Chapter 90 Physeal Fractures About the Knee
Distal Femur
Distal femoral physeal fractures are most common in older children and tend to occur from high-energy trauma.27 Most commonly, these fractures are Salter-Harris II fractures.18 The most common mechanisms of injury are motor vehicle accidents and falls.18 Most commonly, a valgus force leads to medial physeal separation extending into an oblique fracture through the lateral metaphysis.6 Less commonly, a hyperextension injury is responsible, with risk of neurovascular injury.6 The distal femoral physis is at risk for fracture in this scenario because of the fact that the anterior cruciate ligament (ACL), posterior cruciate ligament (PCL), lateral collateral ligament (LCL), and medial collateral ligament (MCL) do not span or protect it.
This fracture is four times more common in boys than in girls.18
Imaging should begin with anteroposterior, lateral, and oblique radiographs. Stress radiographs may provide a definitive diagnosis but risk further physeal damage. If nonstress radiographs are inconclusive, magnetic resonance imaging (MRI) is less painful for the patient and can provide more information.1
Suspicion for popliteal vascular injury should be high, with the incidence of popliteal artery injury reported at 3%.8 Angiography is the gold standard for evaluation of arterial injury in the setting of a fracture about the knee.8 Prompt recognition and intervention for vascular injury in this scenario decreases the risk of catastrophic complications such as loss of limb.
At least 20% of distal femoral physeal fractures lead to angular deformity and growth arrest requiring reconstructive surgery.18 Factors that predict outcome include type of fracture, initial fracture displacement, and exactness of reduction.18 Growth disturbances are usually evident within 6 months to 1 year, but follow-up may be considered until skeletal maturity.28
At times, interposed periosteum may be removed through a relatively small incision with a skin hook. If the Thurston-Holland fragment is large enough, lag screws may be placed for relatively rigid fixation (Figs. 90-1 through 90-4). Thompson and associates demonstrated that 43% of fractures reduced without fixation displaced during cast treatment, whereas no fractures treated with internal fixation displaced.29 Smooth pins can be placed percutaneously to maintain reduction with little risk to the physis. Once the fracture reduction is maintained, the knee can be extended again to assess coronal plane alignment.

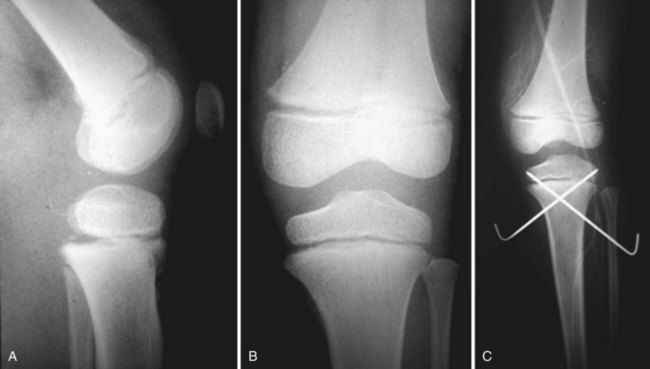
Figure 90-1 Anteroposterior (AP) radiograph of distal femoral physeal fracture.
(Image property of Children’s Orthopedic Center.)

Figure 90-2 Lateral radiograph of distal femoral physeal fracture.
(Image property of Children’s Orthopedic Center.)

Figure 90-3 Anteroposterior (AP) radiograph post closed reduction internal fixation distal femur physeal fracture.
(Image property of Children’s Orthopedic Center.)

Figure 90-4 Lateral radiograph post closed reduction internal fixation distal femoral physeal.
(Image property of Children’s Orthopedic Center.)
Figures 90-1 through 90-4 illustrate a distal femoral Salter-Harris III fracture treated with closed reduction and internal fixation.
Proximal Tibia
Physeal fractures of the proximal tibia are extremely rare. The stabilizing anatomy of the hamstrings, MCL, and LCL protects this region, and high energy is required to disturb the area. Peak incidence of proximal tibia physeal fractures occurs between the ages of 10 and 12 years. Extension is the predominant mechanism of injury for these fractures.21 Salter-Harris type I and II fractures predominate in this age group, and Salter-Harris type III and IV fractures tend to occur at a later age (14 years).21,23 Proximal tibial triplane fractures have also been described, but these occur rarely.26
When injury to the proximal tibia is suspected, imaging consists of anteroposterior and lateral radiographs of the knee. Stress views should be avoided, as they may cause further physeal damage. If radiographs are inconclusive, MRI can be used to further investigate for physeal injury.1
As in fractures of the distal femur and in knee dislocations when there is posterior placement of the tibia, suspicion for injury to the popliteal artery should be high. Angiography is the standard of care in diagnosing popliteal injury, and vascular consultation should be obtained promptly.8 Shelton and Canale reported popliteal artery injuries resulting in vascular insufficiency in 2 of 39 patients.25
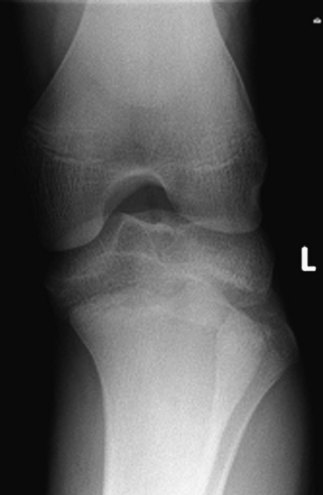
Anatomic reduction of proximal tibial fractures is necessary to protect both the articular surface and the physis. Direct visualization may augment radiographic evaluation of the articular surface and is recommended if there is any doubt about articular congruity. Arthroscopic assistance to assess the reduction is well reported in the adult literature and can be considered for adolescents.5 If a large metaphyseal fragment is present, cannulated screws can be used as fixation. If the physis must be crossed, smooth pins should be used. Because they may need to enter the knee joint itself, early removal of these pins is recommended to prevent infection. Figure 90-5 shows operative fixation of a proximal tibial physeal fracture with K-wires.
Complications of proximal tibial physeal fractures include popliteal artery injury (associated with posterior displacement of the tibial shaft), compartment syndrome, peroneal nerve palsy, growth disturbance, and traumatic arthritis.25 Because of the high energy required to cause this fracture, and the risk of compartment syndrome, inpatient admission for observation should be considered for even minimally displaced proximal tibial physeal fractures. Initially, regaining range of motion can be challenging. Vigilant follow-up to evaluate for growth plate injury in the form of angular deformity or leg length discrepancy should continue for at least a year post surgery. Standing radiographs from hip to ankle should be reviewed at 6 months and 1 year postoperatively.
Tibial Tubercle Fractures
Tibial tubercle fractures occur when the tibial tubercle physis is closing at the age of 11 or 12. These fractures occur much more frequently in boys than in girls.3 They are classified according to the Watson-Jones classification, which was modified by Ogden in 1980 to include “A” and “B” subsets.22 A type I fracture is a small fragment of the tuberosity, which is avulsed and displaced upward. Type IA is an incomplete separation of the fragment from the metaphysis, and type IB is a complete separation. In a type II fracture, the entire lip of the tibial tuberosity is displaced upward. A type IIA fracture has no comminution, and a type IIB fracture has comminution. A type III fracture is one in which the entire tuberosity is fractured at its base, and the fracture line extends superiorly into the proximal tibial intra-articular surface. A type IIIA fracture has a single displaced fragment, and a type IIIB fracture includes comminuted displaced fragments. This classification system was further expanded by Ryu and Debenham24: They added a type IV fracture, which is an avulsion fracture of the proximal tibial epiphysis that extends into the posterior cortex of the tibia.13 This type of flexion avulsion fracture of the proximal tibia is seen most commonly in the prepubescent patient age 13 or older.21 Jumping with eccentric contraction of the quadriceps mechanism is the most common mechanism of injury.
Operative indications for tibial tubercle fracture include displacement or intra-articular extension into the proximal tibia.22 Because these fractures usually occur when the tibial tubercle physis is beginning to close, treatment involves screw fixation across the fracture and physis without concern for growth disturbance in those approaching the end of growth. Type IV tibial tubercle fractures that extend to the posterior aspect of the tibia must also be fixed by securing the tibial tubercle. Although these fractures may appear similar to proximal tibial physeal fractures, they are on a continuum with tibial tubercle fractures (particularly in terms of mechanism and energy of injury) and should be treated as such.
Complications
Compartment syndrome can occur in displaced tibial tubercle fractures as the result of damage to the recurrent branch of the anterior tibial artery. Because this physis is beginning to close, genu recurvatum is actually a rare complication.22 Genu recurvatum may occur, however, in the rare patient below the age of 11 or 12 who sustains a tibial tubercle fracture. Avulsion of the tibialis anterior muscle has been reported in concert with a type III tibial tubercle fracture.14
The case pictured in Figures 90-6 through 90-12 illustrates a type IV tibial tubercle fracture that was treated incorrectly. The proximal tibial physeal fracture was secured with smooth pins, and this portion of the fracture did in fact heal. However, the tibial tubercle component did not heal. The patient thus went on to sustain a tibial tubercle fracture. This was subsequently appropriately treated with open reduction and screw fixation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree