Peroneal Tendon Disorders
Lawrence A. DiDomenico
Michelle C. Anania
A commonly overlooked cause of lateral ankle pain is pathology of the peroneal tendons. Injuries to the peroneal tendons are often misdiagnosed as lateral ankle sprains; therefore, typically, the initial treatment regimen is incorrect. What begins as an acute process that can be treated with conservative modalities progresses to a chronic condition that is highly resistant to conservative care, making surgery oftentimes a necessity. These conditions commonly present as a chronic condition with lateral ankle pain. Disorders of the peroneal tendons can be categorized into one of four groups:
Peroneal tendinitis, tenosynovitis
Peroneal tendon tears or ruptures
Peroneal subluxation and dislocation
Painful os peroneum syndrome (POPS)
Armagon and Shereff (1) explained that these four categories are not completely distinct from one another, but rather, there is a significant amount of overlapping of symptoms and findings. It is representative of a spectrum of conditions. With the increased popularity of sports in all age groups, the advancement of diagnostic modalities, and increased awareness on the part of the physician, peroneal disorders are becoming more commonly diagnosed (2,3).
ANATOMY
The lateral compartment of the leg consists of the peroneus longus and the peroneus brevis muscles. The peroneus longus muscle origin is the lateral tibial condyle and the head of the fibula. The peroneus brevis muscle has its origin at the middle one-third of the fibula and the intermuscular septum. As the tendons course distally, they share a common synovial sheath, which begins approximately 4 cm proximal to the tip of the lateral malleolus. Upon reaching the posterior aspect of the lateral malleolus, the tendons run within a fibro-osseous tunnel known as the retromalleolar or fibular groove. At this level, the peroneus longus tendon sits posterior and lateral to the peroneus brevis tendon, which abuts up against the groove. Heckman et al (4) outlined the boundaries of the fibular groove with the lateral malleolus forming the anterior wall of the fibular groove, the superior peroneal retinaculum located posterolateral, and the posterior talofibular, the calcaneofibular, and the posterior tibiotalar ligaments forming the medial wall. The most important structure in holding the peroneal tendons in place at the level of the distal fibula is the superior peroneal retinaculum. This structure is an extension of the deep fascia and originates on the posterolateral aspect of the distal fibula and inserts as two distinct bands onto the lateral calcaneal wall and the lateral aspect of the Achilles tendon sheath. Its purpose is to prevent lateral migration, subluxation, of the peroneal tendons (4,5).
Coursing distally along the lateral wall of the calcaneus, the common tendon sheath is split into two separate sheaths, a superior and an inferior sheath, by the peroneal tubercle. The superior sheath houses the peroneal brevis tendon, while the peroneal longus is contained within the inferior sheath. From the peroneal tubercle, the peroneus brevis continues distally to insert onto the base of the fifth metatarsal, the styloid process. Hyer et al (6) pointed out that the peroneal tubercle has a cartilaginous facet on its inferior surface and the purpose of the tubercle is to assist in gliding the peroneus longus tendon distally toward the cuboid. Once it reaches the cuboid, the peroneus longus tendon makes a sharp turn within the cuboid groove and heads medially to insert onto the plantar base of the first metatarsal and the medial cuneiform. If an os peroneum is present, it is located within the peroneus longus tendon at the level of the calcaneocuboid joint.
The peroneal muscles receive their innervations from the superficial peroneal nerve. Petersen et al performed a cadaveric study of 40 healthy peroneal tendons, 20 longus tendons, and 20 brevis tendons. These peroneal tendons were injected with an immunohistochemical stain that adheres to laminin, a glycoprotein found in the basement membrane of blood vessels. What they discovered is the peroneal tendons have three areas of avascularity, which correspond with the three areas where most tendinopathy develops. The gross blood supply comes from the posterior peroneal artery and from branches of the medial tarsal artery. These arteries penetrate the posterior aspect of the peroneal tendons. The study showed the majority of each tendon is covered by a vascular-rich peritenon and that the blood supply within each tendon runs proximal to distal following the course of the tendons. Most importantly, they determined that the three zones of avascularity, one in the peroneus brevis and two in the peroneus longus, are due to interruption of these longitudinal arteries. These areas were noted to be devoid of laminin and therefore devoid of arterial vessels (7). These three areas were also noted to correspond to the following regions where the tendons run around a bony pulley:
In the peroneus brevis where it runs against the retromalleolar groove. The length of avascularity averaged 40 mm.
In the peroneus longus as it bends around the lateral malleolus. This area averaged 52 mm.
In the peroneus longus as it turns medially at the cuboid, averaging 25 mm (7)
Various anatomical anomalies as well as associated pathologies have been linked to peroneal disorders. These include a shallow retromalleolar groove, a low-lying peroneal muscle belly, the presence of a peroneus quartus muscle, an enlarged peroneal tubercle, a valgus or cavovarus hindfoot, laxity of the superior peroneal retinaculum, the presence of bone spurs at the posterolateral edge of the fibula, and lateral ankle instability. As a note of caution, Saupe et al (8), in a magnetic resonance imaging (MRI) study of 65 volunteers, revealed that any one of these anatomical variants can be found in asymptomatic ankles.
Therefore, the presence of an anatomical variant does not absolutely lead to peroneal tendon disorders.
Therefore, the presence of an anatomical variant does not absolutely lead to peroneal tendon disorders.
The more narrow or shallow the retromalleolar groove, the more likely instability is present when the peroneal tendons glide along the posterior aspect of the lateral malleolus. The instability leads to an increased risk of subluxation due to the increased stress applied by the tendons on the attachment site of the superior peroneal retinaculum onto the posterolateral lip of the fibula. Studies have shown the shape of the groove can present in one of three ways: convex, flat, or concave. However, both Ferran et al (9) and Heckman et al (4) assert the shape of the groove is dictated by the fibrocartilaginous lip at the posterolateral ridge of the fibula, not by the degree of groove concavity.
Anything that adds bulk within the retromalleolar groove can cause increased pressure during ankle dorsiflexion. This additional pressure leads to stenosing of the peroneal tendons and stretching of the superior peroneal retinaculum (4,5,10). Saupe et al (8) illustrated that a low-lying peroneus brevis muscle belly is one that extends more than 15 mm below the tip of the fibula. A peroneus quartus muscle, an anomalous muscle occurring in 10% to 22% of the population, originates on the peroneus muscle belly and inserts onto the peroneal tubercle. Other muscle variants of note are the peroneal digiti quinti and the peroneocalcaneal muscles. Because of its insertion, the peroneus quartus has been linked to hypertrophy of the peroneal tubercle.
When the peroneal tubercle is hypertrophied, determined by Saupe et al to be higher than 5 mm, the increase in mechanical irritation leads to the development of stenosis and a decrease in the gliding of the tendon within its sheath. This variant is commonly linked to tears within the peroneus longus tendon because of its position inferior to the tubercle (8). A study performed by Hyer et al (6) found that 90% of their specimens had a peroneal tubercle, of which 28% were considered enlarged. Taki et al described a case of a young boy with bilaterally enlarged peroneal tubercles. Upon successful removal, the histologic results proved to be a bilateral osteochondroma (11).
When the hindfoot has a valgus deformity, crowding of the peroneal tendons take place in the retromalleolar area and the area just distal to the fibula (12). A cavovarus hindfoot causes an increase in friction in the areas of the lateral malleolus, the peroneal tubercle, and the cuboid groove leading to tenosynovitis (4). In patients with a neurologic deficit, peroneal weakness leads to an increase in the pulling force from the posterior tibial tendon. This sets the stage for instability of the lateral ankle (13).
Lateral ankle instability refers to the loss of proprioception and function within the lateral soft tissue structures of the ankle, that is, the lateral collateral ligaments, the superior peroneal retinaculum, and the peroneal tendons. These patients are prone to repeated inversion ankle sprains, predisposing oneself to peroneal tendon injuries. When there is failure of the lateral ankle ligaments, the peroneal tendons function to keep the ankle stabilized, placing an increase in strain on the tendons (1,13,14). One study by Squires et al (13) proved various disorders of the peroneal tendons frequently occur in cases of chronic lateral ankle instability: peroneal tenosynovitis, failure of the superior peroneal retinaculum, and tearing of the peroneal brevis tendon (Fig. 77.1). A cadaveric study by DiGiovanni et al analyzed the amount of strain placed on the superior peroneal retinaculum when failure of one or more of the lateral collateral ligaments occurred. When the anterior talofibular ligament was severed, no changes in stress were noted. A 25% increase in the amount of stress across the retinaculum was recorded when both the calcaneofibular and the anterior talofibular ligaments were severed. When all three collateral ligaments were cut, stress within the superior peroneal retinaculum increased by 64%. This proves that as the degree of instability increases, so does the amount of strain placed on the superior peroneal retinaculum (1,15).
BIOMECHANICS
The peroneus longus and brevis muscles work as strong everters of the foot and weak plantarflexors of the ankle. More specifically, Root et al illustrated the functions of the peroneus longus muscle as being (a) a stabilizer of the first ray during midstance and propulsion; (b) a weak plantarflexor of the ankle joint during propulsion; (c) a strong everter of the foot during the early phase of propulsion; and (d) a weak decelerator of ankle joint dorsiflexion during the heel lift period of the propulsive phase of gait. The functions of the peroneal brevis muscle are specifically described as (a) a strong everter of the foot during midstance and propulsion; (b) a stabilizer of the fifth metatarsal
during midstance and early propulsion; (c) an antagonist to those muscles that supinate the subtalar and midtarsal joints; and (d) an antagonist to the lower leg muscles that supinate the foot at the subtalar joint, that is, a weak plantarflexor of the ankle (16). As antagonists to the posterior tibial, flexor hallucis longus, flexor digitorum longus, and anterior tibial muscles, both peroneal tendons function as dynamic stabilizers of the lateral collateral ankle ligaments during excessive inversion and, along with these ligaments, are important in ankle proprioception (1,4,13).
during midstance and early propulsion; (c) an antagonist to those muscles that supinate the subtalar and midtarsal joints; and (d) an antagonist to the lower leg muscles that supinate the foot at the subtalar joint, that is, a weak plantarflexor of the ankle (16). As antagonists to the posterior tibial, flexor hallucis longus, flexor digitorum longus, and anterior tibial muscles, both peroneal tendons function as dynamic stabilizers of the lateral collateral ankle ligaments during excessive inversion and, along with these ligaments, are important in ankle proprioception (1,4,13).
EPIDEMIOLOGY
Overall, disorders of the peroneal tendons are uncommon. They are frequently seen in those sports in which the foot and ankle perform a lot of cutting motions, snow skiing being the most common. Because they are often mistaken as lateral ankle sprains, peroneal disorders tend to go untreated. When this occurs, the delay in diagnosis and treatment leads to instability of the lateral ankle. If a patient has signs and symptoms of ankle instability, it is important to examine the peroneal tendons thoroughly because the instability may be stemming from peroneal tendinopathy. Systemic conditions have also been associated with disorders of the peroneal tendons. These include various forms of arthritis such as rheumatoid and psoriatic, tophaceous gout, hyperparathyroidism, diabetic neuropathy, the use of fluoroquinolone antibiotics, generalized ligamentous laxity, and local steroid injection (5,12,17). The buildup of gouty crystals leads to weakening of extracapsular tissue including tendons (17). Lagoutaris et al described a case in which chronic tophaceous gout infiltrated both the peroneus longus and the peroneus brevis tendons, causing a longitudinal split tear in both tendons. Chronic inflammation within the tendons can accompany the synovitis of tophaceous gout, and as the gout progresses untreated, eventual rupture of the tendons can occur (17).
Peroneal tendinitis and peroneal tenosynovitis occur secondary to repetitive or prolonged movements. To avoid confusion, inflammation located at the musculotendinous junction is termed peritendinitis, which is due to prolonged repetitive movements and presents as pain with motion of the tendon. Tenosynovitis is inflammation of the tendon sheath, which involves edema. Stenosing tenosynovitis is a result of chronic tenosynovitis and is a painful inflammatory condition in which the tendon sheath narrows and adheres to the tendon. Of all the tendons that run in the ankle region, the peroneal tendons are most commonly affected (18). Once stenosing tenosynovitis develops, there is less chance that conservative treatment will be successful. Heckman et al (4) revealed that 77% of patients with chronic lateral ankle instability have some form of peroneal tendon or peroneal tendon sheath inflammation.
Peroneal tendon tears and ruptures are most often due to an inversion ankle injury and are more common in the peroneus brevis tendon than the peroneus longus tendon (Fig. 77.2). Tears involving these tendons can also be associated with other disorders; therefore, if a tear in either peroneal tendon is diagnosed, it is important to examine for chronic tenosynovitis; fractures of the ankle, calcaneus, and talus; and chronic ankle instability (Fig. 77.3).
Although the occurrence is rare, the frequency of subluxation and dislocation of the peroneal tendons is on the rise with the increased popularity in sports. When the ankle joint is suddenly forced into dorsiflexion, the peroneal tendons respond by undergoing severe contraction. This forced movement puts a lot of stress on the superior peroneal retinaculum to the point at which it becomes laxed or ruptures. With failure of the soft
tissue restraint, the peroneal tendons are now able to anteriorly sublux out of the retromalleolar groove (Fig. 77.4) (10,19). This forced dorsiflexion resulting in peroneal subluxation is most commonly seen in skiing accidents but has also been tied to soccer, dancing, basketball, rugby, running, cycling, rowing, football, baseball, ice skating, gymnastics, and horseback riding (3,9,10,18,19 and 20). Peroneal subluxation has also occurred with the foot being in a plantarflexed, inverted, everted, or externally rotated position. These movements are thought to cause tightening of the calcaneofibular ligament. This tightening pushes against the superior peroneal retinaculum and brings about an increase in the amount of pressure against the retinaculum. The results are failure of the superior peroneal retinaculum and dislocation of the tendons (10,19). Trauma is the most likely cause of peroneal subluxation, occurring in 92% of the cases, while the other 8% is congenital in origin due to some type of deficit within the bone or soft tissue structures that act to prevent the peroneal tendons from subluxing (19,21). Rosenfeld et al revealed that congenital peroneal subluxation occurs in approximately 3% of newborns with over 90% resolving without any treatment necessary (19). Ogawa et al added that any congenital deformity of the bone and soft tissue of the leg can increase the risk of peroneal subluxation. These include hyperelasticity of the ligaments, congenital absence of the superior peroneal retinaculum, an anomaly of the peroneus brevis muscle, a shallow fibular groove causing bilateral congenital subluxation, congenital vertical talus, and talipes planovalgus (10). In adults, nontraumatic peroneal subluxation is most likely secondary to laxity of the superior peroneal retinaculum, a shallow fibular groove, or a distal fibula with a convex surface (19). The occurrence of peroneal subluxation along with ankle sprains is less than 0.5%. Lateral ankle instability, longitudinal split tears of the peroneus brevis tendon, attenuation of the superior peroneal retinaculum, insufficient depth of the fibular groove, and fractures of the hindfoot have also been associated with peroneal tendon subluxation. Klein et al (22) discovered that 46% of patients who suffered from a Hawkins type II lateral talar process fracture also had subluxation of the peroneal tendons.
tissue restraint, the peroneal tendons are now able to anteriorly sublux out of the retromalleolar groove (Fig. 77.4) (10,19). This forced dorsiflexion resulting in peroneal subluxation is most commonly seen in skiing accidents but has also been tied to soccer, dancing, basketball, rugby, running, cycling, rowing, football, baseball, ice skating, gymnastics, and horseback riding (3,9,10,18,19 and 20). Peroneal subluxation has also occurred with the foot being in a plantarflexed, inverted, everted, or externally rotated position. These movements are thought to cause tightening of the calcaneofibular ligament. This tightening pushes against the superior peroneal retinaculum and brings about an increase in the amount of pressure against the retinaculum. The results are failure of the superior peroneal retinaculum and dislocation of the tendons (10,19). Trauma is the most likely cause of peroneal subluxation, occurring in 92% of the cases, while the other 8% is congenital in origin due to some type of deficit within the bone or soft tissue structures that act to prevent the peroneal tendons from subluxing (19,21). Rosenfeld et al revealed that congenital peroneal subluxation occurs in approximately 3% of newborns with over 90% resolving without any treatment necessary (19). Ogawa et al added that any congenital deformity of the bone and soft tissue of the leg can increase the risk of peroneal subluxation. These include hyperelasticity of the ligaments, congenital absence of the superior peroneal retinaculum, an anomaly of the peroneus brevis muscle, a shallow fibular groove causing bilateral congenital subluxation, congenital vertical talus, and talipes planovalgus (10). In adults, nontraumatic peroneal subluxation is most likely secondary to laxity of the superior peroneal retinaculum, a shallow fibular groove, or a distal fibula with a convex surface (19). The occurrence of peroneal subluxation along with ankle sprains is less than 0.5%. Lateral ankle instability, longitudinal split tears of the peroneus brevis tendon, attenuation of the superior peroneal retinaculum, insufficient depth of the fibular groove, and fractures of the hindfoot have also been associated with peroneal tendon subluxation. Klein et al (22) discovered that 46% of patients who suffered from a Hawkins type II lateral talar process fracture also had subluxation of the peroneal tendons.
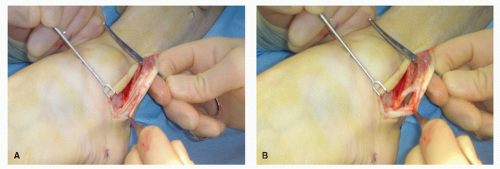
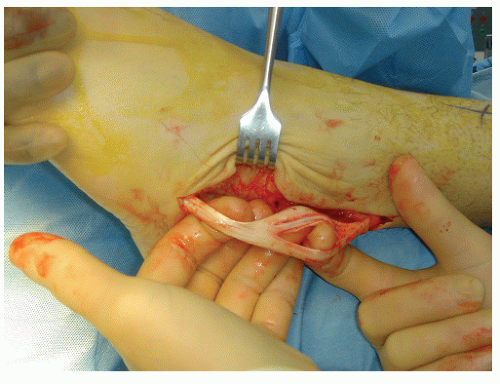 Figure 77.2 A peroneal brevis tendon with two different longitudinal tears in the retromalleolar region secondary to chronic lateral ankle instability. |
PHYSICAL EXAMINATION
Patients with peroneal tendon disorders relate a history of an ankle sprain that never resolved. Because they are frequently overlooked and therefore misdiagnosed, peroneal disorders are not usually picked up until several weeks to several months after the initial injury (Fig. 77.5). A study performed by DiGiovanni et al determined the type and the rate of occurrence of injuries that occur concomitantly with lateral ankle instability. Out of a total of 61 patients, 77% had peroneal tendinitis, 54% had laxity of the superior peroneal retinaculum, and 25% had a tear of the peroneus brevis tendon. The results of this study emphasize the importance of needing a high index of suspicion for associated injuries when treating chronic lateral instability of the ankle (15). This will bring about a more prompt and accurate treatment plan for the patient (4,9,13,15,18,21,23,24). As a general rule, the presence of decreased peroneal muscle strength is not a reliable finding because in many cases the strength can be normal on physical exam (4,5,20). A more reliable exam to determine the possibility of peroneal disorders is to apply stress to the lateral ankle. If there is a problem with the tendons, pain will be elicited with passive inversion of the hindfoot and plantarflexion of the ankle and with active resisted hindfoot eversion and ankle dorsiflexion. Further, Heckman et al (4) and Selmani et al (5) both suggested performing the Coleman Block test to evaluate the alignment of the hindfoot.
PERONEAL TENDINITIS AND TENOSYNOVITIS
The hallmark sign of acute peroneal inflammation is swelling with pain and warmth along the course of the tendons. These findings are not as reliable however in cases of chronic tendinitis. Even though acute trauma can cause tendinitis, the primary cause of inflammation is a repetitive motion that leads to an overuse injury (Fig. 77.6). Tendinitis can present in one of three ways: (a) acute, occurring for less than 2 weeks in which pain presents at the posterior or distal aspect of the lateral malleolus; (b) subacute, symptoms have been present between 2 and 6 weeks; and
(c) chronic, occurring for more than 6 weeks. The chronic situation presents as an insidious onset over weeks to months of pain at the posterolateral aspect of the ankle. To distinguish between the two tendons, peroneal brevis tendinitis can present as pain along the course of the tendon itself or at the site where it inserts onto the base of the fifth metatarsal. Pain associated with tendinitis of the peroneus longus usually presents itself over the lateral aspect of the calcaneus and distally toward the cuboid groove (4).
(c) chronic, occurring for more than 6 weeks. The chronic situation presents as an insidious onset over weeks to months of pain at the posterolateral aspect of the ankle. To distinguish between the two tendons, peroneal brevis tendinitis can present as pain along the course of the tendon itself or at the site where it inserts onto the base of the fifth metatarsal. Pain associated with tendinitis of the peroneus longus usually presents itself over the lateral aspect of the calcaneus and distally toward the cuboid groove (4).
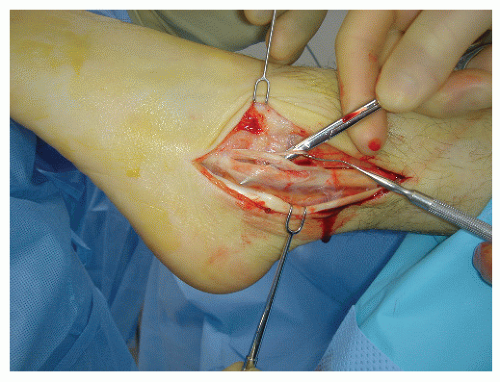
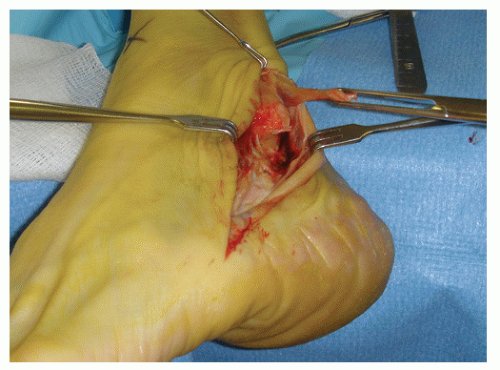 Figure 77.5 A complete tear of the peroneal brevis tendon. This patient also experienced a complete tear of the anterior talofibular ligament. |
PERONEAL TENDON TEARS
Signs and symptoms of a peroneal tendon tear are retromalleolar pain and edema along the tendon’s course. Caution must be used during the physical exam because these findings may be more pronounced in young adults and completely absent in the elderly population. Tears can be acute or chronic in nature and may or may not present with a history of ankle instability with recurrent ankle sprains (4). Muscle strength and range of motion may not be affected because if the tendon is only partially torn, the remaining portion of the tendon, if normal, can compensate; hence a false-negative finding. Specifically, the eversion muscle strength can be picked up by the extensor hallucis longus, the extensor digitorum longus, and the peroneus tertius muscles (4,5,12,13). If the physician palpates too far distal on the lateral malleolus, injuries to the calcaneofibular ligament can be mistaken for injuries to the peroneal tendons (20). Palpable localized soft tissue nodules may be present at the site of tendon disruption. This develops from degeneration that takes place within the tendon after an injury.
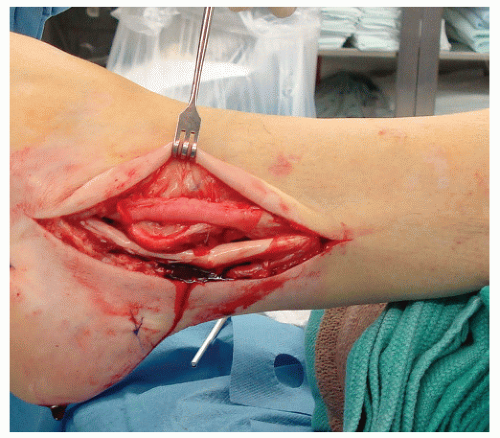
The most common type of tear is the longitudinal split tear that occurs within the peroneus brevis tendon as it runs in the retromalleolar groove (Fig. 77.7). A second type of tear, known as a bucket-handle tear, occurs when the peroneus longus tendon squeezes itself between the two portions of the split in the brevis tendon (13). Tearing of the peroneus brevis tendon can also occur at its insertion site on the base of the fifth metatarsal. This presentation is most often due to an inversion injury. If a patient has a history of arthritis, it is important to take note of any spur formation located at the insertion site of the superior peroneal retinaculum onto the fibula. If the retinaculum is laxed, the peroneus brevis tendon runs over this area when it subluxes, eventually leading to a split tear. Stenosing tenosynovitis of the peroneus brevis is also a risk if there is any erosion of the fibrocartilage on the groove’s surface.
Peroneus longus tendon tears will have pain with palpation at the cuboid or near its plantar insertion onto the base of the first metatarsal and medial cuneiform (Fig. 77.8). The latter presentation can be easily misdiagnosed as posterior tibial tendinitis because of the symptoms occurring medially. Loss or limitation of plantarflexion of the first ray points to disruption of the peroneus longus tendon. Finally, tears within the peroneus longus tendon may be associated with the presence of an os peroneum, an accessory ossicle occurring in 20% of the population (12). These patients will have pain located in the plantar lateral aspect of the foot.
Several easy examination methods can be performed when testing for a tear of the peroneal tendon. The peroneal tunnel compression test can be used in cases of suspected peroneal brevis tendon tears as well as for brevis tendinitis. This involves applying pressure to the peroneal brevis tendon in the retromalleolar groove while the knees are bent at 90 degrees and the foot is in relaxed plantarflexion. A positive exam is the presence of pain (4,5). Other methods described by Squires et al consisted of having the patient get into a runner’s stretch with the affected foot posterior. A tear in the peroneal tendon will cause pain since this type of stretch passively puts the ankle into extreme dorsiflexion. The examiner can also test for tearing by having the patient perform a single-heel- or a double-heel-rise test. This specifically tests for balance and hindfoot stability and will be difficult to do in the presence of a tendon tear. Lastly, patients should be tested for the presence or absence of proprioception by having them stand on one foot with their eyes closed. The patient’s inability to perform this test is a positive result (13).
PERONEAL SUBLUXATION
Subluxation of the peroneal tendons results from failure of the superior peroneal retinaculum to act as a restraint. The mechanism of injury involves a combination of an injury to the ankle
while it is inverted and dorsiflexed and forceful contraction of the peroneal tendons. This puts an unusual amount of strain on the superior peroneal retinaculum, causing it to become stretched or torn (5). Acute cases of subluxation will present with a significant amount of swelling. Pain, tenderness, and ecchymosis will be found posterior to the lateral malleolus just proximal to the distal tip (4,12).
while it is inverted and dorsiflexed and forceful contraction of the peroneal tendons. This puts an unusual amount of strain on the superior peroneal retinaculum, causing it to become stretched or torn (5). Acute cases of subluxation will present with a significant amount of swelling. Pain, tenderness, and ecchymosis will be found posterior to the lateral malleolus just proximal to the distal tip (4,12).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree