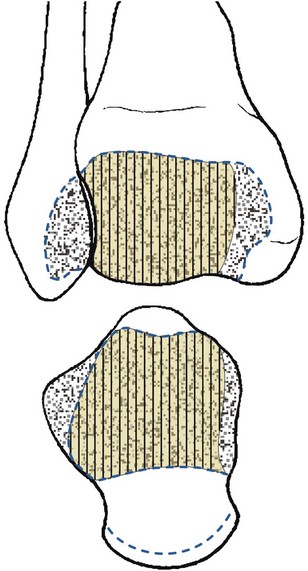
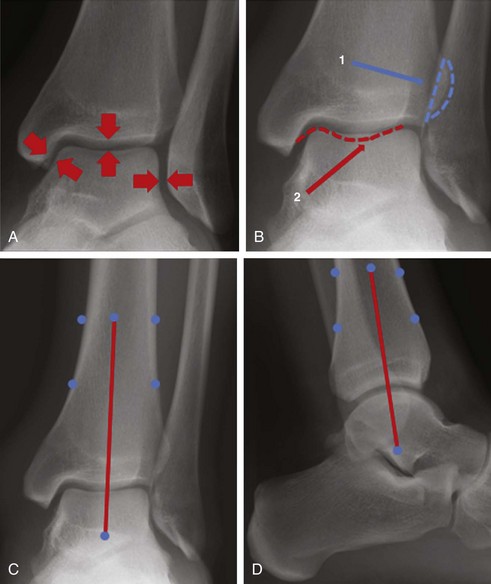
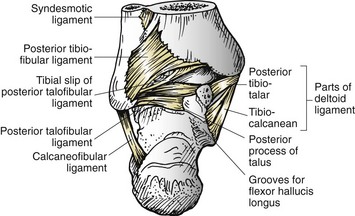
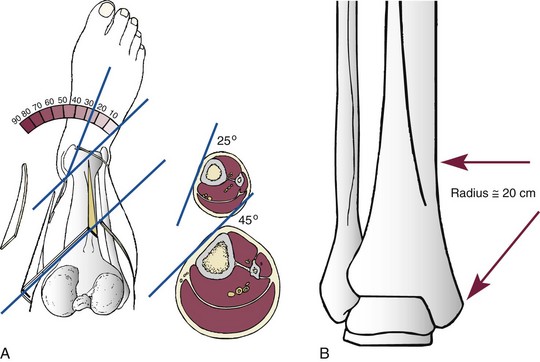
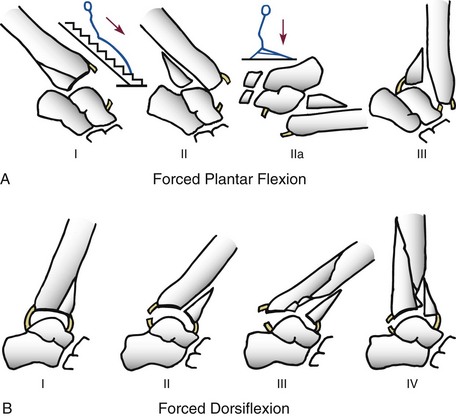
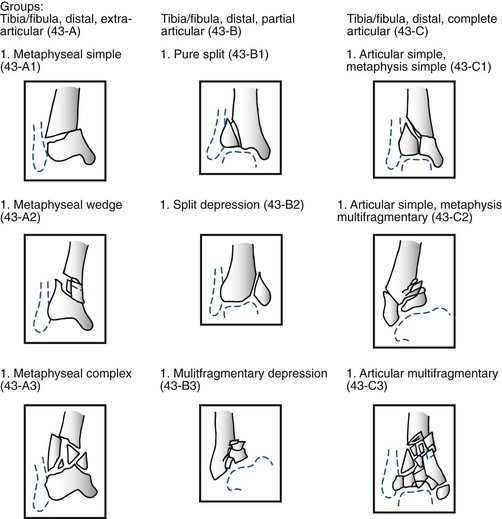
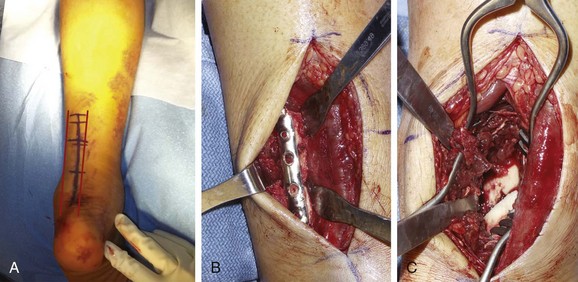
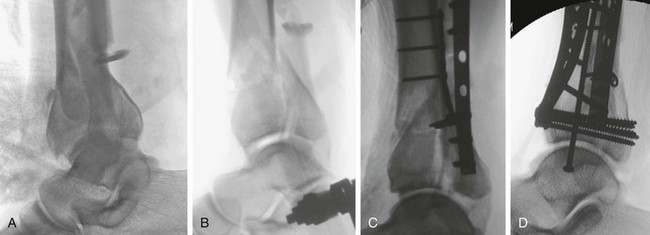
Chapter 36 First described by Destot35 in 1911, ankle fractures that involve the weight-bearing articular surface, or floor, of the distal tibia are known as pilon fractures. Bonin,11 in 1950, described the same fracture as a “plafond” fracture because the fracture disrupted the roof of the ankle joint. In 1968, Rüedi et al86 published their landmark article and were the first to describe the fracture, its treatment, and a prognostic classification. Since that time, the severity of this injury, the complexity of treatment methods, and the limitations of management have been well documented and still pose a challenge to the orthopaedic surgeon. These injuries are rare and comprise less than 1% of all lower extremity fractures but involve between 5% and 10% of tibia fractures.9,18,83 The articular surface of the distal tibia is an irregularly shaped rectangle and articulates with the dome of the talus (Fig. 36-1). The surface is wider anteriorly than posteriorly, and it is concave in both the coronal and sagittal planes.91 This articular surface is continuous with the medial malleolar articular surface, which lies at an angle of about 90 degrees to the tibial plafond and extends about 1.5 cm distal to it. The medial aspect of the distal fibula also articulates with the lateral aspect of the talus to complete the ankle mortise (Fig. 36-2). At the metaphysis, the cortex is thin and filled with relatively dense cancellous bone, with the strongest bone near the subchondral plate. The lateral surface of the distal tibia forms a triangular fibular notch where the tibia and fibula articulate.12 The anterior tibiofibular ligaments arise from the Chaput tubercle on the anterolateral tibia, anterior to the fibular notch; these ligaments insert on the Wagstaffe tubercle of the distal fibula.73 The posterior portion of this articulation serves as the attachment for the posterior tibiofibular ligament, whose ligaments are oriented inferior and laterally (Fig. 36-3). The remainder of the syndesmotic complex consists of the strong interosseous ligament, a distal continuation of the interosseous membrane, and the inferior transverse ligament, running deep to the posterior tibiofibular ligament between the tibia and fibula.12 Internal tibial torsion of approximately 25 degrees is seen from the middiaphyseal medial surface of the tibia to the flat surface of the medial malleolus (Fig. 36-4).58 The anteromedial surface of the distal metaphysis is concave; the radius of curvature of this supramalleolar curve is approximately 20 cm.58 This curved area extends 8 to 12 cm proximal to the medial malleolus, depending on the length of the tibia. The skin covering the distal tibia receives its direct blood supply from the underlying fascia via perforating arteries originating from the dorsalis pedis, posterior tibial, and peroneal arteries.100 The superficial venous system of the leg includes the greater saphenous vein, which travels with the saphenous nerve anterior to the medial malleolus up the medial surface of the tibia to the knee. The lesser saphenous vein, the lesser saphenous nerve, and the sural nerve all run posterior to the lateral malleolus, traveling proximally to the center of the posterior aspect of the leg between the medial and lateral heads of the gastrocnemius.91 The primary branches of the anterior and posterior tibial artery provide the main extraosseous blood supply to the tibia.12 It is well known that the extraosseous blood supply nourishes the outer third of the cortex, and the inner two thirds receives its blood supply from the nutrient artery and its medullary branches.49 Many authors have speculated on the mechanism of a pilon injury.6,35,40,86 Böhler6 was first to note that the position of the foot at the time of impact was critical to the morphology of the fracture. Rüedi,86 however, expanded on this, as did Trojan and Jahna.104 Rüedi86 was the first to describe in detail the combination of an axially applied load in combination with foot position. If the vertical compression force is applied to a plantigrade foot, a central depression occurs, whereas if the force is applied with the foot in either dorsiflexion or plantar flexion, the fracture results in anterior or posterior malleolar injuries, respectively (Fig. 36-5). Aside from the axial load, additional forces can be created to give each fracture its own personality, including bending, rotational, and shearing forces. These fractures also vary by the amount of energy that they absorb, ranging from high-energy injuries (motor vehicle accidents) to lower-energy injuries (simple fall). The higher the energy of the injury is, the greater the likelihood of comminution, displacement, and cartilage injury. The purpose of a classification is to aid the surgeon in selecting a treatment method and to provide prognostic and outcomes based on the fracture pattern. These two principles are essential in the development and use of creating a reliable classification system. Early on attempts at a classification system for pilon fractures were made. Rüedi et al,84 Kellam and Waddell,42 Mast et al,59 and the Association for Osteosynthesis/Association for the Study of Internal Fixation (AO/ASIF)66 have all used plain radiographs to classify pilon fractures. The early radiographic classifications of Böhler,6 and Bonin11 were based on mechanism of injury, and the position of the foot and the direction of the force applied were important criteria. As Rüedi et al86 pointed out in their seminal work, these early classifications did not assist the surgeon in either recognizing the severity of the injury, planning the surgical approach, or determining the outcome. Instead, Rüedi et al86 popularized an easily reproducible classification based on the amount of joint comminution (Fig. 36-6). Type I injuries were cleavage fractures without displacement, type II injuries were displaced fractures that consisted of large osteochondral fragments without comminution, and type III injuries involved all degrees of comminuted and impacted fractures. Although the presence of a fibular fracture was important for treatment, this did not alter the outcome after surgical intervention. Kellam and Waddell42 described two fracture patterns. Type A was a rotational pattern, and type B was the classic compressive pattern. In their study, the rotational pattern was found to be less common than the compressive fracture and to have a substantially better prognosis after surgery. Müller et al66 published the Comprehensive Classification of Fractures (CCF) in an effort to allow surgeons to compare the results of similar fractures. In 1996, the Orthopaedic Trauma Association (OTA)70 published a similar classification that modified the original Rüedi classification scheme. These fractures are now considered 43-A, 43-B, and 43-C fractures (Fig. 36-7). All these systems are based on plain radiographs. Since that time, recent scientific articles have been published that question the reliability and reproducibility of the Rüedi classification, specifically its accuracy in determining the severity of bone injury and the displacement of fracture fragments.20,56,96 All authors concluded that the same fracture could not be reliably and consistently classified by different reviewers, beyond the most basic fracture patterns, and therefore were of limited use in research. Tornetta and Gorup102 described the advantages of adding computed tomography (CT) imaging to the preoperative planning of these fractures. Using plain films, the authors first classified the fracture according to Rüedi and then reviewed the CT scan to determine whether any further useful information was obtained, specifically the direction of the major fracture line, the degree of comminution, and the amount of impaction. Although a more accurate assessment of the fracture was possible in every case, the most important finding was that the direction of the primary and secondary fracture lines could be more clearly identified. This caused a change in the surgical planning and care in 64% of patients. Most recently, Topliss et al101 have used CT scans to define the anatomy of the fracture and improve on the classification. They have documented a lateral disruption fracture, where the lateral border of the talus and the distal fibula was disturbed. This finding was strongly associated with an intact fibula and indicated a likely disruption of the talofibular joint. These studies have supported the routine use of CT scans to aid in understanding the fracture pattern and surgical planning. However, despite the additional information gathered from CT scans, there is still a current lack of a classification system that allows us to adequately correlate long-term outcomes for these difficult fractures.96 The diagnosis is made clinically and radiographically. The clinical appearance is that of an ankle fracture that may be either open or closed. Normal orthopaedic protocols should be used for managing the injury in the emergency department. Urgent recognition of a fracture-dislocation of the ankle is essential, and immediate reduction and splinting should be performed to minimize further injury to the soft tissue envelope. Initial radiographs, including imaging of the ankle and tibia plus fibula, should be performed. The plain films, when studied carefully, offer a wealth of information about the fracture (Fig. 36-8). When evaluating these radiographs, the surgeon should determine whether or not the fibula is fractured, the degree of articular comminution, and the amount and location of fragment impaction. Any obvious subluxations or dislocations at the tibiotalar joint, talofibular joint, or the syndesmosis should be noted, as well as any associated injuries to the hindfoot. CT scans should not routinely be obtained until after the limb has been stabilized (preferably with a spanning external fixator) because the anatomy will be distorted. Once the fracture has been pulled out to length, the CT scan becomes a useful preoperative planning tool (Fig. 36-9). The CT scan allows the surgeon to evaluate missed lesions, such as tubercle of Chaput avulsions, coronal and sagittal splits, syndesmotic disruption, coronal or sagittal fractures of the distal fibula, and bony damage to the talar dome. All of these findings are important for planning subsequent treatment (Fig. 36-10). In the setting of a pilon fracture that may be amenable to limited fixation of the tibia in conjunction with external fixation, a preoperative CT scan may be useful. Successful operative treatment for pilon fractures was initially described in the 1950s, mostly for lower-energy rotational injuries of the ankle occurring from ski injuries. Immediate fixation of these injuries, popularized by Rüedi et al83,86 and published in the European literature, showed good results after 9 years of follow-up in a substantial number of patients. These authors published their data in the English literature in 1979.85 In 1986, Ovadia and Beals71 published their results on 145 pilon fractures. The methods of treatment were divided into two groups: open reduction and internal fixation according to the AO technique and other methods. The best results were obtained by open reduction and internal fixation. In their classic 1987 textbook, Schatzker and Tile92 stated that pilon surgery should be performed soon after the injury, before the development of fracture blisters, incorporating open wounds into the surgical incisions whenever possible. As a result of these publications, internal fixation of these fractures became the standard of care in the United States by the 1990s. In 1992, McFerran et al61 reported on their operative experience with pilon fractures over a 5-year period. They experienced a 40% complication rate when immediate internal fixation was performed, and 21 of 52 fractures required 77 more procedures. Teeny and Wiss,97 in a retrospective study, evaluated 60 plafond fractures treated by internal fixation and reviewed over a follow-up period of 2.5 years. Sixty percent of the fractures were the result of high-energy trauma. Poor results occurred in 50% of the cases. The deep infection rate in Rüedi type III fractures was 37%. Of importance, the deep infection rate statistically correlated with the presence of a postoperative wound dehiscence or skin slough but not with the presence of an open fracture. The authors concluded that if anatomic reduction without soft tissue complications could not be predicted preoperatively, consideration should be given to alternative types of treatment. Using the techniques of minimal internal and external fixation of tibia fractures,95 Bone et al10 presented a series of high-energy pilon fractures treated with isolated lag screws or small plates, or both, for the articular reduction, coupled with external fixation as a neutralization device across the ankle, to align the metaphyseal components of the fracture. The external fixator was then left in place until the tibial shaft component of the fracture healed. The authors noted that their complication rate was decreased and concluded that this was due to better soft tissue management secondary to the external fixator, but they stressed the important need for anatomic reconstruction of the articular surface. Tornetta et al103 furthered this concept by using isolated lag screws combined with a hybrid fixator so that early motion of the ankle joint could be maintained. The authors first operatively stabilized the fibula and then performed an open reduction of the articular surface using lag screws. After this was accomplished, fixation of the distal metaphysis to the tibial diaphysis was performed using a hybrid ring fixator. The authors concluded that the method offered a low complication rate and had the added advantage of early joint motion. Similar results using this technique were subsequently described by many authors.8,30,54,87 Although soft tissue complications were minimized as a result of this technique, many authors began to use percutaneous, rather than open, reduction of the joint surface, either with cannulated screws or with small-wire techniques.4,61 Unfortunately, complications were not eliminated. Anglen1 reported on 61 pilon fractures treated by a single surgeon. Fracture stabilization was accomplished with the use of a hybrid external fixator (n = 34) or with internal fixation (n = 27). Patients treated with hybrid fixation had lower clinical scores, slower return to function, a higher rate of complications, more nonunions and malunions, and more infections. The author concluded that hybrid fixation did not seem to solve the problems inherent in severe pilon fractures, and the optimistic results reported in the literature using frames did not hold true in his series. Hutson and Zych40 reported on the rate of infection associated with tensioned wire fixators. They noted a 7% rate of pin-tract infections, one case of septic arthritis, and one deep infection. When performing a meta-analysis of published data on tensioned wire frames in the treatment of pilon fractures, they noted an overall pin-tract infection rate of 21%. Finally, Vives et al107 documented the risks associated with tensioned wire placement during frame application, including a 55% rate of piercing of at least one tendon and an 8% to 10% rate of impaling neurovascular structures. Complications included malreduction of the articular surface; malunion or nonunion of the tibial shaft; pin-tract, soft tissue, and bone infections; and damage to the neurovascular and tendinous structures about the ankle. As a result of these complications, consideration was again given to open reduction using plates, but in a staged manner. This concept was not new. Schatzker and Tile92 noted that in cases of massive swelling “surgery is hazardous and must be avoided” (their italics). They suggested the use of a spanning external fixator and a delay of 7 to 10 days before attempting internal fixation. Similarly, in 1990, Höntzsch et al39 documented the advantages of two-stage treatment, with a delay in surgical treatment of 2 to 3 weeks in 50 pilon fractures. In February of 1999, two landmark articles were published that reported on the results of a staged management for high-energy pilon fractures, one by Sirken et al94 and the other by Patterson and Cole.74 Both papers used a protocol in which temporary external fixation was used in conjunction with immediate fixation of the fibula, if indicated. Definitive fixation was delayed until the soft tissue envelope had improved, to allow definitive reconstruction, typically between 10 to 14 days. Both studies showed decreased wound complications and improved outcomes for these severe injuries. Staging of the procedure allows the surgeon to stabilize the injury and allows the soft tissues to improve such that soft tissue complications are minimized at the time formal open reduction and internal fixation is performed. More recently, this technique has been modified to allow partial fixation of the tibial fracture while minimizing soft tissue complications. Dunbar et al22 described a technique where tibial pilon fragments that had proximal extensions were treated with limited internal fixation through small incisions. The goal of this technique was to restore the anatomic alignment of the fragments with respect to length and rotation, which can often be difficult to obtain at the time of delayed fixation. Ketz and Sanders43 reported on pilon fractures that had displaced posterior malleolar fracture fragments. These fractures were treated with a staged protocol that used limited posterior fixation of the tibia in conjunction with fibular fixation, using a posterolateral approach. The results showed improved overall reductions with no wound complications in 28 patients. Recent studies have evaluated the role of percutaneous plating techniques for pilon fractures.2,32,34 The majority of these studies have used precontoured medial tibial locking plates. These studies reported low rates of wound complications, but there were a high number of delayed unions or nonunions, with one study having 35% healing after 6 months and a 10% nonunion rate.34 Hasenboehler et al32 had 4 of 30 patients heal at greater than 6 months, with one failure of fixation and two nonunions. Low soft tissue complications or infections were seen with both studies. Percutaneous techniques are useful in reducing the soft tissue trauma and remain a viable option for the treatment of pilon fractures, particularly in minimally displaced or nondisplaced fractures. However, there is often poor visualization of the joint, and articular reduction should not be compromised when using these techniques. When planning to treat pilon fractures with associated fibula fractures surgically, anatomic reduction of the fibula provides restoration of length and rotation of the fracture. It also can indirectly reduce tibial fragments resulting from ligamentotaxis.106 This is performed in conjunction with ankle-spanning external fixation. Surgical fixation of the fibula is best achieved with a plate and screw construct because the fracture pattern is often comminuted and malreduction is a concern. Fixation of the fibula with an intramedullary device is rarely recommended because it can lead to angulation, rotation, or shortening of the fracture, which can affect the surgeon’s subsequent ability to obtain an anatomic reduction of the tibia. Although fixation of the fibula is typically performed with external fixation initially, the authors would like to stress that it should be the treating surgeon who performs this aspect of treatment. This will ensure that further incisions or treatment strategies are not compromised because of a previous incision or malreduction from another surgeon. Although a standard midlateral extensile incision is recommended for fibular fixation, all anterior incisions should be drawn out initially, to verify that the distance between the anterior and lateral incisions is 5 to 7 cm at a minimum. This will prevent vascular compromise of the interposed flap92 and might require the surgeon to move the fibular incision posteriorly when reducing and fixing the fibula. Pin placement distally depends on the type of frame used. A simple A-frame, delta, or traveling traction frame requires a calcaneal transfixion pin.39,53 Unilateral, multiplanar frames require medial half-pins, with one placed in the talar neck and one placed in the calcaneus. Although the calcaneal pin should be placed with care to avoid the neurovascular bundle, the talar pin must be placed to avoid any planned anteromedial incisions. Caution should be used with talar neck pins because they are typically placed within the ankle joint. With all frames, the proximally placed tibial pins should be away from the planned incisions to prevent pin-tract colonization, which could infect the surgical site. Because these frames are rarely left on the patient for longer than 3 weeks, pin-tract complications are rarely seen. If the fracture is isolated, reliable patients may be sent home non–weight bearing on crutches and followed in the office. During that time, additional studies, such as CT scans, may be ordered, and surgical intervention may be planned once skin wrinkling is seen, generally at 10 to 14 days.42,54 Late-stage fixation can be performed through a variety of approaches to the ankle for the operative treatment of pilon fractures, including a straight anterior incision,58 a medial incision (according to Schatzker93), and the lateral Böhler approach (according to Herscovici37), or a posterolateral approach.33,57 Therefore, when planning the fibula incision, the tibial incision should be drawn out so that the placement of the fibula incision is correct. 1. The patient is placed into the prone position. The posterolateral incision begins directly between the posterolateral border of the fibula and the medial aspect of the Achilles tendon. Care should be taken because the sural neurovascular structures run in the subcutaneous tissues. Full-thickness flaps should be created. 2. Dissection should first be carried out laterally to expose the peroneal fascial. This is released from the lateral border of the fibula, and the peroneal tendons are retracted medially to expose the distal fibular fracture. Care is taken to anatomically reduce the fibula, and a posterior or posterolateral plating technique can be used. 3. The peroneal tendons are then retracted laterally, and the interval between the peroneals and flexor hallucis longus (FHL) is dissected. The peroneal artery lies proximally in the dissection plane. The distal aspect of the posterior tibia is exposed. Often, there is a spike of bone from the posterior malleolar fragment that can serve as a “key” for anatomic reduction. A small or mini-fragment compression plate is then applied to span the fracture in a buttress fashion and secured proximally with cortical screws. If screws are required distally to stabilize the posterior malleolar fragment(s), a short (10-14 mm) unicortical screw should be used to prevent interference with the subsequent reduction of the anterior fragments. Small or mini-fragment locking plates are useful for this purpose (Fig. 36-11). This approach allows excellent visualization of the fibula and posterior tibia to allow fixation. There is a healthy muscular bed underlying the incision from the peroneal and FHL muscle bellies. Care should be taken not to strip the posterior tibia because this can destabilize the posterior tibiofibular ligaments and create syndesmotic instability. The main benefit of posterior tibial plating is anatomic reduction of the posterior tibial fragments, and this creates a stable posterior buttress for future fracture reduction and stabilization from future anterior approaches (Fig. 36-12). 1. The anteromedial approach91 begins at the level of the distal shaft of the tibia, just lateral to the anterior crest and continues distally, staying medial to the anterior tibial tendon. As it crosses the ankle, it sweeps along the inferior portion of the medial malleolus. The skin should be taken together with the subcutaneous tissue and the periosteum in a full-thickness flap to prevent separation of the medial skin from its periosteal blood supply. 2. Although the anterior tibial tendon should be left in its sheath for this dissection, this is difficult to do in practice, and the sheath is often incised so that the tendon dislocates out of the sheath (as a practical matter, this is of little concern postoperatively). 3. The exposure of the joint should be through the major tears in the soft tissue envelope. The joint capsule can be incised in line with the skin incision if an incision is necessary for visualizing the articular surface.
Pilon Fractures
Anatomy
Mechanism of Injury
Fracture Classification
Diagnosis and Radiologic Evaluation
Historical Treatment Options
Current Treatment Options
Staged Open Reduction and Internal Fixation
Portable Traction
Approach
Overview
Posterolateral Approach
Anteromedial Approach
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree