Periacetabular Metastases
Peter F. M. Choong
Metastatic carcinoma is the commonest malignancy of bone and characterizes the behavior of 50% of carcinomas. Carcinomas of the prostate, breast, and lung account for over 80% of lesions with renal and thyroid metastases being less frequent. The most destructive lesions are lytic with carcinoma cells permeating the bone and activating lytic proteases and instigating osteoclastic bone resorption. Lung and renal carcinomas typically invoke osteolysis and a permeative behavior. Sclerotic lesions, in contrast, are dominated by regions of bone formation rather than resorption. The stereotypic carcinoma that incites sclerosis with its metastases is prostate carcinoma. Breast carcinoma is characterized by a mixed sclerotic-lytic picture. Regardless of whether the picture is one of lysis or sclerosis, the quality of bone is poor with disorganized formation interspersed between sheets of neoplastic cells. Pain, pathologic fracture, marrow disturbance, and hypercalcemia are the commonest consequences of metastatic bone disease.
The pelvis is a common site of metastatic disease and frequently the entire area can be involved. Destruction of the periacetabulum has far-reaching implications because of its central role in connecting limb mobility and weight bearing. The periacetabular bone transmits the weight of the torso to the legs and the legs in turn transmit the power of mobility to the body through the hip joint. As such, there is a concentration of forces at the hip joint, which makes it vulnerable to failure in the presence of tumor-induced weakening of bone. Failure of function manifests as a loss of weight-bearing capacity, pain, or both.
In the majority of cases, metastatic pelvic disease is treated with a combination of chemotherapy, radiotherapy, hormonal therapy, bisphosphonate therapy, and regimes of analgesia. These combinations of treatment are effective in reducing pain, preventing fracture, preserving function, and improving the quality of life of most patients with pelvic disease. Until recently, the progressive nature of metastatic disease and the lack of surgical experience with periacetabular reconstruction have deterred many from exploiting operative approaches to managing aggressive periacetabular disease that have had a profoundly detrimental effect on patient mobility and independence. Consequently, many patients with potentially surgically treatable disease have had to endure a painful and infirm end to their lives.
GOALS OF SURGERY
The goals of surgical management of periacetabular metastases are to achieve pain control, maintain hip function and mobility, and permit weight-bearing ability. Achieving these goals will have an enormous impact on the patients’ quality of life. To this end, surgery will be directed toward the safe removal of tumor, filling and structurally bypassing the defect, and creating a durable and dependable joint reconstruction. The decision to operate is predicated on the knowledge of the local and systemic extent of the disease, the patient’s health status and longevity, and the probability of the reconstruction improving the patients’ pain, function, and mobility.
INDICATIONS
Periacetabular reconstruction for metastatic disease is indicated in the following situations.
When patients have failed conservative nonsurgical treatment including a non-weight-bearing period, radiotherapy, chemotherapy, and potent pain control programs.
Reconstruction is also indicated when periacetabular destruction presents at an advanced stage when it is clear that nonsurgical treatment is unlikely to improve pain and function.
Periacetabular surgery is also indicated when other surgery for femoral disease, such as impending or completed fracture, is indicated in the presence of periacetabular disease.
Patients who are expected to survive with disease for longer than 3 months should be considered for periacetabular reconstruction.
CONTRAINDICATIONS
The pain and recovery from periacetabular reconstruction and the potential risks of the procedure need to be carefully considered in patients with <2 months survival chance. The justification for surgery in this group may be questionable.
This procedure may also be contraindicated in patients who have significant visceral disease and who may not tolerate the stress of prolonged surgery or blood loss. In this regard, patients with significant pulmonary disease may be particularly vulnerable to a condition known as pulmonary embolic phenomenon which manifests itself as acute cardiovascular and pulmonary collapse at the time of femoral preparation, cementation, or prosthesis insertion.
Surgery is also contraindicated when metastatic disease is so extensive as to provide no bony foundation for the attachment of the reconstruction.
PREOPERATIVE PREPARATION
Preoperative preparation is critical for the safe and successful management of patients with metastatic disease. This includes imaging to assess the local and systemic extent of disease, biopsy to confirm the nature of the bone lesion if this is not known, blood tests to assess the general health status of the patient, and other special tests as required. It is recommended that patients are also reviewed by the anesthetic and internal medicine teams to reverse, stabilize, or optimize any comorbidity that may have a negative impact on the patient’s intraand postoperative course.
Plain Radiographs
Plain radiographs of the whole pelvis should be obtained (Fig. 6.1). This would allow an assessment of not only the extent of periacetabular disease from which surgical planning may be undertaken but also involvement of any other part of the pelvis, which may be relevant. There are a number of classifications of acetabular disease based on plain radiographs. More complex reconstructions are required with increasing degrees of destruction. Plain radiographs should also be taken of the full length of the femur to identify the location of any femoral lesions. This is important to avoid the mistake of implanting a femoral prosthesis above the level of the femoral metastasis, which would create an increase in stress that may lead to periprosthetic fracture.
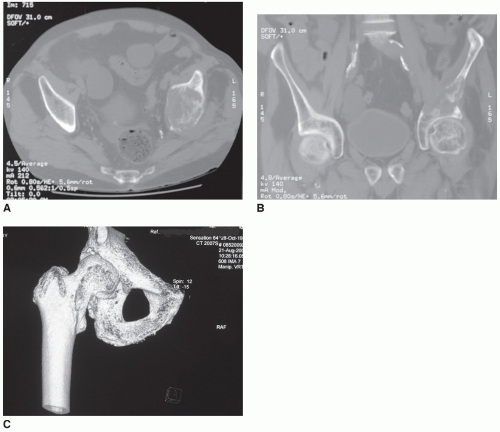
Computed Tomography
Computed tomography (CT) is an excellent modality for assessing cortical and trabecular destruction. This imaging technique is useful for more accurate delineation of periacetabular disease (Fig. 6.2A,B) than plain radiographs. Later-generation software are able to produce excellent three-dimensional reconstructions which can be rotated and manipulated, providing surgeons with different perspectives of the pelvis, which may help to guide their choice of reconstruction (Fig. 6.2C).
CT of the chest, abdomen, and pelvis is a fast and reliable means of determining the extent of visceral spread. This is particularly important for alerting treating teams of the potential for intraoperative pulmonary complications.
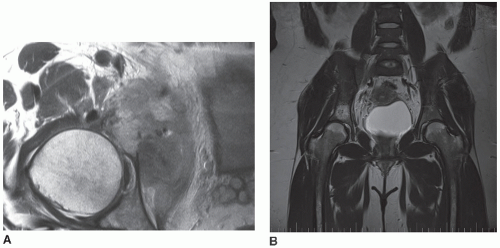
Magnetic Resonance Imaging
Magnetic resonance imaging (MRI) provides unsurpassed soft tissue contrast for clearly delineating any soft tissue extension of the periacetabular tumor (Fig. 6.3A). Further, the marrow extent of disease (Fig. 6.3B) is very clearly seen on magnetic resonance scans and this is important when planning which parts of the pelvis
may be relied upon as stable foundations for transfixing Steinmann pins that are inserted for supporting the acetabular component.
may be relied upon as stable foundations for transfixing Steinmann pins that are inserted for supporting the acetabular component.
Bone Scans
All patients with metastases should undergo technetium nuclear bone scanning (Fig. 6.4) for the existence of other lesions in the same or other bones because lesions in the other long bones may be exposed to increased stress from having to bear greater amounts of weight in the early postoperative convalescence. Identifying other lesions at risk of fracture may lead to earlier intervention to avoid the pain of fracture and the need for emergent surgery.
Blood Tests
Marrow suppression is common with metastatic disease. Anemia, thrombocytopenia, and neutropenia should be corrected or managed appropriately in order to minimize the potential for complications such as sustained postoperative hemorrhage, infection, and anemia. Post-chemotherapy nadir of blood elements is common and may occur up to 2 weeks after the last dose of chemotherapy. Certain cytotoxic agents are more frequently associated with anemia, thrombocytopenia, and neutropenia. Surgery should be considered after discussions
with the oncology team regarding the timing of normalization of blood counts. Renal function tests should be performed to exclude incipient renal failure and to correct any pre-renal cause of dysfunction such as dehydration. Liver function tests give an indication of the patient’s nutritional state which will have an impact on postoperative healing. Further, liver dysfunction may be associated with coagulopathy that may have a detrimental impact on surgery.
with the oncology team regarding the timing of normalization of blood counts. Renal function tests should be performed to exclude incipient renal failure and to correct any pre-renal cause of dysfunction such as dehydration. Liver function tests give an indication of the patient’s nutritional state which will have an impact on postoperative healing. Further, liver dysfunction may be associated with coagulopathy that may have a detrimental impact on surgery.
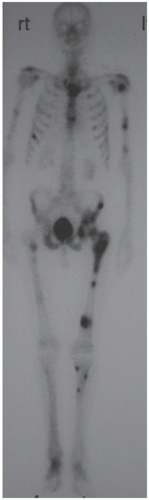 FIGURE 6.4 Technitium nuclear bone scan demonstrating widespread skeletal metastases in a 66-year-old man with metastatic pulmonary carcinoma. |
Pulmonary Function Tests
Pulmonary function tests should be performed on all patients with significant pulmonary metastases to determine if there is sufficient pulmonary reserve to undergo surgery and to withstand the effects of pulmonary embolic phenomenon.
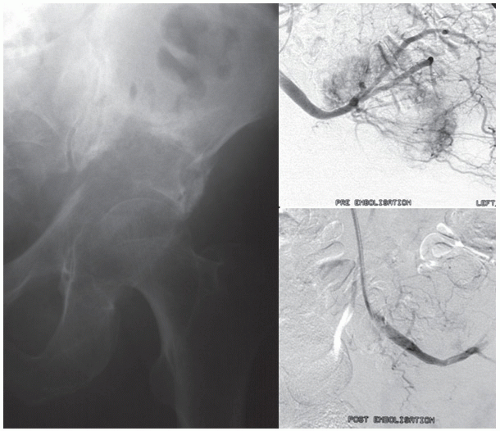
Angiography and Embolization
Certain tumors such as renal and thyroid carcinoma can give rise to hypervascular metastases (Fig. 6.5). All tumors, however, are capable of torrential bleeding. As pelvic tumors can be very large, and with feeding vessels arising directly from the iliac system, preoperative angiography is recommended to identify tumors, which have a high risk of bleeding. These can then be embolized between 24 and 36 hours prior to surgery (Fig. 6.5). Delays >72 between embolization and surgery may allow recanalization of embolized vasculature, thus negating the benefit of preoperative embolization.
MULTIDISCIPLINARY TEAM CONSULTATION
The safe management of an oncology patient who is to undergo periacetabular reconstruction requires active input from a variety of teams. These include the internal medicine team who should stabilize and optimize the patients’ reversible comorbidities. The oncology team should provide guidance on the timing of surgery and the postoperative chemotherapy. The anesthetic team needs to familiarize themselves with the patient’s cardiopulmonary, hematological, and electrolyte status as well as any factor in the patient’s history that will have an impact on the anesthetic technique to be employed.
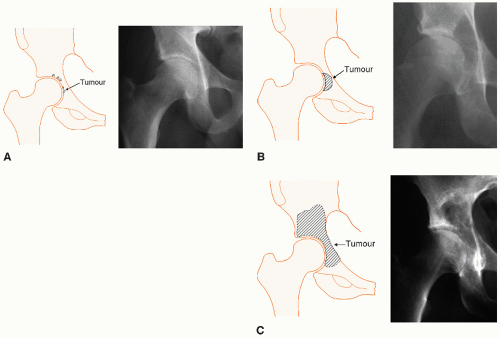
CLASSIFICATION OF ACETABULAR DEFECTS
Classification systems provide a means of standardizing communications between different practitioners (1,2). This is important because of the complexities of such cases, which may benefit from referral or consultation between practitioners. A good classification system accurately describes the pathology, which in the case of periacetabular metastases is the position and extent of acetabular destruction, provides a gradation of severity,
and guides the use of specific techniques depending on the grade of disease. The Harrington classification system is a four-grade system which has enjoyed much popularity (1).
and guides the use of specific techniques depending on the grade of disease. The Harrington classification system is a four-grade system which has enjoyed much popularity (1).
Type I defects are characterized by an acetabulum with intact anterior and posterior columns, superior dome of the acetabulum, and medial wall with only punctuate disease of the floor of the acetabulum (Fig. 6.6A).
Type II defects are characterized by loss of the medial wall with potential or true migration of the acetabulum medially into the pelvic cavity (Fig. 6.6B).
Type III defects are the most challenging because of destruction that involves the medial wall, lateral margin, and superior dome of the acetabulum (Fig. 6.6C). One or both columns are often involved too.
Type IV defects are rare, and were originally classified as solitary lesions that were amenable to en-bloc resection with a curative intention.
TECHNIQUE
Intraoperative Monitoring
Appropriate intraoperative monitoring is required to determine the stability of the patient under anesthesia as well as to rapidly identify changes in the patients that may signal deterioration in their well-being. Invasive monitoring with central venous catheterization allows measurement of right heart performance, while an arterial line permits accurate blood pressure recording. Expiratory carbon dioxide monitoring in conjunction with endotracheal anesthesia will permit an assessment of right to left shunting in the event of cardiopulmonary. Temperature monitoring is important to minimize body cooling that may impact myocardial function. A urinary catheter with a burette should be employed to provide accurate fluid output measurements.
Anesthetic
Postoperative pain management may begin prior to surgery with the insertion of an epidural catheter to allow intraoperative and postoperative instillation of anesthetic. Combining regional anesthesia with a general anesthesia may also allow a lighter general anesthetic to be used. Regional anesthesia alone may be considered safer in patients with pulmonary dysfunction. However, if cardiopulmonary collapse is anticipated, it may be argued that it would be safer to have in position secure endotracheal access from the beginning of the case rather than to attempt an urgent intubation in the middle of surgery with the patient in the lateral position.