Posterior Spinal Fixation for Thoracolumbar Spinal Trauma
Kris Radcliff
C. Chambliss Harrod
Sapan D. Gandhi
Christopher K. Kepler
Alexander R. Vaccaro
INDICATIONS/CONTRAINDICATIONS
The goals of thoracolumbar fracture care are prevention of neurologic injury, restoration of sagittal alignment, and facilitation of early mobilization. Anatomically, several factors predispose the thoracolumbar junction to trauma and spinal cord injury. Forces across the thoracolumbar region are amplified by the rigid, long lever arm of the thoracic spine. There is also a transition of neurologic elements from spinal cord to the conus medullaris and a relatively small spinal cord to canal ratio as one moves distally. The mean normal thoracolumbar sagittal alignment is 0 to 3 degrees of lordosis (9). Mean normal lumbar lordosis is approximately 60 degrees (9) although the majority of lordosis is at L4-L5 and L5-S1. Mean thoracic kyphosis is 40 degrees (9).
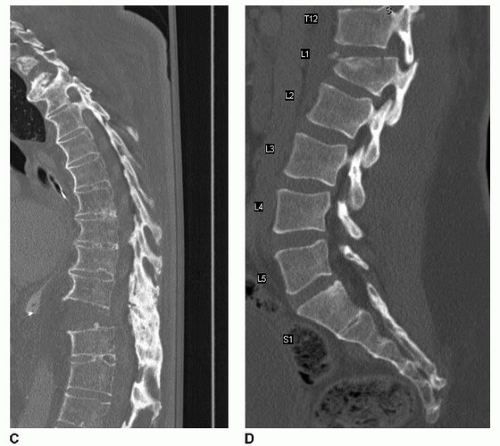
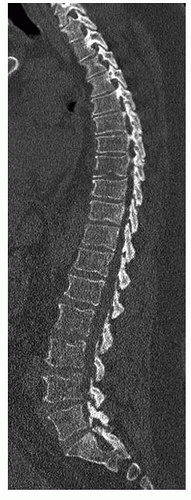
Treatment decision making of thoracolumbar fractures includes assessment of fracture morphology, posterior ligamentous complex integrity, and neurologic status. The thoracolumbar injury classification system (TLICS) (17,21) is a classification algorithm to support decision making in thoracolumbar fractures (Fig. 18-1). Burst fractures are characterized by bony failure of the vertebral body (Fig. 18-2A). Isolated, neurologically intact thoracolumbar burst fractures without posterior ligamentous injury may be managed nonsurgically in the majority of circumstances. Distraction injuries, including flexion-distraction injuries (Fig. 18-2B) and extension distraction injuries (Fig. 18-2C), are often unstable and in the vast majority of cases benefit from surgical stabilization due to distraction failure of the vertebral elements and ligamentous injury. Translationrotation injuries (Fig. 18-2D) are also unstable and are typically managed surgically. Relative indications for surgical stabilization include associated injuries (spinal, abdominal, or extremity) that would complicate compliance with bracing, inability to brace due to body habitus, or high risk of failure of nonsurgical treatment.
A posterior surgical approach is the most commonly used approach for thoracolumbar fractures as it is extensile, allows biomechanically rigid instrumentation, is more familiar to spinal surgeons, does not require the assistance of an approach surgeon, and allows fixation of multiple spinal segments.
The anterior approach is selected for direct decompression from anterior retropulsion of bony fragments at the conus and spinal cord injury level. An anterior approach may allow shorter fusion constructs and sparing of fusion levels.
Relative contraindications to posterior spinal fixation of thoracolumbar fractures include open wounds or compromised posterior soft tissues including skin or subcutaneous tissues, medical instability or Morel-Lavelle lesions. Other relative contraindications include significant retropulsion at the spinal cord level, which may be better addressed with an anterior approach.
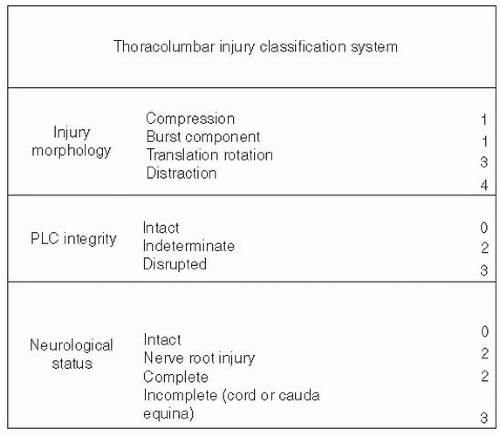 FIGURE 18-1 Thoracolumbar injury classification system. The TLICS includes three elements: fracture morphology, posterior ligamentous complex injury, and neurologic injury. Fractures with a TLIC score greater than 5 are considered to be candidates for surgical intervention. (Adapted from Vaccaro AR, et al.: A new classification of thoracolumbar injuries: the importance of injury morphology, the integrity of the posterior ligamentous complex, and neurologic status. Spine 30(20): 2325, 2005.) |
PREOPERATIVE PREPARATION
Careful clinical assessment with a detailed physical and neurologic examination is essential. Mechanism of injury, associated spinal and nonspinal injuries, and precise physical examination are important in understanding the injury “character” and extent. Furthermore, patients should be queried about coagulopathy (either pharmacologic or pathologic) and history of previous spinal surgery or spondyloarthropathy.
Imaging Assessment
High-resolution computed tomography (CT) is a common trauma screening study in many centers. Sagittal and axial reconstructions are essential to appreciate translation and sagittal fracture lines. MRI is performed for evaluation of posterior ligamentous complex injury (10,16) (Fig. 18-3) and neurologic compression. Imaging studies, particularly in the thoracic spine, should include a scout or scanning view to enable the surgeon to directly count vertebrae from the sacrum to ensure correctlevel surgery is performed (Fig. 18-4).
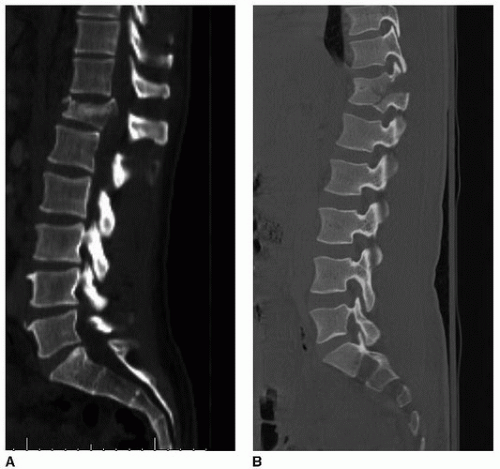 FIGURE 18-2 A: Midsagittal CT thoracolumbar burst fracture is characterized by involvement of the anterior vertebral body. B: Flexion-distraction injury. |
Prior to commencement of the procedure, the surgeon should inspect the preoperative CT scan for the fracture morphology, translation, and evaluation of the adequacy of the pedicles for instrumentation including length, axial convergence, axial vertebral body rotation, scoliosis, and pedicle diameter. Also inspect for location of the great vessels, rib fractures, and facet or pedicle fractures, which may obscure starting points.
Associated spinal and nonspinal injuries should be identified. Approximately 10% to 20% of patients have noncontiguous spinal fractures. Attention should be directed to the cervical spine and the necessity for immobilization or removal of a cervical collar prior to posterior spinal fixation for thoracolumbar trauma. Additionally, the surgeon should discuss with the trauma physicians about the possibility of hollow viscus organ injury particularly after flexion-distraction injuries.
Selection of Fusion Levels
Traditional posterior instrumentation for thoracolumbar fractures differs according to the patients’ pathology. Burst fractures are unstable in axial loading, and traditionally, “long-segment” instrumentation (pedicular) is often considered two and sometimes three levels above and below the fractured level to resist compressive loads (14). Other fracture morphologies, including translation-rotation injuries, extension distraction injuries, and flexion-distraction injuries (2) (including “Chance” fractures), may be more stable to axial loading. Short-segment instrumentation, including one to two levels above and below the level of injury, may be more appropriate for selected fractures. The load-sharing score is a decision-making tool to enable surgeons to identify which fractures are most amenable to short-segment instrumentation (15). The load-sharing score assigns 0 to 3 points to fracture comminution, local kyphosis between 15 and 30 degrees, and axial fragment diastasis, and the total score is calculated 0 to 9 (13). Fractures that score 7 or more are considered to be poor candidates for short-segment fixation.
PERIOPERATIVE CONSIDERATIONS
Patients undergoing posterior spinal fixation for thoracolumbar fractures should undergo preoperative medical evaluation and risk stratification and optimization prior to surgery. Progressive neurologic deficit is considered a surgical emergency. Incomplete neurologic deficit is an urgent but not emergent condition best addressed with early surgery when medically cleared. There is no definitive high-level evidence supporting early surgery for thoracolumbar trauma at this time in the literature (20). Several studies have shown a benefit to early surgery in terms of reduction of medical complications (1,11). Consideration should also be given to the possibility of spinal shock and the possibility that an incomplete spinal cord injury may present as a complete injury due to spinal shock (4).
As part of perioperative management, the surgeon should inform the anesthetic team about special requirements including special positioning or intubation requirements, cervical spine clearance or stabilization, presence of other spinal injuries, blood pressure support, steroid dosing, need for onelung ventilation if necessary, and expected blood loss. The authors’ preference in the setting of a neurologic deficit is to maintain mean arterial pressure greater than 85 mm Hg during the procedure using continuous arterial blood pressure monitoring. The authors’ preference is also for early involvement of plastic surgery if there is concern about adequate soft tissue for closure. Spinal cord injury is a major risk factor for deep venous thrombosis, increasing the risk eightfold over other isolated thoracolumbar trauma (8). Consideration should be given to deep venous thrombosis chemoprophylaxis to reduce the risk of pulmonary embolism. In cases where a prolonged period before thromboprophylaxis is considered and chemoprophylaxis is contraindicated, consideration should be given to placement of an inferior vena cava filter.
Given the biomechanical demands of spinal cord injury, the instability due to loss of protective muscle function, and the high prevalence of smoking in the trauma population, the authors’ preference is autogenous iliac crest for arthrodesis of most patients with thoracolumbar trauma. Preoperative intravenous antibiotic prophylaxis is recommended on all surgeries. Antibiotics should be redosed if the surgical procedure lasts more than 4 hours or if estimated blood loss is greater than 1,000 mL. We monitor somatosensory evoked potentials and motor evoked potential for all spinal cord surgeries. We also perform dynamic triggered electromyography (EMG) for pedicle screw stimulation.
Technique
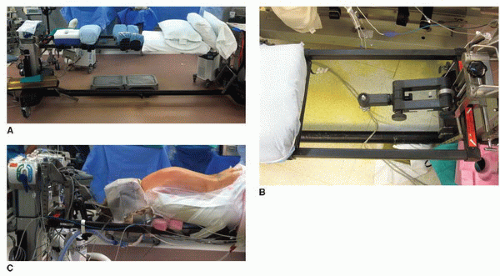
Positioning
Positioning should be dependent upon the fracture morphology. The authors perform the posterior approach prone on a radiolucent Jackson table (Fig. 18-5). The position of the chest pad (normally at the sternal notch) may be manipulated distally to effect kyphosis in the case of an extension distraction injury or fracture dislocation. Similarly, the iliac crest pads, which normally are located at the level of the anterior superior iliac crest, may be manipulated more proximally to effect kyphosis and more distally to increase lordosis. If the iliac crest pads are too low, the patient can develop meralgia paresthetica or a femoral nerve palsy postoperatively if they are directly in the inguinal region. The abdomen should be free to reduce venous pressure and epidural venous bleeding.
Arms are abducted forward out of the operative field and are supported on arm boards and are positioned in a manner so as to not obscure x-ray visualization. Care should be taken to pad the brachial plexus and the ulnar nerves. The head may be supported on a pillow or, for long cases or cases involving the cervicothoracic junction, held in a Mayfield head holder supported from the top of the Jackson table. Care should be taken to ensure that the patient’s eyes are free and arterial pressure is carefully monitored to reduce the risk of blindness. The perineal region should be inspected to ensure that (in the case of male patients) the testicles hang free. The Foley catheter should be taped to the bed so it does not get caught on the C-arm if it hangs unsupported. The patients’ knees rest on a gel pad on the Jackson table and are gently flexed. The patient’s shins rest on one or two pillows. Sequential compression devices are applied to the patient’s shins prior to prone positioning. Localization of levels with intraoperative fluoroscopy may be performed prior to prepping. The authors in some cases confirm adequate radiographic visualization with intraoperative fluoroscopy prior to prepping and draping to confirm that there are no monitors or wires, which are preventing adequate visualization. All surgeries are performed with an intraoperative blood salvage system to reduce the need for nonautologous blood transfusions.
Exposure
For thoracic cases, the spine is draped from lower cervical spine to the pelvis. For lumbar fractures, the spine is draped from the apex of thoracic kyphosis to the sacrum. If iliac crest graft is going to be harvested, then the iliac crest is draped into the field as well.
A midline posterior exposure is a standard extensile approach. The authors’ preference is exposure of the fascia bilaterally prior to deeper exposure to facilitate closure at the conclusion of the case. The author will dissect and identify the fascia and undermine the plane between the subcutaneous fat and the fascia bilaterally several millimeters. The incision is midline. After exposure of the fascial plane (prior to violating the fascia), we repalpate the spinous processes and ensure that the midline is again identified. A cerebellar self-retaining retractor may be helpful at this stage. Exposure may proceed subperiosteally elevating the multifidus muscles off of the underlying spinous processes and laminae. Exposure then proceeds lateral to the facet joints and the transverse processes (TPs). In the lumbar spine, Gelpi retractors are placed deep to the paraspinous muscles to hold the muscles back while remaining in an unobtrusive location to avoid interfering with lumbar instrumentation.
A midline, subperiosteal exposure of the spinous processes and laminae allows for the most efficient, bloodless exposure. The surgeon should avoid working into a hole or crevice as bleeding can quickly occur. Areas that are not being exposed should be packed with sterile sponges to tamponade venous bleeding. Care must be taken in areas of injury not to violate the spinal canal through defects in the laminae or tears in the ligamentum flavum that may have occurred as a result of the spinal fracture (Fig. 18-6




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree