Pilon Fractures
George S. Gumann
Justin J. Fleming
The opinions of the authors are their private views and are not to be considered as representative of official policy of the U.S. Army Medical Department.
The pilon fracture was first described by Destot (1) in 1911. A pilon fracture involves the distal tibial metaphysis with extension into the ankle joint. These injuries are generally produced by either axially/compressive loading patterns or rotational forces. Some fractures may exhibit elements of both mechanisms. Compressive-type fractures are high-velocity injuries in which the talus impacts the distal portion of the tibia, producing bony comminution, varying degrees of displacement, major articular derangement, and significant soft tissue damage. Due to these factors, the overall prognosis is very problematic. There is usually, but not always, an associated fibular fracture. Rotational forces produce a low-velocity-type injury with a spiral configuration of the distal tibia, which may or may not enter the ankle joint. This results in less complex articular injury. The subsequent soft tissue injury is generally less morbid and typically allows for a more favorable prognosis. Pilon fractures represent less than 1% of all lower extremity fractures and 1% to 10% of all tibial fractures (2,3). Approximately 20% to 25% of these injuries are open. One-third are associated with other injuries. Common mechanisms of injury include motor vehicle accidents, falls from heights, and skiing accidents.
Some fracture patterns are dictated by the position of the foot at the time of injury. If the foot is dorsiflexed, the anterior portion of the talar dome will impact and fracture the anterior aspect of the tibial plafond. If the foot is plantarflexed, then the posterior aspect of the tibial plafond will be fractured. A neutrally positioned foot will cause a Y-shaped fracture resulting in anterior and posterior fragments. An inverted foot will produce fractures more on the medial aspect of the tibia, while an everted foot will involve the lateral aspect (4). Pilon fractures are complex injuries, and successful treatment requires great expertise.
CLASSIFICATION
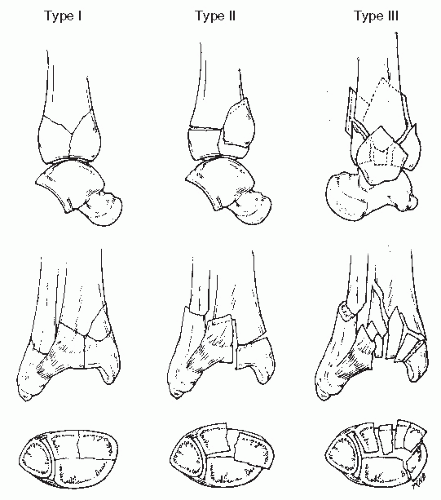
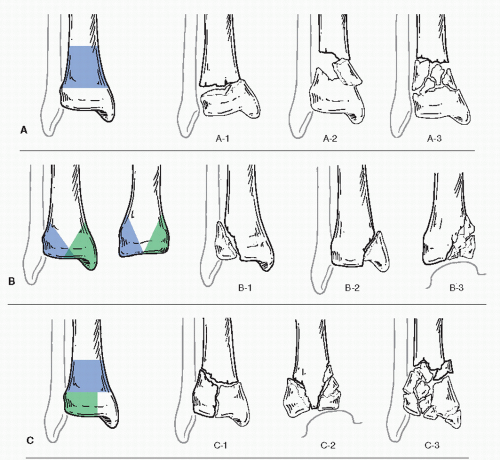
Historically, the classification system advocated by Ruedi and Allgower (5) has been commonly used to describe pilon fractures. There are three fracture types. Type I is a fracture of the distal tibia without significant displacement. Type II is a fracture of the distal tibia with significant displacement. Type III is a fracture of the distal tibia with severe comminution, significant displacement, and loss of the weight-bearing portion of the tibial plafond (Fig. 110.1). More recently, the AO/OTA classification of pilon fractures has been utilized. Type A is extra-articular, type B is partially articular, and type C is completely articular. There are subtypes of each classification based on increasing complexity of the articular and metaphyseal components (Fig. 110.2) (4).
Lauge-Hansen (6) also attempted to describe this fracture pattern with his classification of pronation-dorsiflexion injuries. They were divided into four stages. Stage I is a fracture of the medial malleolus. Stage II is a fracture of the anterior aspect of the distal tibia. Stage III is a fracture of the fibula. Stage IV is a transverse fracture of the distal tibia.
Kellam and Waddell (7) suggested two distinct fracture patterns that were correlated to the mechanism of injury. Type A was a fracture with two or more large tibial articular fragments, minimal or no anterior comminution, and usually a transverse or short oblique fracture of the fibula above the plafond. This fracture pattern is produced by a primary rotation force with minimal axial compression. Type B was a compressive fracture demonstrating multiple tibial fragments, a narrowed ankle joint, significant anterior tibial comminution, and superior migration of the talus. The injury is caused by a severe axial compression force but is not always associated with a fibular fracture. Kellam and Waddell (7) note that the rotation injury has less soft tissue compromise and a better prognosis. Tile (8) agrees with this classification but identifies an axial compression fracture, a shear (tension) fracture, and a combined pattern.
Ovadia and Beals (9) have proposed another classification system. This classification has five categories based on the degree of comminution and displacement. Type I fractures enter the ankle joint but are nondisplaced. Type II fractures enter the ankle joint and are minimally displaced. Type III fractures enter the ankle joint and are moderately displaced with several large fragments. Type IV fractures are also moderately displaced, intra-articular, and associated with large metaphyseal defects. Type V fractures have severe comminution of the distal tibial metaphysis and the articular surface.
ASSESSMENT
The assessment of these injuries typically begins in the emergency room. It may be an isolated injury or a component in the polytrauma patient. The examination must be complete and systemic as concomitant contra- and ipsilateral injuries can occur. Appropriate communication with other services (trauma, vascular surgery, plastics, orthopaedics) may be essential to successful management. There may or may not be gross deformity of the distal leg and ankle. Examine the soft tissue envelop for the possibility of an open fracture or any dermal lesions. There will be diffuse tenderness involving the ankle and distal tibia. Initial and possibly interval neurovascular evaluation is required. The compression-type pilon fractures tend to produce significant soft tissue edema and have the potential to develop fracture blisters in 24 to 72 hours.
RADIOGRAPHIC ASSESSMENT
Radiographs of the foot, ankle, and leg should be obtained. Gross deformity, degree of tibial articular and metaphyseal comminution, and articular displacement will be demonstrated.
The presence, level, and complexity of the fibular fracture will be noted if present. Contralateral films of the ankle may be utilized at the time of definitive surgery as a template for reconstruction if necessary.
The presence, level, and complexity of the fibular fracture will be noted if present. Contralateral films of the ankle may be utilized at the time of definitive surgery as a template for reconstruction if necessary.
Acute CT scanning of axial compression pilon fractures typically provides little value. CT evaluation following application of a spanning external fixator is more informative because of the gross reduction in fracture alignment. However, it may be beneficial in determining articular involvement of distal tibial fractures that appear extra-articular radiographically, in simple fractures with little displacement or in rotational pilon fractures.
TREATMENT
Pilon fractures are complex injuries involving the soft tissue envelop along with the osseous structures of the distal leg and ankle. There are varying degrees of soft tissue damage, deformity, osseous comminution, intra-articular involvement, and metaphyseal loss of bone. After completing the history, physical examination, radiographs, any appropriate laboratory studies, necessary consultations, and resuscitation measures for the patient, the next step is to stabilize the fracture. Clinical examination and radiographic studies readily demonstrate a pilon fracture. Any significant deformity should be reduced in the emergency room under conscious sedation unless expedient transportation to the operating room is possible. The injured extremity should be protected with a splint or if surgery is to be delayed, a padded dressing applied along with a splint or in a bivalved cast. The factors that need to be considered include patient’s age, comorbid medical issues, activity level, employment, postinjury expectations, ability to tolerate potential complications, the experience of the surgeon, the degree of osseous involvement, and the soft tissue damage.
Today, it is recognized that soft tissue management is equally important as osseous treatment. Tscherne and Gotzen (10) have developed a grading system for soft tissue damage. A grade 0 injury involves a closed fracture with minimal soft tissue damage. There is an indirect mechanism of injury producing a simple fracture configuration. A grade I injury is a closed fracture that has a contusion or superficial abrasion. The pressure against the skin occurs as it is stretched over the fracture margins. There is mild to moderately severe fracture configuration. A grade II injury is a closed fracture with deep abrasion with local skin and muscle contusion. There is a moderately severe to severe fracture configuration. A grade III injury is a closed fracture with extensive contusion or crushing of the skin and muscle. There can be subcutaneous avulsions, compartment syndrome, or rupture of a major blood vessel. Compression-type pilon fractures tend to lend themselves to significant edema and fracture blister formation.
HISTORICAL PERSPECTIVE
At one time, pilon fractures were considered nearly impossible to surgically repair. Ruoff and Snider (11) recommended traction as the best treatment option. They were treated with casts, calcaneal pin traction, and pins in plaster technique. Cast management is still appropriate for nondisplaced pilon fractures; however, they are uncommon. Both calcaneal pin traction and pins in plaster have been eclipsed by the use of external fixation. In 1969, Ruedi and Allgower (5) in their landmark work reported on a series of 84 consecutive pilon fractures treated by the principles of the Swiss Study Group/AO. These principles include the following:
Reconstruction of the fibular fracture
Reconstruction of the tibial articular surface
Cancellous bone graft to fill the distal tibial metaphyseal defect
Buttress plate application to the medial aspect of the tibia
This was the first revolution in the treatment of pilon fractures. Seventy-eight fractures were evaluated with an average follow-up of 50.3 months. Seventy-four percent of the patients obtained a good to excellent functional result. Only 9% of patients underwent ankle arthrodesis, and 5% required corrective osteotomy. Seventy-five percent of the fractures were caused by skiing accidents, and only 33% were type III injuries. In a second study, Ruedi (12) reviewed 54 of the original 84 patients 9 years after surgery. He noted that 68% of the results had not changed, whereas 22% had a general improvement. Only in 10% of the patients was there an aggravation of their symptoms.
The important work of Ruedi and Allgower led to an enthusiasm for open reduction with internal fixation (ORIF) (5,12). This is because their conclusion indicated that pilon fractures could be reconstructed and that anatomic reduction of the ankle was necessary to obtain a good result. They also noted that traumatic arthritis would normally develop within 1 year if it was to occur. In addition, some patients could actually improve with time, and patients that demonstrated a good result after 1 year would usually continue to do well.
However, this study later came into question for the high percentage of good results. It was noted that the patient population
was fairly homogeneous, being younger, athletic individuals who sustained lower-velocity-type fractures. To counter this criticism, Ruedi and Allgower (13) reported another series of 75 patients. Forty-seven percent of the patients sustained their fracture during sporting events, 34% had road or work accidents, and 19% had injuries occurring at home. The open fracture rate was 4%. Classification of the fractures demonstrated 25% were type I, 28% type II, and 47% type III. Subjective results from the patients were 80% good, whereas the author’s objective criteria showed 69.4% good results. Only 8% of patients had wound healing problems, and there were no cases of osteomyelitis. The arthrodesis rate was 5.3%. The slightly lower number of good results was attributed to the differences in average patient age, mechanisms of injury, and the experience of the surgeon.
was fairly homogeneous, being younger, athletic individuals who sustained lower-velocity-type fractures. To counter this criticism, Ruedi and Allgower (13) reported another series of 75 patients. Forty-seven percent of the patients sustained their fracture during sporting events, 34% had road or work accidents, and 19% had injuries occurring at home. The open fracture rate was 4%. Classification of the fractures demonstrated 25% were type I, 28% type II, and 47% type III. Subjective results from the patients were 80% good, whereas the author’s objective criteria showed 69.4% good results. Only 8% of patients had wound healing problems, and there were no cases of osteomyelitis. The arthrodesis rate was 5.3%. The slightly lower number of good results was attributed to the differences in average patient age, mechanisms of injury, and the experience of the surgeon.
In 1977, Heim and Nasser (14) reviewed a series of 128 patients with 90% good functional results. Heim was the principal surgeon, and 90% of the injuries involved skiing. In 1979, Kellam and Waddell (7) reported their results in 26 cases of pilon fractures. Surgical treatment of a shearing, rotationaltype fracture without major articular impaction yielded 84% good results. However, fractures of the axial compression type with impaction and comminution achieved good results in 53% of patients. From these statistics, it was concluded that the type of fracture had a significant impact on the final results. They also confirmed previous reports that traumatic arthritis would occur within 1 year in patients destined for this sequelae (5,12). The incidence of subsequent arthrosis was directly related to the degree of articular damage and the congruity of the articular surface. It was speculated that avascular necrosis of the smaller, comminuted fragments of subchondral bone readily led to progressive deformity accelerating the arthritic process (7). Interestingly, Resch et al (15) reported, in 1986, if there was poor joint surface reconstruction after surgery, the incidence of late arthritis was higher than in patients managed nonsurgically.
TRADITIONAL OPEN REDUCTION WITH INTERNAL FIXATION
After the articles by Ruedi and Allgower, ORIF became the mainstay of pilon fracture management (5,7,12,13 and 14). Type I fractures (nondisplaced) were normally managed with cast immobilization but are rare injuries. Type II fractures lent themselves well to ORIF with reasonable expectations of obtaining an anatomic reconstruction. However, the type III fractures remained problematic. Failure to achieve an anatomic reduction with stable fixation would result in an increased risk of complications in
an already highly traumatized extremity. A critical decision was the appropriate timing for a surgical procedure. It was thought surgery should be performed as soon after the injury as possible. This usually meant within 8 to 12 hours before the onset of significant edema and the development of fracture blisters. If surgery was to be delayed, then one should consider waiting 7 to 10 days for the local skin condition to stabilize.
an already highly traumatized extremity. A critical decision was the appropriate timing for a surgical procedure. It was thought surgery should be performed as soon after the injury as possible. This usually meant within 8 to 12 hours before the onset of significant edema and the development of fracture blisters. If surgery was to be delayed, then one should consider waiting 7 to 10 days for the local skin condition to stabilize.
If surgery was delayed, the patient was evaluated for possible compartment syndrome. Fracture blister formation could occur and represents a separation of the epidermis and dermal layers. They can be filled with a serous or hemorrhagic fluid. Hemorrhagic fracture blisters indicate a more significant soft tissue injury. The fluid is sterile inside a fracture blister unless it is ruptured (16). The best advice was not to operate through fracture blisters. Small, unruptured, serous filled blisters away from the incisional site did not necessarily preclude surgery. However, hemorrhagic fracture blisters were a contraindication to surgery. Varella et al (17) reported a 60% incidence of infection when surgery was performed through open fracture blisters. Fracture blisters can be allowed to resolve by themselves or be débrided. Personal preference is débridement followed with wet to dry dressings and periodic air drying. With a pilon fracture awaiting surgery, this was best accomplished by placing the patient in a cast followed by windowing to allow wound care. The cast offered some stabity, which decreased the pain and prevented unnecessary movement of the soft tissue and osseous structures. If the patient was in an external fixator, this process is made easier.
The traditional AO approach for pilon fractures was two incisions assuming both the fibula and tibia are fractured. The fibula was approached by a posterolateral incision and the tibia by an anteromedial incision. Both the fibular and tibial fractures were exposed prior to definitive reduction. The posterolateral incision allowed access to the fibula, which was directly reduced and fixated usually with a combination of screws and plate. Fibular reconstruction usually preceded that of the tibia. The large tibial incision started 1 cm lateral to the crest of the distal tibial shaft and then curved over the anteromedial aspect of the medial malleolus. The important point was to maintain a 7-cm skin bridge between the two incisions to prevent necrosis. If only the tibia was fractured, then the incision was placed anteriorly, anterolaterally, anteromedially, medially, or posteromedially depending on the fracture configuration. Sometimes, even an isolated tibial fracture might require a two-incisional approach. Incision placement was along a major fracture line and guided by the CT scan. The dissection is carried to bone without raising soft tissue flaps, following the planes created by the fracture avoiding further devitalization of the tissue. The fracture fragments were reduced under direct visualization using the talus as a template. An effort was made to reduce every fragment anatomically. Bone fragments were provisionally fixated with guide pins, Kirschner wires (K-wires), and reduction forceps. A cancellous bone graft was placed in the metaphyseal defect. To rigidly fixate the fracture and to prevent late varus deformity, a buttress plate was usually applied to the medial aspect of the tibia. The plate could also be applied to the anterolateral, anterior, or, rarely, the posterior aspect of the tibia depending on the fracture configuration. There were several different styles of plates that could be utilized, such as the cloverleaf, spoon, or limited contact dynamic compression plate (LCDCP). Lag screws could be placed through or outside the plate to obtain interfragmental compression of the fracture fragments. After the plate was applied to the tibia, final intraoperative radiographs were obtained to assess if the reduction was anatomic and placement of the internal fixation appropriate (Fig. 110.3).
EXTERNAL FIXATION WITH OR WITHOUT LIMITED INTERNAL FIXATION
The second revolution in pilon fracture management was external fixation with or without limited ORIF (Fig. 110.4). This technique was introduced by Leach (18) in 1964. Scheck (19), in 1965, using the same technique reported satisfactory results in five cases of pilon fractures in which four of the injuries were open. External fixation with or without internal fixation became popular because of experiences with traditional ORIF that resulted in significant decrease in functional results and an increased rate of complications in pilon fractures, especially the type III (20,21,22 and 23). In a series of 19 patients, Pierce and Heinrich (20) reported poor results despite treatment by varied methods. Ovadia and Beals (9) reviewed 145 pilon fractures, 80 of which were treated with traditional ORIF. They developed their own classification system and reported that the fracture type was extremely important in determining the outcome. Their type I, II, and III fractures had a 70% good to excellent result. However, their type IV and V fractures representing 63 injuries, with 34 undergoing ORIF, demonstrated 47% good to excellent results. The infection rate was 6%, and the arthrodesis rate 12%. In 1986, Dillin and Slaubaugh (21) reported on eight patients with severe pilon fractures who underwent ORIF. In this group, 100% developed either wound breakdown, chronic drainage, or osteomyelitis. All eight patients required additional procedures.
In 1983, Bourne et al (22) reported on 42 pilon fractures, nine of which were open injuries. In 27% of their cases, other injuries were present. Two patients had neurovascular compromise. The fractures were categorized in the Ruedi and Allgower system as type I (26%), type II (29%), and type III (45%). The results were reported as type I 86% good to fair, type II 80% good to fair, and type III 44% good to fair. In the type III fractures, the nonunion rate was 25%, the infection rate 13%, and the arthrodesis rate 32%. Arthrodesis was performed in seven fractures (17%) with six of the patients having type III injuries. Bourne (3), in 1989, reported again on the 42 pilon fractures with a follow-up at a mean of 53 months after treatment. He noted that type I fractures were usually caused by a torsion mechanism, whereas the type II and III fractures were associated with high-velocity injuries. The results indicated that type I and type II fractures were amenable to anatomic reduction and stable fixation with an 80% success rate. However, the type III fractures presented a more difficult problem and had a satisfactory outcome in only 32% of patients.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree