Periprosthetic Fractures: Evaluation and Management
Guy D. Paiement
INTRODUCTION
Periprosthetic fractures are increasing in frequency as the numbers of patients with hip and knee arthritis undergo total joint arthroplasty and life expectancy continues to rise. Epidemiological studies have shown that the joint replacement population is growing faster than both the general and the geriatric populations. This population is older, more osteoporotic, and less conditioned, takes multiple medications, and tends to have a higher body mass index (knee replacement population). They are less at risk for higher energy trauma because of their life style but more likely to sustain fractures from lower energy mechanical falls. Several risk factors have been associated with periprosthetic fractures in the elderly; they include osteoporosis, female gender, advanced age, osteopenia, inflammatory arthritis, metabolic bone disease, and alignment deformities (1). Recently, there has been renewed interest in the mechanical and biological characteristics of the joint implants, which may be possible risk factors (2).
The 1-year mortality following a periprosthetic femur fracture is approximately 11% compared to an acute hip fracture mortality of 16.5%. By way of comparison, the mortality rate for primary hip replacement at 1 year is only 2.9% (3). The majority of periprosthetic fracture patients are elderly frail individuals with significant medical comorbidities, and they behave clinically more like hip fracture patients than elective joint replacement patients. While the need for medical optimization is similar in both groups, surgical planning can be more complicated and difficult in the periprosthetic fracture group.
CLASSIFICATION
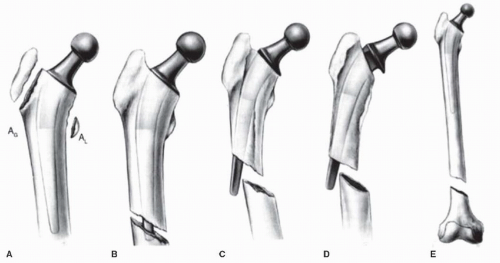
The most widely used classification for periprosthetic femoral fractures around the hip is the Vancouver classification, which is based on three parameters: implant stability, bone stock quality, and fracture location. It divides the femur in three regions: trochanter region (type A), proximal femur down to the tip on the implant (type B), and diaphysis distal to the tip of the implant (type C) (Fig. 45.1). Type A fractures are subdivided into type AG for greater trochanter fractures and type AL fractures that involve the lesser trochanter. Type B fractures comprise a large majority of proximal periprosthetic femur fractures and are divided into three subtypes. In subtype B1, the implant is stable whereas in B2 fractures, the stem is unstable, and in B3 fractures, the implant is unstable and the bone stock is poor (Fig. 45.1B-D). Type C fractures are distal to the tip of a well-fixed stem that complicates the fixation of the fracture (4).
INDICATIONS AND CONTRAINDICATIONS
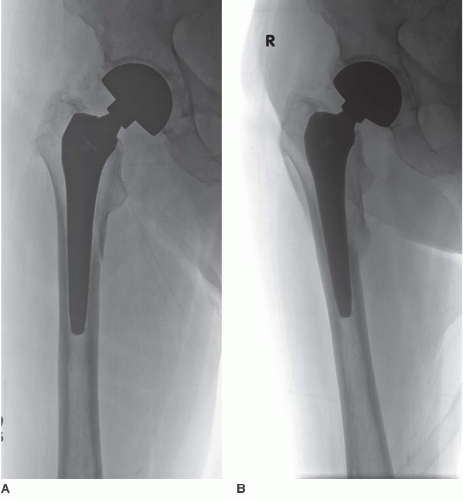
Surgical indication is based on the effect of the fracture on the structural integrity of the bone-prosthesis construct. An undisplaced or minimally displaced greater or lesser trochanter fracture (Vancouver type A) can be
treated nonoperatively because it does not affect prosthesis stability (Fig. 45.2). Caution is required if the stem is cemented because minimally displaced trochanteric fractures may have caused a cement mantle fracture that is not always obvious. Oblique proximal femur or rotational stress radiographs may be indicated in these cases to rule out cement mantle fractures that would require revision of the femoral stem.
treated nonoperatively because it does not affect prosthesis stability (Fig. 45.2). Caution is required if the stem is cemented because minimally displaced trochanteric fractures may have caused a cement mantle fracture that is not always obvious. Oblique proximal femur or rotational stress radiographs may be indicated in these cases to rule out cement mantle fractures that would require revision of the femoral stem.
Femoral condyle fractures in knee replacement patients should be evaluated in the same fashion. An apparently undisplaced medial condyle fracture on standard anteroposterior (AP) and lateral radiograph may be rotated and will heal in a malposition that may change the joint line position or the flexion/extension gap. This can change the prosthesis dynamics and accelerate polyethylene wear. Oblique and varus/valgus stress radiographs can be helpful in making such a determination.
Unstable fractures require surgical treatment. On occasion in a very frail patient where the femoral stem has subsided in a relatively stable position or the acetabular component has migrated medially because of the fracture, nonoperative treatment may be indicated. Small degrees of limb shortening may be preferable to major revision surgery.
PREOPERATIVE PLANNING
History and Physical Examination
Less than 10% of periprosthetic fractures occur following high-energy trauma, and the vast majority occurs after a ground-level mechanical fall. A detailed history of the patient’s preinjury level of function as well as any symptoms related to their joint replacement is essential to determine whether the prosthesis was loose or infected prior to their fracture. Knowledge of the patient’s preinjury ambulatory status and the use of walking aids are helpful. The patient should be questioned about preinjury discomfort or pain with activities of daily living as it may indicate a loose prosthesis. Time, course, and progression of the pain are also helpful clues. Some patients may report progressive instability that suggests implant loosening or bearing surface wear. Whenever possible, prefracture radiographs should be reviewed to detect any changes in component position and axial alignment.
Past medical history, a thorough review of systems, and an accurate inventory of the patient’s current medications are important, because many will require internal medicine consultation preoperatively. Antiplatelet medication, vitamin K antagonists, and immunosuppressive agents are common in this patient population and may impact or delay the surgery. On physical examination, the leg is swollen, tender to palpation, and range of motion is decreased or impossible to evaluate secondary to pain. The skin should be inspected for ulcers, abrasions, lacerations, and ecchymosis particularly around the knee where soft tissues can be problematic. The neurological and vascular status of the limb must be thoroughly evaluated and documented.
Imaging Studies
Full-length AP and lateral radiographs of the femur should be obtained as well as an AP pelvis. Radiographs of the contralateral femur or knee can be useful when the fracture is comminuted making restoration of leg length or alignment difficult. If the fracture involves the acetabulum, Judet views (obturator and iliac oblique views) are required. A CT scan or even a CT-scan angiogram may be needed for some patients with protusio acetabuli to minimize the risk of intraoperative injury to iliac or femoral vessels or to the ureter. A CT scan of the distal femur may be helpful when there is a comminuted, osteoporotic fracture around the knee, because a hinged knee or distal femoral replacement may be necessary. MRI, ultrasound, and nuclear scans are rarely needed in evaluating periprosthetic fractures.
Laboratory Studies
A history of slow wound healing or drainage at the time of the original joint arthroplasty always raises the possibility of a low-grade infection even years later. Biological markers such as ESR (erythrocyte sedimentation rate) and CRP (C-reactive protein) are less reliable in the context of an acute fracture. A recent study of 204 periprosthetic fractures reported a false positive rate for infection of 43% based on the CRP levels and 31% for the ESR (5). If an occult infection is suspected, an image-guided aspiration is recommended to obtain fluid for a gram stain and cultures. Surgery should be delayed if possible until the cultures results are available. A positive culture drastically changes the surgical treatment and the overall prognosis.
Timing of Surgery
Most periprosthetic fractures are caused by low-energy trauma and are rarely open or complicated by neurovascular injury or a dislocation. The preoperative evaluation can be time consuming because of the need to identify the prosthesis, obtain preinjury radiographs, or rule out an infection. The logistics of obtaining the appropriate implants to cover all possibilities may also take time. Few surgeons are equally skilled at repairing difficult fractures and performing complex prosthetic revisions. Collaboration with skilled arthroplasty colleagues may be wise. It may be in the patient’s best interest to postpone surgery until the preoperative evaluation is complete, all necessary equipment is available, skilled operating personnel are on duty and experienced colleagues ready to help.
Surgical Tactics
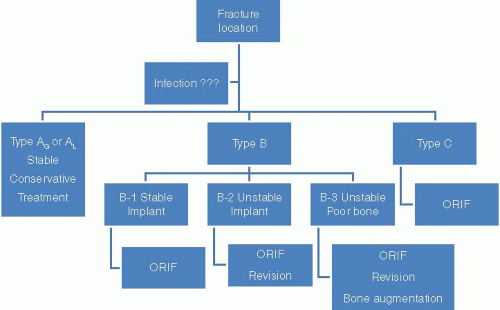
Successful surgery requires a medically optimized patient, a knowledgeable and experienced surgical team, and appropriate equipment and implants. Preoperative planning is crucial, and radiographs should be analyzed with particular attention focused on the fracture location, implant stability, and bone quality. Periprosthetic proximal femur fractures are traditionally classified according to the Vancouver classification since this has been shown to correlate with treatment and outcomes. A simple treatment algorithm for these complex fractures is seen in Figure 45.3.
Although a type B1 fracture (stable stem) is the most common fracture pattern, it is not always easy to distinguish it from a type B2 fracture (loose femoral component). Using the patient’s history, prefracture radiographs of the limb and current x-rays, the stability of the implant is estimated. For Vancouver type C fractures treated with plate osteosynthesis, the plate must extend proximal to the tip of the prosthesis to avoid leaving an area of unprotected bone between the proximal end the plate and the tip of the prosthesis. Failure to “overlap” the plate and the femoral stem leaves an area of high stress concentration between the plate/bone distally and stem/bone proximally. A fracture through such area can occur and is exceedingly difficult to treat. Table 45.1 lists 11 important considerations to address in the course of evaluating and treating these complex fractures. Addressing each of the 11 considerations will improve the chance for a successful outcome. Table 45.2 lists the implants that should be immediately available by likelihood of need for each type of fractures.
SURGERY
Monitoring
Periprosthetic fracture surgery can lead to substantial blood loss in many patients, and since the extent of the surgery cannot be accurately predicted in advance, it is important to prepare preoperatively. Adequate
intraoperative monitoring is very important, and adequate blood replacement must be available. In these elderly frail patients, a Foley catheter, arterial line, and central venous catheters are routinely employed. The use of a “cell saver” is strongly recommended.
intraoperative monitoring is very important, and adequate blood replacement must be available. In these elderly frail patients, a Foley catheter, arterial line, and central venous catheters are routinely employed. The use of a “cell saver” is strongly recommended.
TABLE 45.1 Considerations in Managing Type B Periprosthetic Fractures | |
|---|---|
|
Positioning
Implant stability is the major determining factor in deciding patient position. Fracture fixation alone in the presence of a loose implant invariably leads to a poor outcome. Fluoroscopic examination under anesthesia with the patient supine on a radiolucent table may confirm the presence of a loose implant. If all clinical and radiographic testing point toward a well-fixed implant without infection, the patient should be positioned supine on a flat-top radiolucent table. The supine position facilitates fracture reduction as well as assessment of leg length and alignment. Radiolucent sterile triangles are also useful to maintain reduction and alignment.
A fracture table is rarely needed; a femoral distractor or an external fixator can be helpful if there is substantial shortening of the fracture, or skilled assistance unavailable. If there is any doubt about the stability of a hip implant, the patient should be positioned in the lateral decubitus position. This allows femoral fracture fixation, as well as assessment of the femoral or acetabular component stability, and facilitates revision at the same time if necessary. We routinely use a patient positioning device (peg board) to ensure a stable patient position
throughout the procedure. Furthermore, the table should rotate (backward or forward) in order to obtain a true AP radiograph of the pelvis and obturator/iliac oblique views if needed.
throughout the procedure. Furthermore, the table should rotate (backward or forward) in order to obtain a true AP radiograph of the pelvis and obturator/iliac oblique views if needed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree