Posterior Occipitocervical Fusion
Mathias Daniels
Zachary Child
Jens R. Chapman
Carlo Bellabarba
INDICATIONS
Occipitocervical fusion with or without neural element decompression is usually used to definitively treat craniocervical instability or deformity-related conditions. Typical indications for this procedure include patients afflicted by trauma, inflammatory disease processes, deformity, neoplasia, and more rarely infections, degenerative diseases, and congenital dysplasia (21).
Untreated instability or displacement of the craniocervical junction can result in a variety of sequelae ranging from progressive pain and neurologic dysfunction to death. Instability of the craniocervical joints in the setting of trauma is usually manifested by any translation or distraction of more than 1 mm in any plane, presence of neurologic injury, or concomitant cerebrovascular trauma (4). With respect to trauma, any injury to the atlantoaxial articulation should be evaluated for its effect on the stability of the craniocervical junction. It is important to remember that in instances of traumatic craniocervical instability, the static position of the head relative to the cervical spine is usually arbitrary and is more dependent on external forces than on any intrinsic injury characteristic. In patients with nontraumatic cranial settling or deformity, such as atlantoaxial dislocation or kyphosis, brainstem or spinal cord compression may lead to respiratory compromise, cranial nerve deficits, paresis, paralysis, and even sudden death.
GENERAL TECHNIQUE
The goal of this type of surgery is to provide permanent immobilization of the craniocervical junction and—as needed—adjacent spine segments, in a functionally useful, preferably balanced anatomic alignment. This desired result is preferably gained through a firm osseous fusion accomplished through structural bone graft in combination with morselized graft. Implants take the secondary role of securing the best possible craniocervical alignment while optimizing chances for successful osseous fusion. In this era of advanced implant fixation systems, the goal of achieving a solid fusion remains paramount to any device design, and thus, suitable attention should be placed on allowing for this important biologic healing process to take place (26). Our preferred internal fixation consists of segmental instrumentation via a rod/screw/plate construct and often involves the use of cables or wires in a supplemental fashion to secure structural bone graft that bridges the occipitocervical junction. Temporary postoperative immobilization can be supplied through a variety of modalities befitting the patient needs and range from a soft neck collar to rigid neck collars or halo-vest constructs. For very young skeletally immature patients requiring craniocervical fusion, structural bone graft alone with cables and supplemental halo-vest fixation may be sufficient.
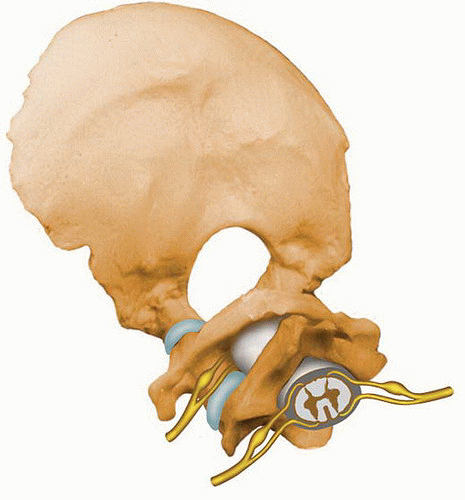
The posterior midline approach is by far the most commonly used surgical approach to treat most craniocervical disorders. A straightforward midline exposure usually provides predictable exposure of familiar posterior anatomic landmarks and can easily be extended to an extensile approach of the lower cervical spine or the upper thoracic spine, if needed (Fig. 12-1). This
exposure allows for posterior decompression of neural structures as well as placement of bone grafting and rigid posterior segmental fixation while it also minimizes long-term exposure-related morbidity. Indirect decompression of anterior compressive lesions caused by nonrigid upper cervical spine kyphosis can usually be gained through traction and subsequent posterior-only decompression and instrumented fusion surgery. Some anterior compressive lesions, such as retrodental pannus formation associated with atlantoaxial instability in inflammatory diseases, may also be expected to resorb with a solid posteriorly based fusion. Anterior surgery may be performed through transoral and anterolateral or direct upper neck exposures. Indications for these include fixed upper cervical deformities in need of deformity correction, neoplasia, and rarely patients with space-occupying lesions brought on by inflammatory conditions (22). Finally, socalled minimally invasive posterior stabilizing procedures relying largely on interarticular screw fixations have been described but have failed to attain greater popularity. All of these variants of craniocervical spine surgery are very limited in their indication range compared to the posterior midline approach and are highly case specific. Undoubtedly, the posterior open technique allows for superior biomechanical stabilization and controlled realignment while affording a high incidence of fusion.
exposure allows for posterior decompression of neural structures as well as placement of bone grafting and rigid posterior segmental fixation while it also minimizes long-term exposure-related morbidity. Indirect decompression of anterior compressive lesions caused by nonrigid upper cervical spine kyphosis can usually be gained through traction and subsequent posterior-only decompression and instrumented fusion surgery. Some anterior compressive lesions, such as retrodental pannus formation associated with atlantoaxial instability in inflammatory diseases, may also be expected to resorb with a solid posteriorly based fusion. Anterior surgery may be performed through transoral and anterolateral or direct upper neck exposures. Indications for these include fixed upper cervical deformities in need of deformity correction, neoplasia, and rarely patients with space-occupying lesions brought on by inflammatory conditions (22). Finally, socalled minimally invasive posterior stabilizing procedures relying largely on interarticular screw fixations have been described but have failed to attain greater popularity. All of these variants of craniocervical spine surgery are very limited in their indication range compared to the posterior midline approach and are highly case specific. Undoubtedly, the posterior open technique allows for superior biomechanical stabilization and controlled realignment while affording a high incidence of fusion.
PREOPERATIVE PREPARATION
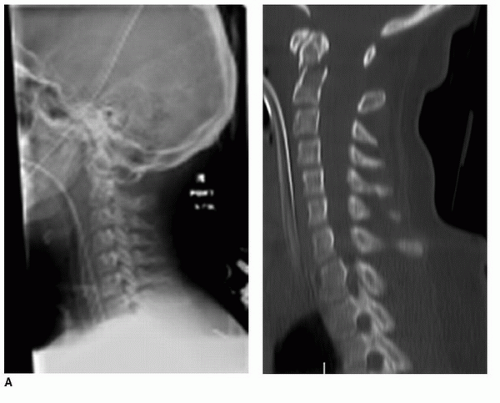
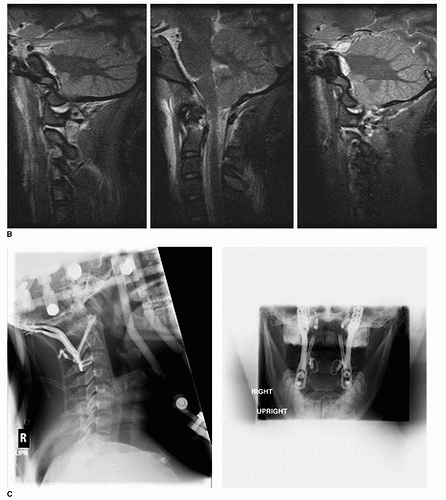
As in any surgical undertaking, careful understanding of the patient anatomy and pathophysiology is an important prerequisite for a successful procedure. The craniocervical junction encompasses a confluence of multiple vital structures, which require appropriate imaging modalities for preoperative surgical planning. In addition to anteroposterior and lateral plain radiographs, it is helpful to have advanced imaging in the form of computed tomography (CT) scan and/or magnetic resonance imaging (MRI) available for comprehensive preoperative assessment as medically indicated (25). Perfusion studies, such as MR angiography (MRA) or CT angiography, may be indicated for patients with suspected vertebral artery trauma or in case of suspected vascular abnormalities (Figs. 12-2 and 12-3).
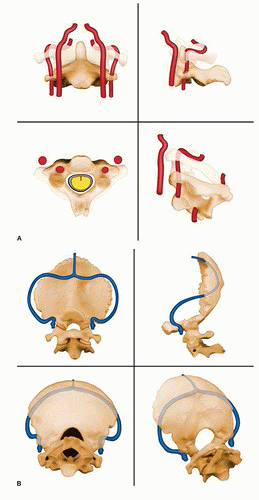
Anteroposterior and lateral radiographs are useful in assessing global sagittal and coronal alignment, as well as a number of craniocervical reference lines to measure cranial settling and instability (Harris lines, Power ratio, Wackenheim line). Ideally, a true lateral radiograph centered on the craniocervical junction is available as a valuable reference tool (20). Some understanding of preferred craniocervical alignment of the patient about to undergo permanent fusion of this articulation is helpful in order to minimize the risk of functional impairment or secondary compensatory spinal deformity. Calculation of an occipitocervical slope angle and/or occipitocervical incidence may help guide alignment determination in the future (16) (Fig. 12-4).
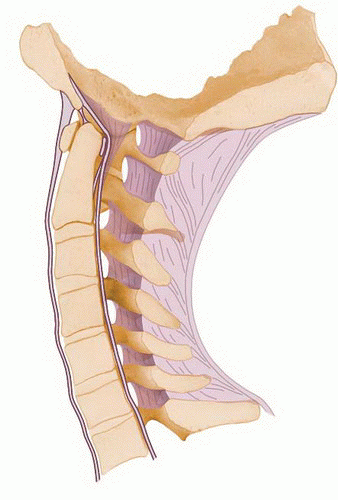 FIGURE 12-3 Measuring craniocervical alignment. The subject of craniocervical alignment angles has been overlooked for a long time despite its significant impact on overall sagittal balance of the patient and potential implications on development of adjacent segment disease. Occipitocervical slope is determined by drawing a line from the midpoint of the orbital globe to the opisthion and then calculating the resultant angle to the horizon level. Occipital inclination is determined as the angle from a perpendicular line drawn from the maximum anteroposterior skull excursion to a vertical line through the odontoid process. While larger population-based studies and relationship to outcomes are still elusive, a general range of an occipital slope of 20 to 30 degrees and an occipital inclination of 30 degrees (±5 degrees) has been suggested (19). |
CT imaging with reformatted views in sagittal and coronal planes allows for detailed assessment of bony architecture in preparation for hardware placement. This is of particular importance toward better understanding of vertebral artery anatomy, which can be quite variable. Other anatomic norm variants, such as failures of segmentation or formation in the craniocervical junction, should be assessed on CT. Finally, important insights that can be gained from preoperative CT analysis, for instance, include occipital skull thickness, the presence of associated skull and cervical segment fractures, as well as bone quality and spinal morphology in general (14).
MRI is helpful in identifying medullary signal changes in brainstem and cord, demonstrating space-occupying lesions in the neural canal and assessing for integrity of craniocervical ligaments and fluid signals in the major articulations of this critical and vulnerable transition region.
Mechanical stability of the craniocervical junction is a result of a combination of osseous, ligamentous, and muscular restraints that permit a significant degree of motion in multiple planes (7,21). For patients with questionable stability, fluoroscopically guided traction tests have been helpful adjuvants in decision making. This form of dynamic imaging has proven to be safe in our hands and can convincingly confirm either instability or ligamentous integrity (4).
For a variety of conditions, it can be very important to establish integrity of cerebral blood flow. This is probably best established with CT angiography; however, MRA can be a suitable alternative (10). In cases of flow impairment, it may be helpful to obtain cerebral Doppler monitoring to look for ongoing perfusion problems.
EXAMINATION PEARLS
Preoperative clinical examinations of patients with suspected craniocervical abnormalities if possible preferably include assessment of long-tract signs, pathologic reflexes, and cranial nerve function 2 to 12 bilaterally in addition to the usual systematic motor, sensory, and reflex assessment. Exorbitant pain in the skull base region may indicate trauma and/or instability. Greater occipital neuralgia may be pathognomonic for chronic atlantoaxial derangement and C2 root impingement.
Craniocervical dissociation or severe rotatory subluxation (types III or IV) should heighten the suspicion for presence of a vertebral artery injury. Fractures of the transverse foramen, especially displaced fractures, may be other tip-offs for potential vertebral artery injuries (10).
Anterior fractures of the occipital condyles deserve scrutiny, and the potential for craniocervical dissociation should be considered (2). If in doubt, a manual fluoroscopic traction test can be performed to document stability. Presence of bilateral occipital condyle fractures invariably implies an unstable occipitocervical dissociation.
Radiographic signs of transverse alar ligament (TAL) instability include widening of the lateral masses and bony avulsion injuries of the atlas. The TAL is considered to be the primary stabilizer of the atlantoaxial articulation.
A preoperative/intraoperative fluoroscopic manual traction test can confirm ligamentous disruption and document cervicocranial instability.
Preoperative CT angiography and/or MRA is recommended preoperatively for suspected vertebral artery injuries.
TECHNIQUE
Preoperative Preparation: Instability or derangement of the craniocervical junction places its neurovascular structures at risk with potential for catastrophic outcome due to a lack of substantial primary bony craniocervical stabilizers. For severe craniocervical trauma, initial stabilization is preferably accomplished with sandsacks surrounding the head with tape placed transversely across the patient’s forehead. Alternatively, a primary halo-vest assembly can be considered as a temporary immobilizer. Traction is not desirable in this setting. Neither of the mentioned external immobilization options is particularly functional beyond a relatively brief temporizing period, thus placing an imperative on early definitive surgical intervention (5). For elective conditions such as craniocervical settling seen with inflammatory conditions, thought may be given to preoperative skeletal traction, usually applied through a halo ring over a course of several days, with the goal to facilitate a gradual deformity reduction over several days. Such a deformity reduction through skeletal traction is preferably accompanied by serial lateral C-spine radiographs and clinical evaluations.
Prior to actual surgery, it is important to establish a safe airway, avoiding excessive manipulation of the patient’s neck prior embarking on surgery in cases of instability or major deformity. For those patients, a safe endotracheal airway can be established through awake fiberoptic or nasal
intubation techniques while maintaining full spine precautions with the patient positioned prone on a radiolucent table. Baseline electrophysiologic monitoring with somatosensory evoked potentials and motor evoked potentials is completed prior to prone positioning and repeated after final positioning. Final craniocervical fine adjustment is performed under fluoroscopy shortly after turning the patient prone to assure the best possible closed reduction prior to embarking on surgery. For trauma cases, the surgeons might consider the threat of craniocervical distraction by excessive reverse Trendelenburg positioning.
intubation techniques while maintaining full spine precautions with the patient positioned prone on a radiolucent table. Baseline electrophysiologic monitoring with somatosensory evoked potentials and motor evoked potentials is completed prior to prone positioning and repeated after final positioning. Final craniocervical fine adjustment is performed under fluoroscopy shortly after turning the patient prone to assure the best possible closed reduction prior to embarking on surgery. For trauma cases, the surgeons might consider the threat of craniocervical distraction by excessive reverse Trendelenburg positioning.
Surgical Technique:




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree