage II, mild structural deformity will develop, the symptoms worsen, and the tendon begins to degenerate. The patient presents with functional impairment and diminished muscle strength. Lateral ankle or sinus tarsi pain may also develop secondary to subfibular impingement, and patients may have difficulty performing a single heel rise test during stage IIB (11).
Clinical evaluation of a stage III PTTD will demonstrate significant triplanar deformity, which is clinically and radiographically evident. Stage III PTTD symptoms typically include medial hindfoot pain secondary to soft tissue attenuation. Additionally, lateral hindfoot pain due to calcaneofibular impingement and lateral tarsal arthritis are often present. Motion is usually reduced or absent in the tritarsal complex, and this results in a rigid deformity. The foot will appear with an abducted forefoot; a short, concave lateral column; and a long, convex medial column. The medial longitudinal arch will be collapsed and will not reconstitute with a hallux raise maneuver. The valgus deformity may not reduce with a double heel rise test in stages III and IV of PTTD. A single heel rise test should be performed on the affected foot to ascertain strength of the PTT. Patients typically cannot perform a single heel rise test in later stages of PTTD. A flexor digitorum longus (FDL) tendon transfer should be considered when the deformity is supple and the PTT appears weakened.
NONOPERATIVE MANAGEMENT
Surgical treatment is rarely indicated for stage I PTTD. Supportive therapies including orthotics, bracing, and control of inflammation are often effective in stage I PTTD. Treatment for stages I and IIA PTTD is aimed at improving the patients’ symptoms and attempting to decrease the force being applied to the hindfoot joints. This can be accomplished with weight loss, physical therapy, bracing, support, and activity modifications. Initially, stage I and early stage IIA can be treated with control of inflammation and a period of immobilization, followed by supportive devices. Support to the medial arch is important to improve clinical symptoms such as pain and inflammation and prevent eventual collapse of the medial longitudinal arch (12). Alvarez et al introduced a conservative nonoperative protocol consisting of an exercise program (physical therapy) and either a foot orthosis or a short, articulated ankle-foot orthosis. They concluded that
there was weakness in all muscle groups of the foot and ankle in patients with stage I or II PTTD. Most patients (89%) responded well with a short articulated ankle foot orthosis (SAAFO) or foot orthosis, while function was regained through a four-muscle group ankle-strengthening program (13). At the author’s institution, this treatment protocol has been utilized with similar success. High-demand patients and elite athletes are an exception. They often require more invasive interventions during the earlier stages of PTTD to return to their normal functional level.
there was weakness in all muscle groups of the foot and ankle in patients with stage I or II PTTD. Most patients (89%) responded well with a short articulated ankle foot orthosis (SAAFO) or foot orthosis, while function was regained through a four-muscle group ankle-strengthening program (13). At the author’s institution, this treatment protocol has been utilized with similar success. High-demand patients and elite athletes are an exception. They often require more invasive interventions during the earlier stages of PTTD to return to their normal functional level.
Orthoses have been recommended to address symptoms of painful flatfeet. The goal is to control the amount of hindfoot valgus in the flexible flatfoot deformity and support the medial longitudinal arch. Casting for the orthotic devices should be performed with the STJ in neutral position. Imhauser described the efficacy of orthotic devices in controlling flatfoot deformities. The University of California Biomechanics Laboratory (UCBL) has demonstrated the ability to partially correct both hindfoot and medial column position (12,14). However, the ability of the UCBL device to control foot position is sometimes overridden by the patients’ inability to tolerate a rigid device. Patients who do not tolerate a semirigid device often require placement into a softer orthotic.
The fixed, more severe flatfoot deformities respond better to a custom-molded ankle foot orthosis (AFO), which provides increased ankle support but cannot restore adequate hindfoot position. The authors often use a low articulating AFO (Yankee orthopaedic type) for symptomatic stages I to III flatfoot deformities. Patients who do not respond to initial immobilization and control of inflammation are placed in a low articulating AFO much like the SAAFO described by Marzano (15). The majority of patients do very well with this device. The solid AFO used to immobilize the ankle and a patellar tendon-bearing device are used for bracing the most severe flatfoot deformities to support the ankle and to eliminate motion of the hindfoot and ankle joints (16).
IMAGING STUDIES
RADIOGRAPHIC ANALYSIS
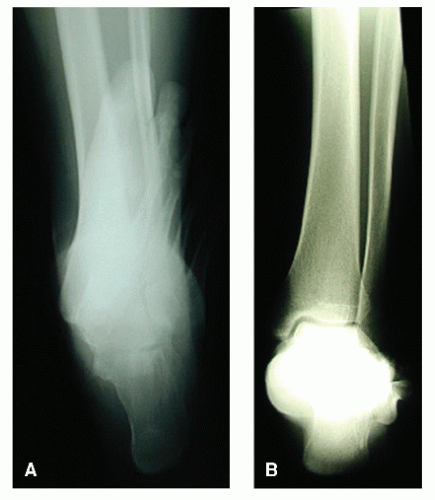
An accurate diagnosis of PTTD secondary to AAFD can often be made entirely upon clinical exam. However, radiographs are useful for assessing concurrent abnormalities, quantifying the degree of deformity, and determining the stage of the disease. Weight-bearing AP, lateral, hindfoot alignment, and long-leg calcaneal axial views are used to evaluate structural deformities and alignment. The weight-bearing hindfoot alignment radiograph is helpful in assessing the amount of valgus deformity of the calcaneus in relation to the tibia (Fig. 46.2) (17). Consideration should be made for obtaining weight-bearing ankle views for late-stage deformities if ankle valgus or arthritis is a concern. Non-weight-bearing (NWB) films fail to provide necessary information for evaluation of alignment and the extent of the deformity. Radiographs appear normal in stage I disease but are obtained to rule out other structural abnormalities, which include tarsal coalition, degenerative arthritis, accessory navicular, and the presence of prior trauma.
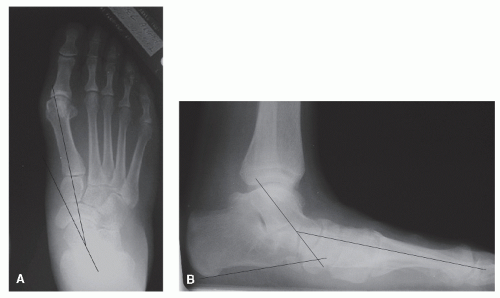
There are many different approaches to the measurement of AAFD on plain radiographs. On the AP radiograph of the foot, Sangeorzan concluded that the talonavicular coverage angle is a good measurement of the extent of midfoot abduction (18). This angle is found by drawing a line from the edges of the articular surfaces of the navicular and of the talus. When the angle between these two lines exceeds 10 degrees, increased midfoot abduction is present. Also on AP radiograph, the talar-first metatarsal angle, which is the angle between the longitudinal axis of the talus and the first metatarsal, can be used to quantify the amount of forefoot abduction (Fig. 46.3A).
The lateral view is used to measure the lateral talar-first metatarsal angle (Meary angle) and the cuneiform height. The lateral talo-first metatarsal angle is measured by finding the angle formed at the intersection of the longitudinal axis of the talus and the first metatarsal (Fig. 46.3B). These two lines are parallel in a rectus foot. With excessive pronation and loss of arch height, this angle will increase with the severity of the deformity (19). In a normal arch, the height of the medial cuneiform is higher than the base of the fifth metatarsal. In a pes planovalgus deformity, the height of the medial cuneiform above the fifth metatarsal decreases and may even become a negative value (20). Cuneiform height is measured by the distance between the inferior portion of the medial cuneiform and the fifth metatarsal base.
ADVANCED IMAGING
Advanced imaging modalities including ultrasound, magnetic resonance imaging (MRI), and computed tomography (CT) can provide additional information in the diagnosis and treatment of PTTD. However, in most cases of PTTD, the diagnosis can be made using clinical and radiographic examination alone, without the use of advanced imaging. Some studies have shown that ultrasound can provide an accurate assessment of the integrity of the PTT (21). However, MRI provides the best evaluation of the spring ligament, the deltoid ligament, and the posterior tibial tendon and muscle belly. MRI also may help to confirm the presence of tenosynovitis or intrasubstance tears of the tendon in a patient who has an unusual or subtle presentation of dysfunction of the PTT (22). The evaluation of the functional status of the PTT can also be made with MRI by assessing the amount of fatty degeneration of the muscle belly
(23). MRI will also provide confirmation of tendinosis. This assessment is important when a tendon transfer is being considered. A CT scan can provide valuable information regarding the diagnosis of a tarsal coalition and determining the level of arthritis. Therefore, advanced imaging is of benefit when plain radiographs are equivocal regarding joint quality, extent of deformity, or a possible tarsal coalition. They are also easily transformed into 3-D computer models by most imaging facilities and may be of some benefit during surgical planning.
(23). MRI will also provide confirmation of tendinosis. This assessment is important when a tendon transfer is being considered. A CT scan can provide valuable information regarding the diagnosis of a tarsal coalition and determining the level of arthritis. Therefore, advanced imaging is of benefit when plain radiographs are equivocal regarding joint quality, extent of deformity, or a possible tarsal coalition. They are also easily transformed into 3-D computer models by most imaging facilities and may be of some benefit during surgical planning.
STAGE I PTTD
Surgical treatment for stage I PTTD is rarely indicated. However, surgical intervention may be warranted in patients with chronic tenosynovitis with or without intratendinous degeneration who have failed nonoperative therapy. High-level athletes and those patients with high-demand occupations may require surgical management of stage I PTTD. Surgery may prevent progression of the deformity. The goal of surgery is to relieve pain and inflammation and to help restore function.
POSTERIOR TIBIAL TENDON DÉBRIDEMENT AND SYNOVECTOMY
Indications
Most cases of stage I PTTD can be treated with immobilization, support, and control of inflammation. Surgery is indicated when nonoperative therapy is ineffective and patients present with persistent symptoms and/or functional deficits. According to McCormack et al (24), tenosynovectomy and tendon débridement for stage I PTTD can halt the progression of the disease process without the need for a tendon transfer.
Contraindications
The main contraindications for isolated tenosynovectomy and tendon débridement of the PTT are the presence of structural deformity and/or intratendinous degeneration. Studies have shown that if there is valgus deformity of the hindfoot, whether flexible or rigid, a tendon débridement alone is inadequate. Also, if intratendinous degeneration is present, débridement alone without transfer and/or adjunctive osseous procedures will be insufficient. Furthermore, disruption of the medial soft tissue structures can result in a rapid progression of the flatfoot deformity.
Technique
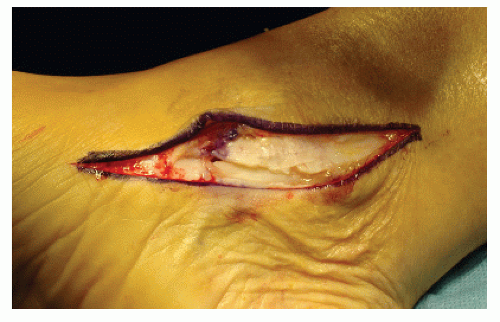
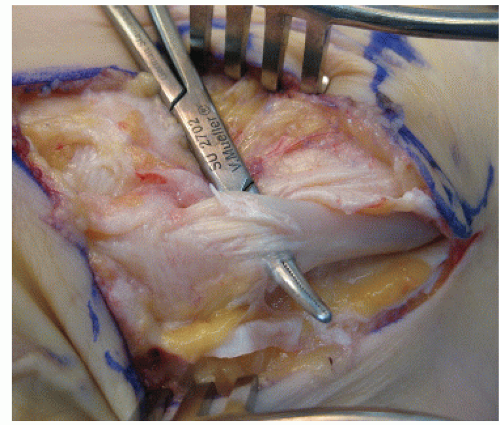
The patient is positioned in the supine position with a thigh tourniquet. A small bump is placed under the contralateral hip to externally rotate the opposite lower extremity obtain good visualization and maximize exposure to the medial ankle. A curvilinear incision is placed along the course of the PTT beginning 3 cm proximal to the tip of the medial malleolus extending distally to the NC joint. Dissection is carried down to the posterior tibial tendon sheath. A pair of curved scissors is used to open the tendon sheath both proximally and distally in one smooth motion, exposing the posterior tibial tendon to its insertion. Effusion of fluid will often expel from the tendon sheath (Fig. 46.4). Débridement of the inflamed synovial lining is then performed. Intratendinous degeneration, often seen as fusiform thickening of the tendon, should be excised, followed by a direct repair of the PTT. A FDL or a flexor hallucis longus (FHL) tendon transfer may be performed if there is significant degeneration of the tendon or substantial weakness was noted during the preoperative
assessment (Fig. 46.5). Inspection along the lateral portion of the tendon might reveal longitudinal split tears in the PTT. The tendon can be repaired via a tubulization suture technique. The sheath is then reapproximated and closed using absorbable suture to prevent dislocation of the PTT.
assessment (Fig. 46.5). Inspection along the lateral portion of the tendon might reveal longitudinal split tears in the PTT. The tendon can be repaired via a tubulization suture technique. The sheath is then reapproximated and closed using absorbable suture to prevent dislocation of the PTT.
Complications
Complications specific for tenosynovectomy and/or tendon débridement include numbness along the medial aspect of the foot, incisional dehiscence, and further progression of the deformity.
Postoperative Management
The patient is initially placed in a NWB cast and immobilized for 3 to 4 weeks. The patient is progressed to a short-leg walking boot and partial weight-bearing. The patient is instructed to remove the boot at home and perform range of motion (ROM) exercises to mobilize the tendon within the tendon sheath to prevent adhesions and fibrosis. The patient is then progressed to full weight-bearing, and physical therapy is initiated for posterior muscle group stretching and flexor muscle strengthening.
STAGE II PTTD
Prior to the 1980s, stage II PTTD was treated with a TA. However, isolated hindfoot arthrodesing procedures and joint-sparing procedures are now more commonly used to treat stage II PTTD. Calcaneal osteotomies, arthroeresis procedures, and medial column procedures have proven to be successful in combination with other ancillary procedures for the treatment of stage II PTTD. The primary goals in surgical management of stage II PTT include improved symptomology, realignment, and restoration of function while maintaining a supple tritarsal complex.
CALCANEAL OSTEOTOMIES
Lateral Column Lengthening (Anterior Calcaneal or Evans Osteotomy)
Indications
Lateral column lengthening (LCL) or the Evans procedure is a powerful anterior calcaneal osteotomy that can provide correction of the foot in multiple planes. The primary indication for performing an isolated LCL (with or without adjunctive soft tissue procedures) is a reducible flat foot with predominately transverse plane deformity and instability of the MTJ. Alternatively, LCL can also be accomplished by bone-block arthrodesis of the calcaneocuboid joint (CCJ). PTT repair, FDL tendon transfer, and posterior muscle group lengthening are also performed with LCL.
Contraindications
This procedure is not recommended for rigid hindfoot deformity and should not be performed if painful arthritic changes are present in any of the tritarsal joints. A metatarsus adductus is a controversial contraindication. It has been suggested that unmasking of a metatarsus adductus can lead to poor results. However, it has been shown radiographically that the degree of metatarsus adductus remains essentially unchanged by LCL (25). Therefore, the authors do not exclude candidates based on this radiographic criterion.
Technique
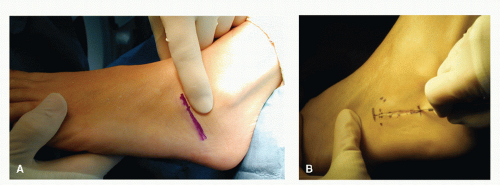
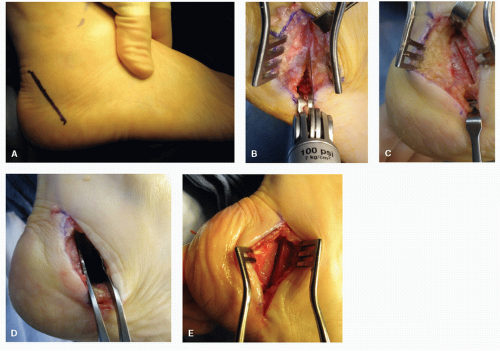
The patient is placed on the operating table in the supine position with a bump under the ipsilateral hip to allow easy access to the lateral hindfoot. Spinal or general anesthesia may be used. An oblique incision is placed just distal to the sinus tarsi and extends 1 to 1.5 cm proximal to the CCJ (Fig. 46.6A). We will sometimes convert this into a serpentine incision to increase exposure to the lateral calcaneal wall if a plate is being used for fixation. This approach usually avoids dorsal cutaneous nerves and will provide access to the lateral wall of the anterior calcaneus. Alternatively, a curve-linear or
transverse approach may be used as well (Fig. 46.6B). Care should be taken in the preservation of the peroneal tendons and the sural nerve with careful retraction (Fig. 46.7). The CCJ should be identified but not exposed for proper osteotomy planning. Overzealous periarticular dissection may impart instability with subsequent sagittal plane displacement of the distal calcaneal segment following execution and distraction of the osteotomy.
transverse approach may be used as well (Fig. 46.6B). Care should be taken in the preservation of the peroneal tendons and the sural nerve with careful retraction (Fig. 46.7). The CCJ should be identified but not exposed for proper osteotomy planning. Overzealous periarticular dissection may impart instability with subsequent sagittal plane displacement of the distal calcaneal segment following execution and distraction of the osteotomy.
The osteotomy is performed approximately 1 to 1.5 cm proximal to the CCJ. The osteotomy is kept more proximal if a plate or staple is being considered for fixation. Otherwise, there is a risk of fixation violating the CCJ. An image intensifier can be used to confirm location prior to executing the periosteal incision and osteotomy (Fig. 46.8). The periosteum is usually incised in a vertical fashion. However, a horizontal incision should be considered when a plate or staple is being used to fixate the osteotomy. An elevator is used to dissect enough periosteum from the lateral calcaneus to allow room for the sagittal saw. The dissection is carried dorsally and plantarly. One should avoid extensive dissection or stretching of the periarticular ligaments of the CCJ as well as the long plantar ligament as this can result in instability of the distal segment. The sagittal saw blade is oriented perpendicular to the lateral surface of the calcaneus and perpendicular to the weight-bearing surface. The osteotomy is performed from lateral to medial. Ideally, the osteotomy should extend between the anterior and middle facets of the STJ (25). Hyer et al (26) found that the majority of calcanei (56%) had a conjoined anterior and middle talocalcaneal articular facet complex, which has implications when planning for the osteotomy. Currently, there are no published recommendations to preoperatively determine conjoined versus separate anterior and middle facets. Use caution when approaching the medial cortex of the calcaneus; exiting the blade too far medially may compromise vital structures. It is sometimes difficult to appreciate the medial cortex, from a tactile standpoint, in this subchondral region of the calcaneus. An osteotome sometimes can be used to complete the osteotomy. A lamina spreader may be used to manipulate and distract the osteotomy (Fig. 46.9A). Alternatively, an external distractor may be used to distract the osteotomy in preparation for the bone graft (Fig. 46.9B and C). The foot should be evaluated with the STJ in neutral position and the forefoot maximally pronated. Distract the osteotomy to the desired position and assess this position both clinically and under image intensification. Simulated weight-bearing fluoroscopy can sometimes
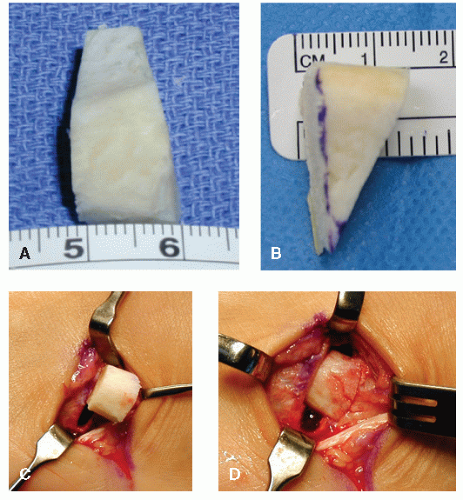
be difficult. Trial wedges are an alternative method to determine the amount of correction and the size of the bone graft that will be required (Fig. 46.9D) (27). The authors typically use freeze-dried or frozen allograft bone as a graft source.
be difficult. Trial wedges are an alternative method to determine the amount of correction and the size of the bone graft that will be required (Fig. 46.9D) (27). The authors typically use freeze-dried or frozen allograft bone as a graft source.
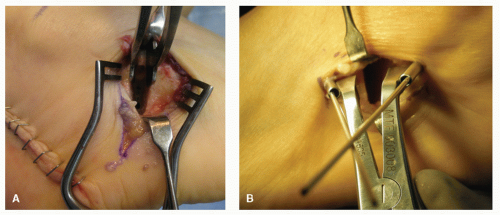 Figure 46.9 A: Lamina spreader used to distract osteotomy. B,C: External distractors used to open the osteotomy. (Continues on next page) |
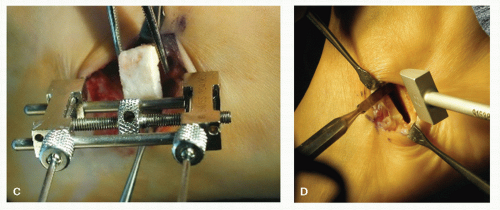 Figure 46.9 (Continued) D: Trial wedge can be used to determine the appropriate size of the bone graft. |
The allograft should be a composite of cortical bone to maintain structural realignment and cancellous bone to promote osteoconduction. Tricortical or bicortical iliac crest graft and patellar graft are good bone graft options. The incorporation rate of allograft bone in calcaneal osteotomies is excellent (28,29,33). The graft should be fashioned into a trapezoid or triangular shape with the base lateral (Fig. 46.10A and B). The graft is then placed into the osteotomy site and tamped into position under tension (Fig. 46.10C and D). Increased tension will eliminate micromotion at the host-graft interface and promote consolidation. Placement of the graft and final verification of the osteotomy should be checked under image intensification. The graft size will vary. A larger graft is used in larger individuals or if significant deformity is present. One must avoid overcorrection. Overcorrection often results in stiffness of the MTJ and plantarflexion of the lateral column. MTJ ROM should be tested by manual eversion testing and the sagittal plane position of the lateral column evaluated after graft placement. Graft size should be adjusted accordingly. The authors often decrease the graft size and add a posterior calcaneal osteotomy in cases in which overcorrection is a potential issue. The authors generally do not use fixation. Lack of fixation has not demonstrated adverse affects on incorporation rate (28). The tension within the osteotomy invariably provides inherent stability. However, a Kirschner wire (K-wire), screw, small plate, or staple may be applied as a form of fixation to stabilize the sagittal plane position of the bone graft and the distal fragment (Fig. 46.11). Other alternatives for LCL include callous distraction osteogenesis as opposed to using allograft or autograft bone (30).
Complications
Potential complications following LCL include nonunion, transient sural neuritis, graft resorption, dorsal displacement of the distal segment, lateral column pain, and CCJ arthrosis. Dorsal displacement of the distal calcaneal segment and lateral column pain are often secondary to overcorrection. Lateral column overload with secondary pain can also result if the forefoot remains supinated following LCL (31). This can be remedied with a plantarflexory procedure of the medial column (32). Nonunion following anterior calcaneal osteotomy is rare, but can occur and result in symptoms. The use of allograft versus autograft bone for reconstruction has been debated. Recent studies have shown excellent results using allograft bone in foot and ankle surgery (28,33,34). Dolan et al studied union rates between allograft and autograft bone when performing an LCL in 33 feet. Their study concluded that union rates between allograft and autograft are equal (35). Thus, allograft may be preferred over autograft to avoid potential donor site morbidity.
Postoperative Management
An NWB short-leg cast is recommended for 8 weeks. Serial radiographs should be performed
to evaluate graft incorporation. Graft stability, as seen by trabeculation at the host-graft interface, is an important factor in determining transition to weight-bearing and requires approximately 6 to 8 weeks in adults. However, absence of warmth and edema are also key indications of bone graft incorporation. The patient can progress to controlled weight-bearing in a fracture brace for 2 to 3 weeks following cast removal and then proceed to physical therapy, which functions to maintain ROM of the foot and ankle as well as to strengthen the posterior muscle group following a lengthening procedure.
to evaluate graft incorporation. Graft stability, as seen by trabeculation at the host-graft interface, is an important factor in determining transition to weight-bearing and requires approximately 6 to 8 weeks in adults. However, absence of warmth and edema are also key indications of bone graft incorporation. The patient can progress to controlled weight-bearing in a fracture brace for 2 to 3 weeks following cast removal and then proceed to physical therapy, which functions to maintain ROM of the foot and ankle as well as to strengthen the posterior muscle group following a lengthening procedure.
Posterior Calcaneal Displacement Osteotomy
Indications
An isolated posterior calcaneal displacement osteotomy (PCDO) (typically with adjunctive soft tissue procedures) is indicated for late stage I and IIA PTTD with reducible hindfoot valgus. There should also be an acceptable degree of stability within the MTJ and minimal to no transverse plane deformity. The authors typically perform an adjunctive FDL tendon transfer and posterior muscle group lengthening. If a forefoot varus is present, it should be reducible. Otherwise, a fixed forefoot varus will require realignment with a medial column procedure.
Contraindications
Absolute contraindications for PCDO include rigid deformities and degenerative joint disease (DJD) within the tritarsal complex. A relative contraindication is a significant clinical deformity with corresponding angular deformity on radiographs. The authors have found that an isolated PCDO will invariably result in undercorrection, even when the deformity is reducible (36). Therefore, the authors will only consider PCDO as an isolated procedure in late stage I and very early stage II PTTD. PCDO is used primarily as a supplement to an Evans procedure in stage IIA or B PTTD or as a supplement to a TA in stage IV PTTD.
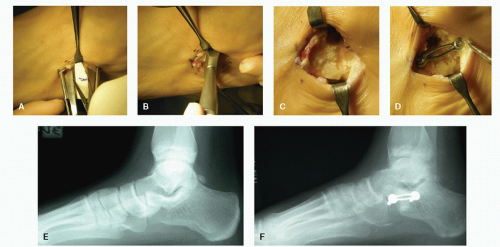
Technique
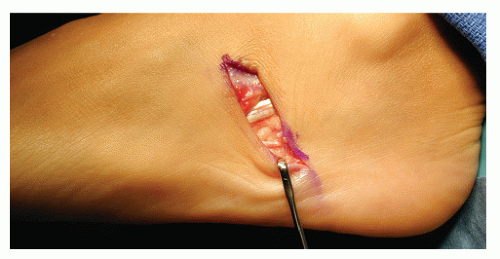
The patient is placed on the operating table in the supine position with a large bump under the ipsilateral hip to allow access to the lateral hindfoot. Spinal or general anesthesia may be used. The incision is placed parallel to the peroneal tendons from just inferior to the lateral malleolus at a 45-degree angle to the weight-bearing surface (Fig. 46.12A). This approach usually avoids the sural nerve, its communicating branches, and the peroneal tendons. The periosteum is incised in the same fashion as the skin incision. An elevator can be used to dissect periosteum from the lateral calcaneus to allow access for the sagittal saw. Dorsal dissection should reach just posterior to the posterior facet of the STJ and inferior dissection just anterior to the plantar tubercle. The osteotomy is then performed in an oblique fashion between these landmarks (Figs. 46.12B). Care should be taken to control the depth of the saw when approaching the medial cortex; this can be accomplished by utilizing two hands. Alternatively, the medial cortex may be broken with an osteotome (Fig. 46.12C). An osteotome or lamina spreader may also be utilized to manipulate the osteotomy to stretch the medial periosteum (Fig. 46.12D). This maneuver will mobilize the tuber segment of the calcaneus and allow medial translation. The posterior tuber is then displaced medially, and provisional fixation is obtained with a 0.062-inch K-wire. The foot is held in plantarflexion during displacement to relax the intrinsic muscles, Achilles tendon,
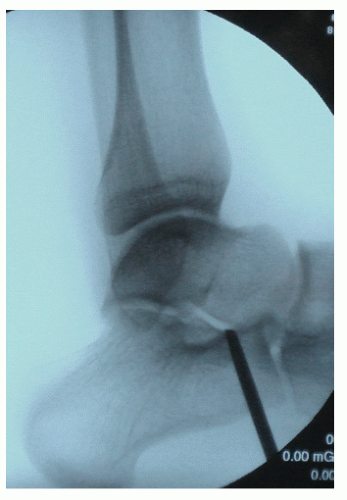
and plantar fascia. This avoids sagittal plane displacement and allows for easy medial manipulation of the posterior segment. The calcaneus is medially translated as far as the soft tissues permit or approximately 1 centimeter (Fig. 46.12E). An axial image can be obtained to insure that adequate medial displacement has been achieved (Fig. 46.13). Osteosynthesis is accomplished with one or two large-diameter compression screws. Care should be taken not to violate the STJ. Compression screws are delivered percutaneously under image intensification (Fig. 46.14). An osteoplasty of the remaining cortical shelf should be performed to avoid tension on the wound (Fig. 46.15). The authors have experienced dehiscence in several patients when osteoplasty has not been performed.
and plantar fascia. This avoids sagittal plane displacement and allows for easy medial manipulation of the posterior segment. The calcaneus is medially translated as far as the soft tissues permit or approximately 1 centimeter (Fig. 46.12E). An axial image can be obtained to insure that adequate medial displacement has been achieved (Fig. 46.13). Osteosynthesis is accomplished with one or two large-diameter compression screws. Care should be taken not to violate the STJ. Compression screws are delivered percutaneously under image intensification (Fig. 46.14). An osteoplasty of the remaining cortical shelf should be performed to avoid tension on the wound (Fig. 46.15). The authors have experienced dehiscence in several patients when osteoplasty has not been performed.
Postoperative Management
The patient is placed in an NWB short-leg cast for 6 weeks. The patient is then advanced to partial weight-bearing in a fracture brace for 2 to 3 weeks. It is important to evaluate the need for physical therapy, as this is often necessary to maintain ROM of the foot and ankle as well as to strengthen the posterior muscle group following lengthening.
Complications
Complications related directly to the PCDO are rare but include peroneal tendon irritation and sural nerve neuritis (37). Nonunion is rare due to the excellent vascularity of the calcaneus. Penetrating the medial cortex too aggressively can damage vital neurovascular structures, so care must be taken when completing the osteotomy through the medial cortex. Structures that cross at the point of the osteotomy include branches of the lateral plantar nerve and posterior tibial artery, as well as the lateral plantar nerve and posterior tibial artery less frequently. Damage to these structures should to be avoided to prevent permanent numbness, increased pain, and hematoma formation (38). A methodically controlled osteotomy will reduce the risk of damage to medial structures. Wound dehiscence is not uncommon following a large displacement or failure to perform an adequate osteoplasty to decompress the lateral skin. Screw heads may cause pain and necessitate removal after healing has occurred (39).
The most common complication is insufficient correction when PCDO is used as the primary procedure to address stage II PTTD. Isolated PCDOs should not be used with significant deformities that are reducible. Inadequate correction will result in a less than optimal outcome. These more significant deformities should be addressed with an LCL osteotomy or double calcaneal osteotomy (DCO) (40).
Double Calcaneal Osteotomy
The combined use of LCL and PCDO has been described for surgical management of stage II PTTD and is commonly referred to as a DCO (Fig. 46.16). Frankel first introduced the concept in 1995 through a single patient with an encouraging outcome
(41). Pomeroy and Manoli et al reported short- and intermediate-term follow-up of patients who underwent double calcaneal osteotomies stating that the “technique provides symptomatic relief and lasting correction of the pes planovalgus deformity associated with stage II posterior tibial tendon insufficiency… It has a high patient satisfaction… and radiographic measurements demonstrate maintenance of correction” (42,43). We have found similar results and continue to utilize the DCO in conjunction with FDL transfers and posterior muscle group lengthening for treatment of reducible stage II flatfoot showing transverse and frontal plane deformity and an unstable MTJ. We believe that the extra-articular location of these osteotomies may prevent impending joint degeneration, provide powerful correction of flatfoot deformity, and preserve the tritarsal complex.
(41). Pomeroy and Manoli et al reported short- and intermediate-term follow-up of patients who underwent double calcaneal osteotomies stating that the “technique provides symptomatic relief and lasting correction of the pes planovalgus deformity associated with stage II posterior tibial tendon insufficiency… It has a high patient satisfaction… and radiographic measurements demonstrate maintenance of correction” (42,43). We have found similar results and continue to utilize the DCO in conjunction with FDL transfers and posterior muscle group lengthening for treatment of reducible stage II flatfoot showing transverse and frontal plane deformity and an unstable MTJ. We believe that the extra-articular location of these osteotomies may prevent impending joint degeneration, provide powerful correction of flatfoot deformity, and preserve the tritarsal complex.
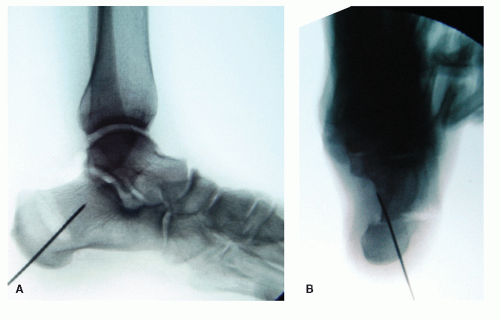 Figure 46.13 Lateral and axial intraoperative images demonstrating medial displacement and provisional fixation.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|