CHAPTER 79 Physical Examination of the Lumbar Spine
INTRODUCTION
Low back pain (LBP) is one of the most common disorders in the industrialized world1–4 and it is a frequent complaint in patients with musculoskeletal disorder.5 Lifetime incidence of LBP in the general population in the United States is 50–80%.1 LBP is the most frequent cause of work-related disability in workers younger than 45 years old, and second only to arthritis in people 45–65 years old.4
INSPECTION
Anterior inspection
With the anterior inspection, the examiner must begin with the head. The position of the head should be symmetrical on the shoulders. The shoulders are usually equal in height; although in many people, especially overhead athletes, the dominant shoulder is slightly lower.6 The anterior superior iliac spine, the iliac crest and the greater trochanter should be equal in height. The patellas should also be equal in height and face anteriorly. Examiner should identify genu valgus/varus. The medial malleoli should also be equal in height. The clinician should look for varus/valgus deformity of the forefoot and prone/supine position of the feet and note the foot arch.
Posterior inspection
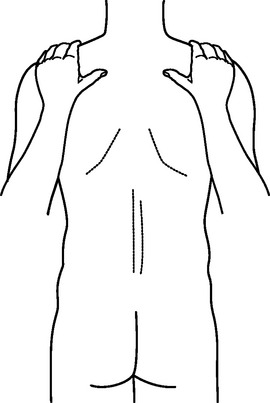
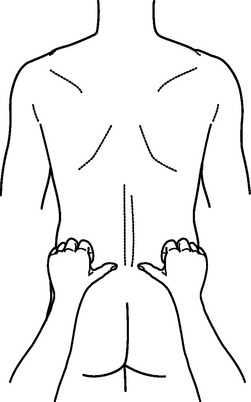
Posterior observation is the most crucial aspect of inspection in patients with LBP. Symmetry of the head and shoulder height should be reexamined in this plane (Fig. 79.1). Scapular symmetry is assessed. The spine of scapula is normally at the T3 level. Inferior angle of scapula is at the level of T8. The clinician should assess symmetry of the scapula at these levels. The distance of inferior angle of scapula from the spine is also noteworthy. With inspection of the spine, the clinician should search for tissue asymmetry, signs of edema, or erythema. The spinal column should be evaluated for signs of scoliosis. Asymmetrical paraspinal fullness is also clinically significant and should be noted. The waist lines should be equal in height. Iliac crests should be symmetrical (Fig. 79.2). Gluteal folds, popliteal creases and medial malleoli should also be symmetrical bilaterally. The Achilles tendons and the heels should be midline.
RANGE OF MOTION
Assessment of range of motion (ROM) of the lumbar spine is a critical aspect of lumbar spine examination. It is an important tool in evaluation of recovery in a patient with low back pain. Abnormal spinal motion is associated with abnormal spinal mechanics.7 Motion of the lumbar spine must be assessed in all planes including flexion, extension, side bending, and rotation. ROM can be done actively or passively. If passive ROM is performed, caution should be made not to put too much pressure on a person who expresses discomfort at a certain angle. Key findings that the examiner should look for are end-range pain and side-to-side asymmetry. Examiners should be aware that lumbar flexion is composed of lumbar ROM as well as pelvic motion.8,9 Lumbar motion occurs prior to pelvic movement. This is very important, especially in a subgroup of patients who are flexible enough to bend forward and touch their toes using only hip motion.10 For this reason, when asking a patient to flex fully, one should also look for reversal of lumbar lordosis. Caillet has shown that the first 45 degrees of flexion consists of reversal of the lumbar lordosis with the remainder of motion secondary to pelvic rotation.11,12 Generally, the first 60 degrees of flexion are attributed to the lumbar spine. However, there have not been any accurate measures to confirm this observation.13
The most accurate method to measure the movement of the vertebrae is through radiologic studies. However, use of long-term radiography is not realistic due to risk of radiation and cost.10,14 Various methods have been utilized in measurement of the lumbar spine. Burdett et al.15 and Portek et al.16 both performed studies comparing plain radiographs with various external measurements. However, the findings were inconsistent. Mayer et al.10 compared flexion and extension measured by an inclinometer to radiographic films and found no statistical significance between the two measurements. Saur et al.14 also compared lumbar ROM in flexion and extension with and without radiologic determination using an inclinometer. The results showed that flexion alone demonstrated a strong correlation (r=0.95) while extension showed a more moderate though good correlation (r=0.82).
Ng et al.17 measured normative values in 35 healthy men in all three planes using pelvic restraint as well as lumbar lordosis. They found good reliability in all measurements. The ICC and Pearson’s r values were greater than 0.9. Their normative values in degrees are shown in Table 79.1.
Table 79.1 Lumbar range of movement in 35 healthy men
| Type of motion | Degrees of motion |
|---|---|
| Flexion | 52 + 9 |
| Extension | 19 + 9 |
| Flexion & extension (sagittal plane) | 71 + 12 |
| Right lateral flexion | 31 + 6 |
| Left lateral flexion | 30 + 6 |
| Lateral flexion (coronal plane) | 60 + 11 |
| Right axial rotation | 32 + 9 |
| Left axial rotation | 33 + 9 |
| Axial rotation (transverse plane) | 65 + 17 |
| Lumbar lordosis | 24 + 8 |
From Ng et al.17
The examiner should also be aware of variables affecting lumbar range of motion. McGregor et al. studied spinal motion in 203 normal subjects and concluded that range of motion is affected by age and sex. They also found that occupation and body mass index have little or no effect on spinal range of motion.18 Mellin determined that age had a significant, though indirect relation with spinal ROM.19 Sullivan et al.20 demonstrated a significant difference between flexion and extension angle of men and women, but a small difference between genders for total lumbar sagittal ROM; they also showed total sagittal ROM, flexion and extension angle to decrease with an increase in age.
The examiner must be able to eliminate sources of error in measurement, such as improper technique and poor standardization. Studies have shown total lumbar range of motion to be variable in the afternoon as compared to the morning.21 The clinician should also bear in mind that decreased lumbar ROM in a patient who is asymptomatic is not predictive of low back pain.
Fingertip to floor test
Measurement of fingertip to the floor is a simple test which is commonly used in clinical practice. The patient is asked to stand erect and bend forward as far as possible with the knees fully extended and heel on the floor. The distance between the tip of the middle finger and the floor is then measured. This test, however, can only be used as a crude method of measuring lumbar function because it does not take into account the contribution of pelvic movement and tightness of the hamstrings.22 Merritt et al.23 found the mean coefficient of variation for this test to have an inter-examiner reproducibility of 83% and an intra-examiner reproducibility of 76.4%. Gill et al.24 found the intra-examiner coefficient of variation to be 14%. Thomas et al.25 performed fingertip to floor on 344 patients with new-onset low back pain and 118 individuals without any history of back pain and found the test to have a sensitivity of 45.3% with a specificity of 88.8%.
Fingertip to floor distance is also used in lateral flexion. The patient is asked to stand with the head and buttock pressed firmly against the wall and bend sideways as far as possible without bending the knees. Flexion is measured as the distance covered by the fingertips on the lateral thigh. Thomas et al. showed right lateral flexion to have a sensitivity of 23.1% and a specificity of 94.1%. Left lateral flexion had a sensitivity of 26.1% and a specificity of 92.4%.25
Schober test
The Schober test was first described by Schober in 1937 to measure segmental motion of the lumbar spine. The examiner marks the S1 spinous process and measures and marks 10 cm above the first mark. Patient is then asked to flex forward as far as possible. The increased distance is then measured. In absence of any pathology, the distance should increase by 4–5 cm.26 This test, however, is only utilized to measure lumbar flexion. The intra-tester variation with this test is reported as 4.8%.27
Modified Schober test
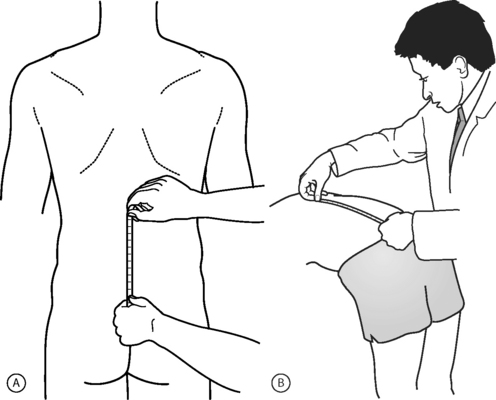
Macrae and Wright modified the Schober test in 1971.28 The examiner draws a line between the posterior superior iliac spines with the patient standing erect. The distance 10 cm above and 5 cm below is measured. The patient is then asked to fully forward flex. The distance between the two marks is re-measured.24,28 Normal values are consistent with a greater than 5 cm increase in distance between the two marks when measured in full flexion (Fig. 79.3).
Thomas et al. compared standing extension, lateral flexion, modified Schober test, finger to floor, and knee extension in a study comparing 344 patients with back pain to 118 patients with no history of back pain and found modified Schober test to be the most specific: 94.9%. However, they found the sensitivity of the test to be only 25.3%.25 Gill et al.24 compared this test to fingertip to floor test, the two-inclinometer method, and photometric technique. They found modified Schober test to have the best repeatability and good intra-tester reliability. They found the coefficient of variation of this test to be 0.9% in flexion and 2.8% in extension. Meritt et al.23 found inter-examiner reproducibility to be 6.3% and intra-examiner reproducibility to be 6.6% with the modified Schober test in flexion and suggested that it be added to a routine lumbar spine examination.23 Reynolds29 found the coefficient of variation to be 11.65% in flexion and 21.57% in extension. He found the test to have good reliability with Pearson coefficients of 0.59 for lumbar flexion and 0.75 for extension. Fitzgerald et al. showed the Pearson coefficient to be 1.0 in lumbar flexion and 0.88 in lumbar extension.30
Miller et al.31 also noted a good inter-rater reliability of the modified Schober method, while Stankovic et al. showed this test to have an intra-rater and inter-rater correlation coefficient of 0.95 and 0.94, respectively.32
The modified Schober test is a simple procedure which can easily be performed in the office setting. It is specific but not sensitive when comparing patients with and without low back pain.33 It is also fairly reproducible.
Modified, modified Schober test
This test was described by Van Adrichem and van der Korst. The patient stands erect with feet 15 cm apart. A horizontal line is made across the posterior superior iliac spine. Another horizontal line is drawn 15 cm superior to the first line. Patient is then asked to flex or extend as far as possible. The new distance between the two lines is measured and the distance is recorded.34 No studies to date have evaluated sensitivity and specificity of the modified, modified Schober test. Van Adrichem and van der Korst reported the Pearson correlation coefficient of this test to be 0.78–0.89 in lumbar flexion and 0.69–0.91 in lumbar extension. The inter-rater reliability was 0.72 in flexion and 0.76 in extension.
Inclinometer
This technique requires the use of more advanced equipment for measurement of motion. An inclinometer is a handheld, circular, fluid-filled disc that has a weighted gravity pendulum attached to it that is maintained in the vertical direction. It is graduated by 0.5 degree intervals over 360 degrees. Various studies have described the use of this device using a single inclinometer and dual inclinometers. The use of dual inclinometer has shown to have superior results. The American Medical Association has recommended the dual inclinometer technique.35 This method is attributed to Loebl and Troup.36,37 Mayer later modified the test in 1984.10 One inclinometer is placed over the sacrum with the patient in the erect position. The second inclinometer is placed on the T12–L1 spinous process. These areas are marked. The patient is then asked to fully forward flex while the readings of the two inclinometers are recorded. The difference between the readings in the inclinometer in the T12–L1 area measures the rotation of the torso, whereas the difference between the readings in the sacral area measures the rotation of the pelvis. Range of motion in lumbar flexion is then calculated by subtraction of the sacral rotation from the torso rotation (Fig. 79.4). This process can also be done in extension.10,24
Mayer et al. reported results using single and double inclinometry and found no difference between the two techniques.10,24 However, Nattrass et al.,38 comparing goniometry and dual inclinometry, found intra-rater reliability to be poor, with a Pearson correlation coefficient ranging 0.38–0.54. The measurement of error for thoracolumbar and lumbar movements ranged from 9 degrees to 30 degrees.38
A review of inter- and intra-tester reliability using single and dual inclinometer technique shows varying results. Using a standard goniometer, Reynolds29 found the test to have an inter-tester reliability of 0.75 in flexion and 0.87 in extension. Burdett et al.15 used a parallelogram goniometer and found inter-tester reliability to be 0.73 in flexion and 0.27 in extension. Saur et al.14 demonstrated high reliability using a standard inclinometer with an inter-tester reliability of 0.88 and 0.94 in flexion and extension, respectively. They also showed a very close correlation (r=0.93) between the measurements taken with radiographic studies as compared to the ones taken without. Merritt et al.23 found intra-tester coefficient of variation to be 9.6 in flexion and 65.4 in extension and inter-tester coefficient of variation to be 13.4 in flexion and 50.7 in extension.
Using a dual inclinometer technique, Dillard et al.39 found a high inter-examiner reliability in flexion (r=0.78) with a poor inter-examiner reliability in extension (r=0.27). Nattrass et al.38 established an intra-tester reliability of 0.90 in flexion and 0.70 in extension. Williams et al.40 concluded inter-tester reliability to be 0.60 in flexion and 0.48 in extension compared to 0.72 and 0.76, respectively, in flexion and extension for the modified, modified Schober test. They also found intra-tester reliability to be poor with the reliability ranging 0.13–0.87 in flexion and 0.28–0.66 in extension. Mellin19,41,42 used dual inclinometers and found inter-tester reliability to be 0.86 in flexion and 0.93 in extension. Gill et al.24 looked at the range of motion of the lumbar spine comparing dual inclinometer, fingertip to floor, and modified Schober test. They found the modified Schober test to be the most repeatable test. Intra-tester coefficient of variation (COV) of dual inclinometer was 9.3–33.9 in flexion and 3.6–4.7 in extension as opposed to modified Schober test with COV of 0.9 and 2.8, respectively, in flexion and extension.
Other studies have used different versions of goniometers. A computerized goniometer (CA 6000) was used by Dopf et al. who found inter-examiner correlation coefficient to be 0.76 and intra-examiner correlation coefficient to be 0.936.43 Ng et al.17 utilized a modified inclinometer with a pelvic restraint. Their data showed intra-tester reliability to be 0.87 in flexion and 0.92 in extension.
The inclinometer is also used in lateral rotation. The placement of the inclinometer is identical to the spots used in flexion and extension. The first inclinometer is placed over the sacrum with a second inclinometer being place over the T12–L1 spinous process. The patient is then asked to bend laterally. The degree of lumbar lateral flexion is obtained by subtracting the values from the sacral goniometer from the one over the T12–L1 interspace.44 Dillard et al.39 found the intra-tester reliability in lateral flexion to be 0.66 using a double inclinometer. Using the same device, Nattrass et al.38 found that lateral flexion intra-tester reliability ranged 0.89–0.90. Ng et al.17 showed an intra-tester reliability of 0.96 in right lateral flexion and 0.94 in left lateral flexion using a modified inclinometer with pelvic restraint.
PALPATION
Palpation of the lumbar spine should be performed both in the standing and in the prone position. It is crucial to know certain landmarks in order to better isolate the symptomatic level. An imaginary horizontal line through the peak level of iliac crests crosses the lumbar spine at the L4 spinous process and through the tubercles of the iliac crests is the L5 spinous process. As the fingers move inferiorly from the L5 spinous process, the posterior superior iliac spine (PSIS) is palpated. The simplest way to find the PSIS is by placing the fingers on the iliac crest and moving them posteriorly until they rest on the two small dimples located at the base of the sacrum. The PSIS is at the level of the second sacral vertebra. The upper margin of the greater sciatic notch is at the level of the third sacral vertebra. Moving caudally from the PSIS, the ischial tuberosity (IT) is palpated, the origin of the hamstring muscles. Drawing a line from the PSIS to IT, the posterior inferior iliac spine (PIIS) is located 5 cm distally with the ischial spine 10 cm caudal. The ischial spine is opposite the first portion of the coccyx. In the standing position, a horizontal line can be drawn joining the pubic tubercle to the top of the greater trochanter; at the midline, the acetabulum and the head of the femur are located.
In the prone position, the spinous processes are palpated along the midline with the transverse processes palpated approximately 4 cm laterally in the same fashion. In a patient with lumbar spine dysfunction, the clinician must palpate above and below the lumbar area to assess the etiology of patient’s discomfort. In the prone position, other structures to be palpated include the PSIS, iliac crests, greater trochanters, ischial tuberosities, along with various muscle groups including the paraspinals, tensor fascia lata, gluteus maximus, gluteus medius, and piriformis. The examiner should look for tissue texture changes from side to side, tender points, and trigger points. A trigger point is a tender muscle area that, when palpated, has a band-like quality and causes radiation of pain to an area distant to the area palpated. Deyo et al.45 described spine and paraspinal tenderness as having low specificity and poor reproducibility. Importantly, they described vertebral tenderness to be suggestive of spinal infection (sensitivity 0.86).
FLEXIBILITY
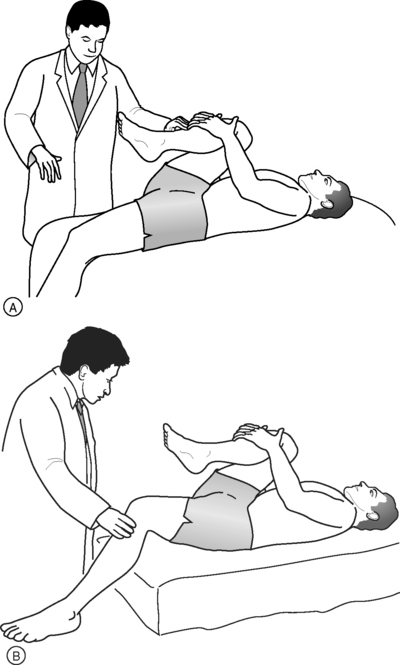
Thomas test
This maneuver examines the flexibility of the iliopsoas. The test is performed with the patient in the supine position. The patient is asked to flex the hip to the chest (Fig. 79.5). Elevation of the opposite hip off the table would indicate hip flexure tightness. Kujala et al.46 studied factors associated with low back pain in 138 adolescents (100 athletes and 38 non-athletes). They found tightness of the hip flexors to be the one factor associated with incidence of low back pain.
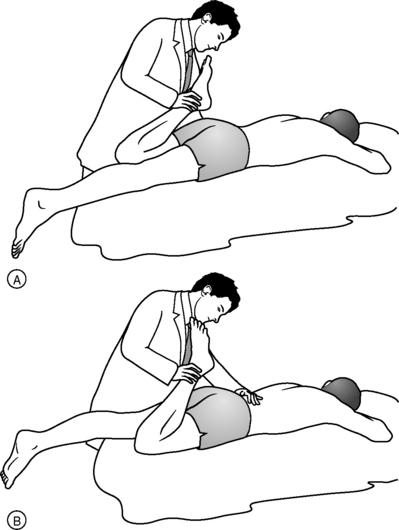
Ely’s test
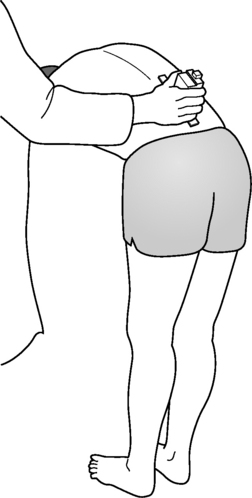
Ely’s test assesses rectus femoris flexibility. The patient lies prone on the examining table. The clinician passively flexes the knee maximally, approximating the ankle to the buttock (Fig. 79.6). Elevation of the buttocks from the table is indicative of rectus femoris tightness. Another sign is inability of the heel to contact the buttocks. The distance from the heel to the buttocks can be measured to assess side-to-side differences.
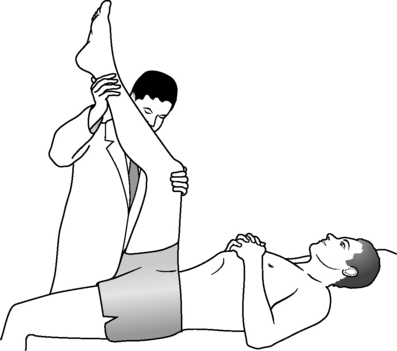
Popliteal angle
The hamstrings are tested via measurement of the popliteal angle or passive straight leg raise. Popliteal angle is measured by having the patient lie supine. The examiner flexes the patient’s hip to 90 degrees. The knee is then extended. Popliteal angle is defined as the line formed by a perpendicular line drawn around the axis of the knee and the knee at end range (Fig. 79.7).
Esola et al.47 found a high correlation between hamstring flexibility and low back pain. They also concluded that improving hamstring flexibility in subjects with a history of low back pain may decrease the stress on the lumbar spine during flexion by allowing a greater hip range of motion.
ASSESSMENT FOR LEG LENGTH DISCREPANCY
Leg length discrepancy can be a cause of low back pain. In assessment of leg length discrepancy, the clinician needs to place the patient’s legs in precisely comparable positions and measure the distance from the anterior superior iliac spines to the medial malleoli of the ankles. In a supine position, the examiner will ask the patient to raise the pelvis off the examining table and place it back on the table with the knees flexed at 90 degrees, with the feet flat on the table. If there is a height discrepancy between the knees, the tibia is longer on the side where the knee lies superiorly. If one knee is more anterior with respect to the other knee, it indicates that the femur of that extremity is longer. If the knees are fully aligned, the next step is for the examiner to fully extend the patient’s knees passively. Leg length discrepancy is assessed by comparing the position of the medial malleoli. For another useful measurement, the examiner can measure distance between the umbilicus and each medial malleolus. Unequal distances signify an apparent leg length discrepancy, usually due to pelvic obliquity or from adduction or flexion deformity in the hip joint. Nadler et al.48 demonstrated no association between leg length discrepancy and the development of low back pain in college athletes.
NEUROLOGICAL EXAMINATION
Motor examination
Classifications of MMT utilize a 6-point scale.49–51 The scale is shown in Table 79.2.
Table 79.2 Classification of manual muscle testing
| 0 = no palpable muscle contraction |
| 1 = palpable or visible contraction |
| 2 = full range of motion with gravity eliminated |
| 3 = full range of motion against gravity |
| 4 = full range of motion against moderate resistance |
| 5 = full range of motion against full resistance |
The examiner needs to have a systematic approach to performing this test. The examination should include the hip flexors (L1–3), quadriceps (L2–4), tibialis anterior (L4–5), extensor hallucis longus (L5), and the gastrocnemius/soleus complex (S1). Hip extensor and hip abductor strength also need to be assessed. Hip extensors are examined by placing the patient prone and asking him or her to extend the lower extremity. The examiner will apply a downward force and the patient is instructed to resist the examiner’s force. Hip abductor strength is tested by having the patient lie on the table on his or her side. The patient is then asked to raise the leg that is upward and resist a downward force by the examiner. Hip abductor weakness can also be detected by the Trendelenburg test. The patient is instructed to stand on one leg; with a weak hip abductor, the patient leans the trunk toward the weak side or the pelvis drops to the contralateral side. Varus deviation of the proximal lower extremity while performing one-legged squats further confirms this finding.
Manual muscle testing is subjective and is reliant on the patient. Factors such as motivation, cooperation, pain, and fatigue strongly affect the outcomes of this test. Also, patient’s age, comprehension skills, and ability to follow commands can affect the usefulness of MMT. Barr et al.52 showed increased variability among older and younger patients. Escolar et al. also showed increased variability in children.53
Due to the subjectivity of manual muscle testing, there may be a need for specialized equipment to quantify the amount of force produced. Quantitative muscle testing produces data demonstrating the amount of force produced. It is composed of isokinetic and isometric muscle testing. Isokinetic muscle testing measures maximum torque and work across a joint throughout the range of motion. Reliability of isokinetic muscle testing has been confirmed in many studies. In 1996, Li et al. determined the reliability of the Cybex 6000 isokinetic dynamometer in knee flexors and extensors using 30 subjects with no previous history significant of knee injuries. They found the dynamometer to be highly reliable with the intra-class correlation coefficient (ICC) ranging 0.82–0.91 for peak torque, 0.76–0.89 for total work, and 0.71–0.88 for average power. The average variability for the three tests was 9–14%.54
Pincivero et al. utilized a Biodex System 2 isokinetic dynamometer to assess test/re-test reliability for concentric quadriceps and hamstring strength. The results showed high ICC values ranging 0.88–0.97 at 60 degrees/second and 0.82–0.96 at 180 degrees/second.55 Emery et al. used a Cybex Norm isokinetic dynamometer to evaluate reliability of eccentric hip flexor and adductor peak torque. Nineteen male volunteers participated in this study. ICC was measured to be >0.84 with eccentric measurement of peak hip adductor torque.56 Callaghan et al. looked at the reliability of isokinetic testing in 20 healthy subjects and 16 patients with patellofemoral pain syndrome. In the healthy population, ICC estimates were >0.75 for isokinetic peak torque and >0.83 for average power and total work. In the patients with patellofemoral syndrome, intra-class correlation coefficient estimates were >0.82 for isokinetic peak torque and >0.75 for average power and total work.57 Isokinetic testing has been proven to be highly reliable in all of the above studies. However, the equipment needed to perform this test is large and expensive.
Many studies comparing MMT with quantitative muscle testing have shown MMT to falsely overestimate a muscle as having full strength, whereas quantitative muscle testing is able to detect subtle differences. Comparing MMT to a handheld dynamometer, Beasley demonstrated that 50% of quadriceps strength needs to be lost before manual muscle testing can identify knee extensor weakness.58 Bohannon, studied knee extension force in 50 patients comparing MMT to a HHD. He found the two tests to be significantly correlated (p=0.001). However, he also found the two test scores to be significantly different (p<0.001). He concluded that MMT may overestimate knee extensor strength.59
Several studies have examined the sensitivity and specificity of muscle strength in patients with lumbar radiculopathy. In 1961, Knutsson showed great toe extensor weakness to have a sensitivity of 76% and a specificity of 52% in patients with an L5 root involvement.60 Spangfort looked at 2504 patients with a confirmed lumbar radiculopathy and found that 70–90% of patients with a weak ankle dorsiflexor had a herniated disc at L4–5 level. Ankle dorsiflexor weakness showed an overall sensitivity of 49% and a specificity of 54%.61 In a study of 1986 patients with lumbar disc herniation, Hakelius et al. demonstrated quadriceps weakness to have a sensitivity of <1% with a specificity of 99%. Reduced ankle dorsiflexor strength had a sensitivity of 49% and a specificity of 54%. Great toe extensor strength was 37% sensitive and 71% specific. Ankle plantar weakness only had a sensitivity of 6% and a specificity of 95%.62,63
Kerr et al. showed ankle dorsiflexion weakness in 54% and ankle plantar flexion weakness in 13% of the patients with L4–S1 disc herniations. The overall specificity was 89%.64 Lauder compared MMT to electrodiagnostic findings in 170 patients with radiculopathy. In this study, 40% of the patients with an L3–4 radiculopathy had weak knee extensors (specificity = 89%). In patients with an L5 radiculopathy, she found toe extensor weakness to be 61% sensitive and 55% specific. In patients with a documented S1 radiculopathy, ankle plantar flexion strength had a sensitivity of 47% with a specificity of 76%.65
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree